Severe Psychotic depression
advertisement

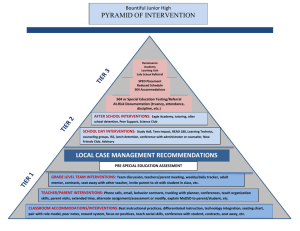
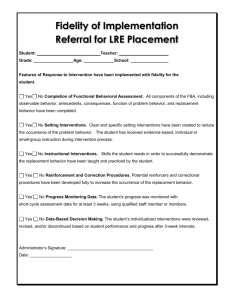
Cluster 15 Care Pathway for Sever Psychotic Depression This group of patients will be suffering from an acute episode of moderate to severe depressive symptoms. Hallucinations and delusions will be present. It is likely that this group will present a risk of suicide and have disruption in many areas of their lives. Diagnosis:- Likely to include: F 32.3 Severe depressive episode with psychotic symptoms. Structured Assessment · Comprehensive MDT assessment of Health and Social Care needs including a detailed physical, social, mental health and risk assessment. Care should be given to safeguarding/childcare and vulnerability issues. (eg Morgan assessment tool) · Assessment to identify current coping strategies for managing distress and dealing with difficulties. · Assessment to understand the emotional impact of symptoms and individual experiences · Comprehensive carer’s assessment including the emotional impact of condition and dealing with stressful situations. Please refer to detailed ‘Notes for Structured Assessment’ on the back Enabling and Implementing Interventions The ‘Core’ interventions will include: · Develop a care plan in line with the Trust CPA policy. · All Inpatients will be offered a Recovery tool (STAR) Organisational Guide, User Guide · Provide patient information leaflets . Medical intervention for symptom control, risk and crisis management. . Medical and Nursing interventions to maximize physical health, maintain current physical health and prevention of worsening or slowing of physical health condition · Medical Intervention such as Prescribing . Social interventions to promote better adjustment to situation, return to previous best level of social role functioning, significant improvement in quality of life and prevention of worsening or slowing of condition. The ‘supplementary’ interventions will include: · Specific psychosocial interventions in relation to the condition for the patient and their family. · Metabolic monitoring in line with Trust guidelines. · Occupational therapy assessment to explore range of occupational interventions. . Psychological intervention for symptom reduction and crisis management . Crisis intervention/admission / use of Mental health Act Assessment as necessary. For details of Core and supplementary interventions please refer to ‘Notes on Enabling and Implementing interventions’. For condition specific interventions please refer to ‘Notes on Enabling and Implementing Services provided by LPT Services provided by Mental Health Social Care Team Services provided by 3rd Sector agencies Services provided by primary health care Review · Regular review- CPA or non-CPA, relating back to goals set in care plan. · HoNos (PBR)- Guidance tool · Review cluster once every 4 weeks Please refer to detailed notes for ‘Review’ on the back for further information Sustained Improvement . Wellness recovery action plan links into service user self help groups. . Average duration of episode is 8 to 12 weeks Please refer to detailed notes for ‘Sustained Improvement’ on the back for further information Detailed Notes Notes for Structured Assessment All assessments will be person centred, holistic and multidisciplinary. Consideration to be given to additional assessment for comorbid conditions like Personality Disorder, Learning Disabilities, Deliberate Self-harm etc. Consideration to be given to Capacity, Deprivation of Liberty and Mental Health Act( if appropriate) Where appropriate, consider issues of sexual health and pregnancy in women including prescribing in pregnancy. Utilise assessment tools which may include Recovery star and HoNos. Physical Healthcare Assessment Consider setting up prospective review date. Notes for Enabling and Implementing Interventions Core interventions to include significant reduction of symptoms, prevention of worsening or slowing of condition, crisis management, reducing risk of harm to self and others.The purpose of interventions will be to prevent relapse, maximise role functioning or maintain current social role functioning, reduce risk of self-harm and promote better adjustment to situation. These interventions will involve on-going assessments, enabling and monitoring by lead professional, medical staff, psychologist, nursing and support staff as guided by the principles of Care Programme Approach (CPA). Under CPA provisions provide hope, information about cluster, diagnosis, pathway and services. Coordination is crucial to holistic care that fits with individual needs and makes efficient and effective use of social resources, consider referral to Wellbeing social inclusion team. Promote development of patient centred aims for recovery. Develop contingency and crisis plans. Swift response in mental health crisis in order to minimize risk to self and to others. Ensure provision of risk management training for staff. Pharmacological management including medication/ side effect monitoring and ECT (as clinically indicated). Psychological intervention including brief solution focused therapy, Psycho-education, CBT informed intervention, Supportive therapy, Interpersonal therapy, compliance therapy. Provide provisions to deliver swift and immediate response to vulnerable adults, child/adult safeguarding and ensure sexual safety of vulnerable females on ward. Gender, ethnic and communication specific support as needed e.g. sexual health, language interpretation. As appropriate advise / sign post/ access self-help (e.g. groups), self monitoring (e.g. triggers, ? signs), health promotions e.g. smoking cessation, exercise, harm minimisation for substance misuse, activity scheduling, diet, sleep, social support, work patterns, coping strategies, and activities of daily living etc. Provide finance/ benefits, debt reduction and specialist advice. Consider use of befriending and training volunteers. Assess accommodation needs. Provide on-going accommodation monitoring/support as necessary. Identify and inform carers/family at earliest opportunity. Provide support to carer’s, friends and family of service users. Also provide information of self help support groups. Consider family interventions e.g. psycho education, offer carer’s assessment. Liaise with 3rd Sector agencies to address socio-economic needs. Use Recovery STAR tool. Specific Therapeutic Interventions: Severe depression with Psychotic symptoms: Augment treatment with antipsychotic medication. Consider inpatient treatment for those with high suicide/self harm risk, offer full range of high intensity psychological intervention. ECT only for rapid and short-term improvement of severe symptoms after other treatments have proved ineffective or if the condition is life-threatening. Consider medication for severe behavioural disturbance. After crisis episode consider individual structured psychological interventions, include psycho-education and coping skills, circa 16 sessions over 6-9 months. NICE guidance on managing disturbed/violent behaviour in in-patient settings: De-escalation; Rapid tranquilization (Trust guidelines); Physical intervention; Seclusion For older people consider lower dosage medication, co morbidities and drug interactions. Work through de-escalation process if necessary. Follow LPT Trust guidance on rapid tranquilization if necessary Self-harm: Treatment for physical effects of harm. Appropriate harm minimisation strategies. If some substance/alcohol abuse - consider cluster 16, Dual diagnosis. Otherwise offer psychosocial intervention targeted at the abuse, delivered by general mental health services, with specialist substance use service support as appropriate. Notes for Review Goals identified in care plan are agreed with client and actions planned towards achievement. Improvement in social functioning including links with 3rd sector Promote self esteem and empowerment, maintenance of employment. Greater understanding/ stabilisation of symptoms and increased ability to manage self and symptoms, developing awareness of life skills. Provide information on stress management and develop Stress vulnerability plans. Finalise after care plan incorporating goal setting, crisis / contingency planning, provision of advocacy service and advance statement. Carer’s assessment and support. Feedback from patient’s carers on sustained improvement. Review of clustering/crisis at least every 4 weeks, or more frequent in inpatient setting if need/circumstances make this sensible. Make necessary arrangements for 7 day follow-up after discharge. Referral to Assertive Outreach team in case of poor engagement. In case of deterioration consider re-clustering. Notes for Sustained Improvement Identify patient’s awareness of their own symptoms and management by their willingness to engage with CRHT in a crisis or come into hospital on an informal basis if required/appropriate. Feedback from patient carers Support 3rdo sector and links with support groups Support from statutory services. CPA review PSA 16- Vocational and accommodation outcomes.