Respiratory Exam
advertisement

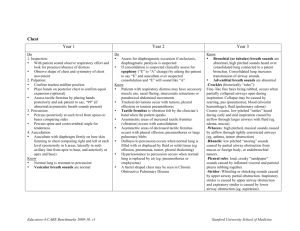
Student Bedside Medicine Respiratory Case A young man wonders about his chest Inspection Pectus Excavatum Pectus excavatum “funnel chest”: oval pit near the infrasternal notch or a more extensive concavity Isolated, Noonan, Marfan, rickets, tracheomalacia, bronchomalacia, congenital heart disease (including mitral valve prolapse) Case A young man with an abnormal sternum. Sternum protrudes from a narrowed thorax. Isolated, familial, Marfan, Noonan, rickets, acromegaly, anomalies of the diaphragm. Pectus carinatum “pigeon breast” Palpation Lung Expansion The diseased side moves less well than the less diseased. Fremitus German: “neun und neunzig”. The “eu” diphthong was important - not the number “99” we are taught! We need English sounds with “eu” like “toy” or “boy”. Press entire base of palm and fingertips against the chest to feel vibrations. Fremitus “toy” or “boy” Increased Consolidation or mass with an open airway. Decreased Obstructed airway, pleural effusion, pleural scar, pneumothorax Chest Percussion Leopold Auenbrugger - Austria Wine-cask fullness 1761 Latin treatise on percussion with four fingers of one hand to detect pleural effusion, which was ignored. Chest Percussion 50 years later the work was “rediscovered” by Corvisart (Napoleon’s physician) who made direct percussion a widely popular exam maneuver. Indirect percussion 1828 Special hammers and plates were developed. As equipment was lost, physicians used their fingers. Flat part of reflex hammer is often better than the finger of the other hand. Percussion notes Clinically important ones! Dull - Medium pitch/intensity Resonant - Low pitch, loud Hyperresonant/tympanitic - Lowest pitch, louder Indirect percussion Sides of posterior chest are compared. Primarily intended to screen for pleural effusion. Mass/consolidation may be detected. Pt needs to be sitting up Dull Resonant Tympanitic Auscultatory Percussion Described soon after the stethoscope was invented and popularized over the years for various organs. Sound is generated by fingers (tapping, flicking, scratching) and detected with stethoscope; sound changes pitch and loudness as it moves over density boundaries Auscultatory Percussion Stethoscope at lowest rib. Light tap or flick from above down. Sound gets louder and higher pitched right near stethoscope. With pleural effusion, sound change occurs higher. Easier than indirect percussion and possible on more frail patients. Auscultatory Percussion Sensitivity = 96%, Specificity = 100% for pleural effusion in one study. Superior to indirect percussion. False positives = elevated diaphragm. False negatives = small effusions in patients recumbant for hours. Sound change over effusion Rene Laennec Summer, 1816: saw children tapping on ends of a log and listening at each end. Next day, rolled a notebook of paper up into a cylinder to listen to a woman’s chest. Heard the heart and lungs better than ever. Rene Laennec Began to experiment with materials and dimensions to optimize the listening. Settled on a wooden cylinder 1 foot long and 1.5 in. in diameter. Rene Laennec Three years of research resulted in “De l’Auscultation Mediate”. He coined the term “stethoscope” (inspector of the chest). Known as a “cylindromaniac” and was opposed strongly by the “percussionists” Corvisart. It took many years before the percussionists accepted ascultation. Lung Anatomy The reason why we must examine the posterior, lateral, and anterior chest. Can actually do it all from behind by going under the lifted arm. Lung Sounds Breath sounds are what we hear with our native ears as patient is breathing through the nose and mouth. Lung sounds are what we hear with the stethoscope and is the preferred terminology for describing the exam. Decreased Lung Sounds Diffusely decreased Poor effort, thick chest, diffuse obstructive or restrictive disease Locally decreased Local airway obstruction, effusion, mass, pneumothorax Vesicular Lung Sounds Soft, rustling, 3:1 inspiration to expiration ratio. These are the “normal lung sounds” heard over most of the lung periphery. 3 1 Bronchial Lung Sounds Bronchial, tracheal, tubular lung sounds. Louder, higher pitched, and prominent expiration. Heard anteriorly in normals over the trachea/main stem bronchi. 1 3 1 1 Bronchial Sounds Should only be heard in the upper, anterior, central chest in patients. Bronchial lung sounds heard anywhere else (where vesicular should be heard) are a sign of consolidation with an open airway. Adventitious Sounds Laennec heard and named various abnormal sounds which were later called “adventitious”. He called most of these some form of “rale” - French for “rattle”. Adventitious Sounds Laennec could not use the term rale at the bedside. It reminded patients of the phrase “le rale de la mort” (the death rattle) and made him unpopular with the patient and family! Tuberculosis was rampant and Laennec died of TB in 1826 at the age of 45. Adventitious Sounds Laennec developed a synonym for rales: rhonchus. Rhoncus in Latin meant “rattle” and in Greek meant “snoring” and patients and families did not know what it meant. However, the English who studied Laennec’s work didn’t know what these terms meant either and they got everything confused. Further Term Confusion Laennec French Rale muquex ou gargouillement Rale humide ou crepitation Rale sibilant sec ou sifflement Rale set sonore ou ronflement Later English Coarse rale Fine rale, crepitation Sibilant rhonchus Sonorous rhonchus American Thoracic Society -1977 “Every physician seems to have his own classification” British/American investigations resulted in new published nomenclature that was supposed to get everyone communicating more clearly. Adventitious sounds: “continuous” if long (>250 msec) “discontinuous” if short (< 250 msec) Continuous Adventitious Sounds Wheeze Stridor Rhonchus Late inspiratory squeak Wheeze Musical, higher pitched; hissing, squeaking, whistling Indicates bronchiolar obstruction Expiratory before inspiratory Wheezing Inspiratory and expiratory: worse disease than expiratory alone. Stridor A hiss, whistle, or shriek; very similar to a wheeze. Better heard over upper sternum. Indicates upper airway obstruction either inside or outside the thorax . Stridor The obstruction closest to the beginning of the airflow movement creates the most noise Inside thorax = expiratory stridor Above thorax = inspiratory stridor Stridor Inspiratory stridor (upper airway obstruction above thorax) should not be confused with wheezing. Inspiratory wheezing would always be accompanied by expiratory wheezing. Rhonchus Lower pitched, polytonal, usually expiratory sound A snoring, gurgling, bubbling sound. Indicates expiratory collapse or secretions of/in larger bronchi. Rhonchus Inspiratory Squeak Late inspiratory “squeak” should not be confused with a wheeze because an inspiratory-only wheeze should not exist. Heard in pulmonary fibrosis, allergic alveolitis, and BOOP Rhonchi Squeak Discontinuous Adventious Sounds Crackles Fine Coarse Fine Crackles High pitched, mid-to late inspiratory; usually over dependent parts of lung; not changed by cough or position Like locks of hair rubbed by your ear Fine Crackles Coarse Crackles Lower pitched, longer, louder “popping sound”; early inspiration and/or expiration; any lung region; change with cough Like Velcro pulled apart Coarse Crackles Crackles Normals may have a few fine crackles over lower lobes with deep breathing. Fine crackles: left heart failure, pulmonary fibrosis, asbestosis, granulomatous infections Coarse crackles: bronchopneumonia, bronchitis, bronchiectasis Coarse Crackles Pure pneumonia may have no crackles at all. Any crackles should be coarse, reflecting the bronchial component. Pleural Rub Loud and creaky as two inflamed pleural surfaces rub; confused with rhonchi or coarse crackles; often highly localized Lower pitch, loudest during inspiration which helps distinguish it from rhonchi. Egophony “Goat sound”: any spoken vowel (usually “E”) is transmitted through the lung to the overlying chest wall as a nasal “ay” The change may be subtle Most sensitive sign of consolidation; occasional false (+) with patchy fibrosis Absent Present Egophony Consolidation Signs Increased tactile fremitus Bronchial (tubular) lung sounds Egophony (most sensitive) Whispered pectoriloquy and bronchophony are worse than egophony and can be skipped. Consolidation Signs If a dense infiltrate is clearly present on imaging, but there are no bronchial lung sounds and no egophony: Worry about a closed airway (mucus plug, tumor). Pleural Effusion Dullness to percussion Elevated dullness boundary by AP Decreased lung sounds Layer of consolidation findings over effusion (due to atelectasis) Occasionally, consolidation findings may be more generalized over effusion. END