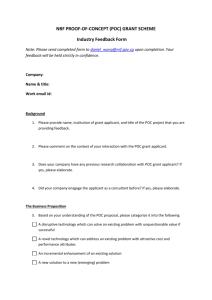
Client Name Quarter: Q1 Q2 Q3 Q4 MEDICAL RECORDS AND
advertisement
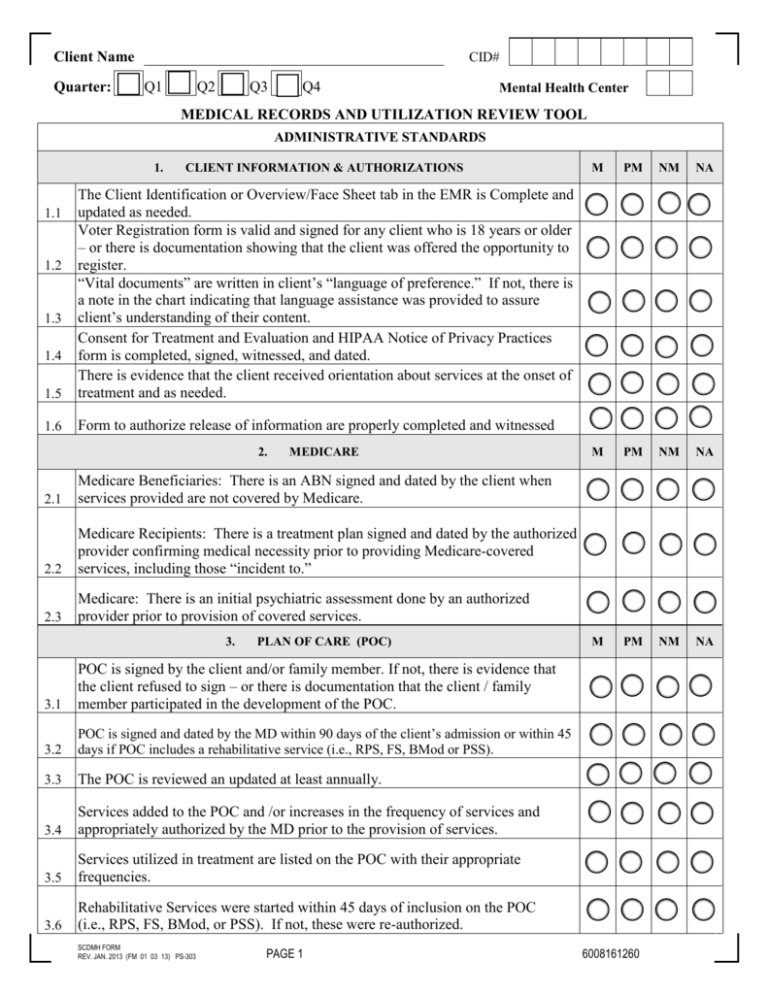
CID# Client Name Quarter: Q1 Q2 Q3 Q4 Mental Health Center MEDICAL RECORDS AND UTILIZATION REVIEW TOOL ADMINISTRATIVE STANDARDS 1. CLIENT INFORMATION & AUTHORIZATIONS 1.5 The Client Identification or Overview/Face Sheet tab in the EMR is Complete and updated as needed. Voter Registration form is valid and signed for any client who is 18 years or older – or there is documentation showing that the client was offered the opportunity to register. “Vital documents” are written in client’s “language of preference.” If not, there is a note in the chart indicating that language assistance was provided to assure client’s understanding of their content. Consent for Treatment and Evaluation and HIPAA Notice of Privacy Practices form is completed, signed, witnessed, and dated. There is evidence that the client received orientation about services at the onset of treatment and as needed. 1.6 Form to authorize release of information are properly completed and witnessed 1.1 1.2 1.3 1.4 2. MEDICARE 2.1 Medicare Beneficiaries: There is an ABN signed and dated by the client when services provided are not covered by Medicare. 2.2 Medicare Recipients: There is a treatment plan signed and dated by the authorized provider confirming medical necessity prior to providing Medicare-covered services, including those “incident to.” 2.3 Medicare: There is an initial psychiatric assessment done by an authorized provider prior to provision of covered services. 3. PLAN OF CARE (POC) 3.1 POC is signed by the client and/or family member. If not, there is evidence that the client refused to sign – or there is documentation that the client / family member participated in the development of the POC. 3.2 POC is signed and dated by the MD within 90 days of the client’s admission or within 45 days if POC includes a rehabilitative service (i.e., RPS, FS, BMod or PSS). 3.3 The POC is reviewed an updated at least annually. 3.4 Services added to the POC and /or increases in the frequency of services and appropriately authorized by the MD prior to the provision of services. 3.5 Services utilized in treatment are listed on the POC with their appropriate frequencies. 3.6 Rehabilitative Services were started within 45 days of inclusion on the POC (i.e., RPS, FS, BMod, or PSS). If not, these were re-authorized. SCDMH FORM REV. JAN. 2013 (FM 01 03 13) PS-303 PAGE 1 M PM NM NA M PM NM NA M PM NM NA 6008161260 4. CLINICAL SERVICE NOTES 4.1 There is a charge for each legitimate service rendered. 4.2 There is documentation for each service billed. 4.3 Bill times in service notes match actual time billed. 4.4 Dates in service notes match dates they were billed. 5. 5.1 5.2 5.3 5.4 5.5 5.6 MEDICAL STANDARDS M PM NM NA M PM NM NA M PM NA Non-Medicare Recipients: The initial PMA was provided by a physician within 90 days of admission or on the first service thereafter. Medicaid Recipients: There is a PMA rendered by the MD before an APRN delivers a PMA. MMO: There is a PMA rendered by the MD assigning client to this level of care. MMO: There is an annual assessment conducted by the MD or APRN to determine continuation of services at this level of care. If done by the APRN, it is co-signed by the MD. MMO: PMO or CSN must contain the following: a. intervening services since the last PMA b. assessment of whether client is meeting the goal (s) c. indication of changes in goal (s) d. verbal agreement to continue MMO e. justification for treatment. MMO: Clients’s progress and any significant changes in treatment are documented by the MD, APRN, or RN every 90 days or on the first contact thereafter if client was not seen in the quarter. 6. MEDICAL RECORDS 6.1 When required, all clinical documents in the medical record are signed/ co-signed, dated by clinician(s), and include their license and/or degree. 6.2 Abbreviations used on clinical documents are included in DMH/Center approved Abbreviations List. CLINICAL STANDARDS 7. CLINICAL ASSESSMENT 7.1 Initial Clinical Assessment (ICA) was thoroughly completed within three nonemergency visits. 7.2 Primary clinical assessment provides sufficient and appropriate clinical information to justify the diagnosis according to DMS criteria. SCDMH FORM REV. JAN. 2013 PS-303 PAGE 2 5029161262 NM CID# 8. PLAN OF CARE (POC) 8.1 Transition or Discharge plan is individualized and relevant. 8.2 Treatment goals are expressed in the client’s (family member or guardian, if appropriate) own words. 8.3 Objectives are written in a way that is understandable to the client based on his/her development and age. 8.4 Objectives address symptoms/behaviors, including those of co-occurring disorders, as identified in clinical assessments. 8.5 Objectives are outcome oriented: that is, desired, observable and measurable behaviors which, once mastered, would lead to achievement of overall treatment goals. 8.6 Objectives are achievable. 8.7 Objectives are time-specific. 8.8 Treatment interventions are specific and relevant to the treatment objectives. 9. CLINICAL SERVICE NOTES 9.1 CSNs include all of the following elements: a. focus of the intervention (activities, if Rehab groups) that are directly related to a goal / objective on the ROC. b. clinician’s interventions c. client’s response to clinician’s interventions d. client’s general progress in relation to treatment e. plan for next session. 9.2 Service Plan Development notes reflect MD and MHP/RN involvement in a. development, staffing, review, and monitoring of POC or b. review of outcome data as it impacts diagnosis, treatment, discharge plans, and focus of types of services, or c. confirmation of medical necessity, or d. establishment of dx, and MD recommendation (s) 9.3 9.4 M PM NM NA M PM NM NA All services are provided by qualified providers. Documentation in clinical notes supports services billed. 9.5 Documentation in CSNs/PMOs, including referenced documents, supports bill time. 9.6 No “non-billable” services were billed (e.g. socialization and recreational activities) without a clear therapeutic justification. SCDMH FORM REV. JAN. 2013 PS-303 PAGE 3 5778161263 CID# 10. TREATMENT PROCESS M PM NM NA M PM NM NA M PM NA 10.1 There is evidence of follow up when client misses an appointment. There is evidence of inclusion of a family member in treatment for ongoing 10.2 support, when clinically indicated. 10.3 There is evidence treatment focuses on integration of client into the community. 10.4 Progress Summaries are documented every 90 days after admission. Progress Summary Note includes: a. review of appropriateness of services and their frequencies b. review of the client progress on each objective and goal c. justification for continued treatment 10.5 d. recommendation(s) for continued services 11. UTILIZATION REVIEW 11.1 There is documentation to justify services as medically necessary. Services and their frequencies, as planned, are appropriate based on diagnosis, 11.2 needs, and strengths. 11.3 Services are provided within the maximum frequency authorized on the POC. The frequency and intensity in which services are delivered are appropriate to treat 11.4 the client based on diagnosis, needs, and level of functioning The clinical interventions effectively treat, relieve, or improve client’s symptoms, problems, and behaviors OR, in the case of clients who are stable, interventions 11.5 preserve current functioning and/or prevent decompensation. 12. MEDICAL SERVICES The Neuroleptic Consent Form is signed and dated by client or guardian and the prescribing authority when client is prescribed a Neuroleptic or atypical 12.1 antipsychotic medication. The presence of abnormal movements is assessed and documented at the initiation of treatment and thereafter every 6 months when the client is prescribed 12.2 antipsychotic medications. Medication Administration notes include: a. the name of the medication administered b. dosage given (quantity and strength) c. route (IM, ID, IV) d. injection site 12.3 e. side effects or adverse reactions noted SCDMH FORM REV. JAN. 2013 PS-303 PAGE 4 9458161262 NM CID# 12. PLAN OF CARE (POC) M PM NM NA M PM NM NA Medication-monitoring notes include: a. the name of the medication (s) client is taking or refers to PMO where medications are listed b. side effects or adverse reactions experienced 12.4 c. whether client is refusing or is unable to take medication (s) as order or if compliant in taking medications as prescribed d. effectiveness of medications in controlling symptoms e. issues relating to co-occurring substance use 13. DISCHARGE/TRANSITION PLAN Discharge/transition plan include all of the elements listed: a. date of admission b. services provided c. presenting condition 13.1 d. extent to which established goals and objectives were achieved e. reasons for discharge f. status of the person served at last contact g. recommendations for services or supports h. date of discharge from program COMMENTS Standard Issue Auditor’s Initials and Date: SCDMH FORM REV. JAN. 2013 PS-303 PAGE 5 0634161269