8. Action Potential
advertisement
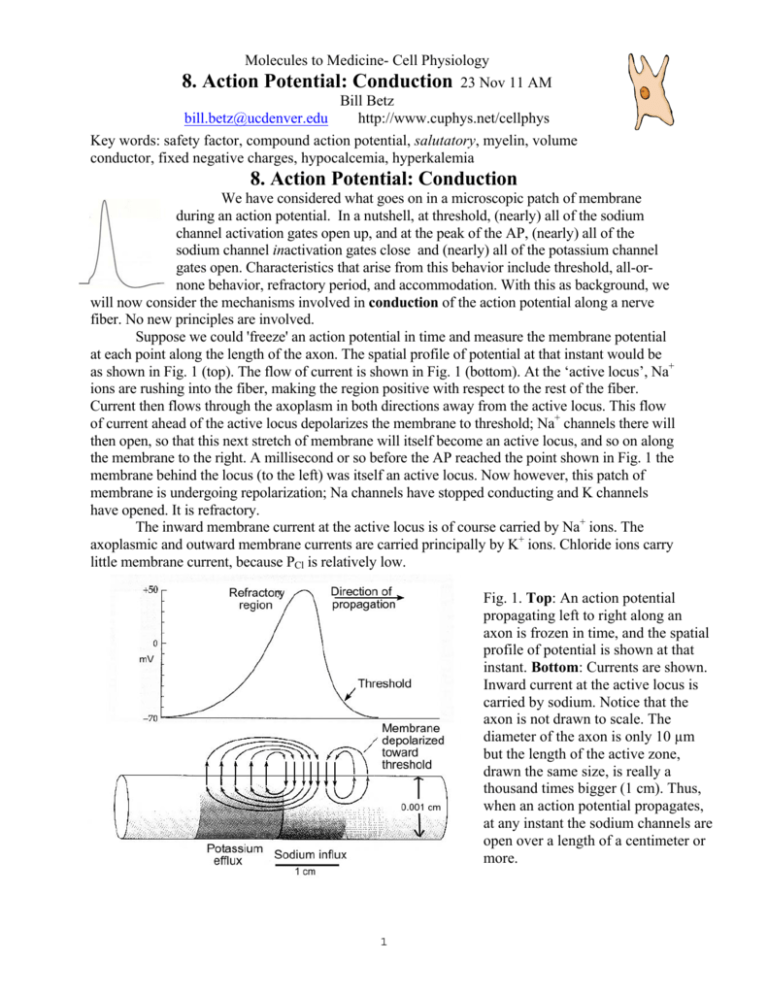
Molecules to Medicine- Cell Physiology 8. Action Potential: Conduction 23 Nov 11 AM Bill Betz bill.betz@ucdenver.edu http://www.cuphys.net/cellphys Key words: safety factor, compound action potential, salutatory, myelin, volume conductor, fixed negative charges, hypocalcemia, hyperkalemia 8. Action Potential: Conduction We have considered what goes on in a microscopic patch of membrane during an action potential. In a nutshell, at threshold, (nearly) all of the sodium channel activation gates open up, and at the peak of the AP, (nearly) all of the sodium channel inactivation gates close and (nearly) all of the potassium channel gates open. Characteristics that arise from this behavior include threshold, all-ornone behavior, refractory period, and accommodation. With this as background, we will now consider the mechanisms involved in conduction of the action potential along a nerve fiber. No new principles are involved. Suppose we could 'freeze' an action potential in time and measure the membrane potential at each point along the length of the axon. The spatial profile of potential at that instant would be as shown in Fig. 1 (top). The flow of current is shown in Fig. 1 (bottom). At the ‘active locus’, Na+ ions are rushing into the fiber, making the region positive with respect to the rest of the fiber. Current then flows through the axoplasm in both directions away from the active locus. This flow of current ahead of the active locus depolarizes the membrane to threshold; Na+ channels there will then open, so that this next stretch of membrane will itself become an active locus, and so on along the membrane to the right. A millisecond or so before the AP reached the point shown in Fig. 1 the membrane behind the locus (to the left) was itself an active locus. Now however, this patch of membrane is undergoing repolarization; Na channels have stopped conducting and K channels have opened. It is refractory. The inward membrane current at the active locus is of course carried by Na+ ions. The axoplasmic and outward membrane currents are carried principally by K+ ions. Chloride ions carry little membrane current, because PCl is relatively low. Fig. 1. Top: An action potential propagating left to right along an axon is frozen in time, and the spatial profile of potential is shown at that instant. Bottom: Currents are shown. Inward current at the active locus is carried by sodium. Notice that the axon is not drawn to scale. The diameter of the axon is only 10 µm but the length of the active zone, drawn the same size, is really a thousand times bigger (1 cm). Thus, when an action potential propagates, at any instant the sodium channels are open over a length of a centimeter or more. 1 Now suppose we add a local anesthetic like novocaine to just the right side of the axon, just ahead of the active locus. The anesthetic blocks sodium channels, keeping activation gates from opening. The depolarization generated by the last active sodium channels might spread passively farther along the axon, but it would become smaller and smaller, so that if the anesthetic was applied to a long enough length of axon, any depolarization getting past the anesthetic block would not reach threshold, and the sodium channels there would not open, and the action potential would die. This is what happens when your dentist administers novocaine. Pain fibers in your tooth or gum may be firing action potentials like crazy, but they don’t get past the novovaine block and your brain remains blissfully ignorant of the licensed violence being committed in your mouth. (How long would the length of block need to be? To answer this, you need to remember the length constant of a typical axon – about 1 mm. The depolarization will fall to about one-third each length constant. So, several millimeters of blocked axon should do the job.) Safety factor. It should be clear that a crucial factor in normal conduction is the density of Na channels in each imaginary patch of membrane. There must be enough Na channels to supply enough current to depolarize the next bit of membrane to threshold. This is key to understanding action potential conduction. It turns out that axons have more than enough Na channels to do the job; their safety factor of transmission is 5-10 times the minimum required for successful propagation. Is this excess just a needless waste of Na+ channels? After all, for every Na channel that opens, the sodium-potassium pump must eventually pump several thousand ions. There are several good reasons for this apparent extravagance. First, axons branch, sometimes profusely. At each branch point, the safety factor for transmission is reduced: the membrane just before the branch must deliver sufficient current to depolarize both branches to threshold. A high safety factor insures that action potentials will spread down both branches of the axon. Another good reason for having a high safety factor concerns sodium channel inactivation. Immediately after an AP, the axon is refractory, in part because Na channel inactivation gates have not yet reopened. The absolute refractory period ends when enough inactivation gates have reopened to enable the axon to conduct again. This requires that a certain minimum number of inactivation gates must be open in each ring of membrane. That number will be reached sooner if there is an excess of Na channels in the membrane. The upshot of this is simply that the axon will be able to transmit AP's at higher frequency than if it had only the minimum number of Na channels required for propagation. Moreover, the velocity of propagation of the AP will be increased, because the excess Na channels will supply extra current, and so drive the ring ahead of the active locus to threshold quicker. Mini-problem set Action potential aerobics. Here are some questions to test your understanding. Answers follow the last question. 1. In a clinical neurological test, a nerve trunk is stimulated with a brief shock delivered transcutaneously in the forearm. In each axon that reaches threshold, how many action potentials are generated? 2. Backfiring: Why doesn’t a propagating action potential reverse direction? After all, when repolarization occurs (behind the active zone), Vm comes back to threshold. So, why isn’t a second AP generated, which would then propagate in the opposite direction? 3. An axon is stimulated simultaneously at two points separated by about 10 cm. How many action potentials are created? 4. Same as number 3. What happens when the two APs traveling towards each other collide? Does one win and the other stop? Do both stop? Do both pass on through? 2 5. An axon is perfused intracellularly with ECF, and is bathed in ICF (believe it or not, this experiment has been done, using the squid giant axon). The membrane potential, instead of being -70 mV, now is about +70 mV. Negative current is injected to drop Vm to about +40 mV. Does the axon fire an upside-down action potential? ANSWERS: 1. When an axon is stimulated, unless the stimulus is given exactly at one end, then two APs arise, and travel in opposite directions. There is no inherent directionality to the AP mechanism. 2. An AP doesn’t reverse direction because, looking backwards (like riding in the last car on a train and looking back), all one sees is refractory axon – the sodium channels are incapable of firing an AP immediately after the active zone passes. 3. Two stimulating electrodes on an axon will generate four APs, two of them traveling towards each other, and two traveling towards the ends. 4. When the two APs traveling towards each other collide, they annihilate each other. Why? Pretend you’re one of the APs, traveling down the axon. As you collide with the oncoming AP, all you see ahead of you is refractory membrane. 5. Reversing ICF and ECF, do you get an upside-down AP? If the membrane potential is +70 mV, what is the position of the inactivation gates in the sodium channels? They are all tightly closed, and they wouldn’t open unless Vm were made very much more negative (-70 mV or so). So there will be no upside-down AP. [This might lead you to ask, suppose in addition to switching solutions, we also inverted the membrane, like turning a sock inside-out? In that case, all membrane potentials would be positive, and all APs would indeed be upside-down.] Extracellular recording. Hopefully by now you are comfortable thinking about experiments involving measurement of membrane potential with an intracellular microelectrode. There are, however, no clinical tests involving the use of intracellular microelectrodes (they are technically too difficult), although many do involve extracellular recording techniques (e.g., EKG, EMG, EEG). Such records of course give less precise information than an intracellular recording, but they report simultaneously the activity of many cells, which can provide useful diagnostic information. Like intracellular recordings, extracellular recordings involve nothing more than measuring the potential difference between two electrodes. The ECF has a small but finite electrical resistance (which we have ignored previously), and a current flowing will produce a voltage drop across this resistance. That’s what extracellular recording electrodes detect. The currents are generated, of course, by action potentials. Extracellular signals are small (a few mV) in amplitude. Because extracellular recordings detect activity of many nearby axons, their amplitudes and shapes vary a lot. Some details of extracellular recording and stimulation are described in Appendix Ia, Ib, and Ic. Consider a typical recording from a nerve trunk, which may contain thousands of individual axons (Fig. 2). The external electrode will sample the activity from all of the fibers simultaneously (something which certainly is not possible with an intracellular micropipette). The result is called a compound action potential because it comprises many discrete units. Assume we stimulate the ulnar nerve where it enters the upper arm, and record extracellularly in the arm near the stimulating electrodes (Fig. 2, V1). The stimulating electrodes, like the recording electrodes, are extracellular. During the pulse, current flows between the stimulating electrodes; some of it will flow across the axonal membranes, and depolarize the axons. With pulses of low intensity, we record a small negative deflection. With further increase in stimulus strength, the size of the 3 recorded response grows; that is, the response is graded with stimulus intensity. This is certainly different from an intracellular recording where the action potential is an all-or-none event. The extracellular response is graded because the axons in the nerve trunk do not all reach threshold together. Some axons require a stronger stimulus than others in order to initiate an action potential. The more axons that fire, the bigger the response. We will return to this point shortly. Continuing the experiment, we move the recording electrodes much farther from the stimulating electrodes - say, down to the wrist - and stimulate again with increasingly strong shocks. Now, of course, the latency (i.e., the elapsed time between the stimulus artifact and response) is increased because the action potentials must cover a greater distance before reaching the recording electrodes (V2 in Fig. 2). As before, we find that the amplitude of the compound action potential is graded with stimulus strength. With strong shocks, however, an additional change in the response is observed: now a second, smaller bump is observed on Fig. 2. Superimposed extracellular recordings the tail of the first. In other words, the compound action from sciatic nerve. Stimuli were applied where potential is dispersed in time. The dispersion means nerve enters the thigh; three different stimulus strengths (top). Recordings were made from the simply that some axons conduct at a lower velocity than others and so reach the recording electrodes later than sciatic nerve in the thigh (V1) and at the ankle the fast action potentials. This dispersion wasn’t (V2). observed when the recording was made in the thigh because the fast conducting APs had not had time to outrun the slow ones. And the fact that the second peak (corresponding to the slowly conducting fibers) is seen only with relatively high stimulus strengths means that the slow fibers require a stronger stimulus to reach threshold than do fast fibers. So slow conduction velocity and high threshold (to external stimulation) go together. If we assume that the microscopic properties of all axon membranes are identical, we can explain this behavior on the basis of one very simple parameter: axon diameter. As we will see, small diameter fibers have a high threshold to (external) stimulation and conduct action potentials at a lower velocity compared to large diameter axons. In addition, they have a low safety factor for conduction. Let's take these three properties in turn. 1. Threshold to external stimulation. Small diameter fibers are harder to stimulate than large diameter fibers. The basic mechanism is described in Appendix Id. This difference in threshold to extracellular stimulation is useful in clinical tests. For example, the conduction velocity in peripheral nerves is measured during regeneration of damaged nerves (velocity increases as recovery proceeds). Such measurements are also useful in localizing compressive tumors or inflammatory processes (conduction velocity is reduced where a nerve trunk is compressed or inflamed). A potential practical problem arises because there are pain fibers in the nerve trunk, and if they are stimulated, the testing procedure can be very unpleasant for the patient. However, it turns out that pain fibers have small diameters. Thus the large diameter fibers (which include motor axons) can be selectively stimulated, and the testing procedure is relatively painless. 2. Safety factor. Small diameter fibers have a low safety factor for conduction of AP's. The quantitative analysis of the effect of axon diameter on safety factor is complex. However 4 complicated the explanation is, though, the fact is easy to demonstrate. For example, small diameter axons can be selectively blocked by a low dose of local anesthetic such as procaine. (The anesthetic works by blocking some of the Na channels.) Large axons, however, are spared. If you have ever had a laceration stitched up, you may have felt the skin being manipulated (large diameter "touch" fibers were still conducting), but felt no pain (small diameter pain fibers blocked by anesthetic). 3. Conduction velocity. Bigger is faster. Myelin is even faster. Through the course of evolution, organisms that could react quickly to changes in their environment had a strong selective advantage over their slower peers. Reaction time is limited, in the end, by the velocity of action potential conduction along sensory and motor axons. Two mechanisms have evolved to boost conduction velocity: axon diameter and myelin. We will consider these in turn. a. Axon diameter. Axons with big diameters conduct faster than axons with small diameters. The mechanism by which this arises is described in the Appendix. The biggest human axons are about 20 µm in diameter. The world record is held by the squid, which has an axon that may be over one millimeter (1000 µm) in diameter, and mediates the squid's escape behavior. Now that is a lot of space to devote to one cell. The human olfactory nerve is only a millimeter wide, yet contains more than 100,000 individual axons! Furthermore, the squid's response to natural selection reaches a point of diminishing returns, because conduction velocity depends on the square root of diameter, so that doubling diameter (which quadruples the volume) increases conduction speed by only 41%. b. Myelin. Vertebrates have evolved a novel specialization to increase conduction speed still further, namely myelin. Glial cells create the multiple layers of tightly packed myelin membrane that surround an axon, which increases the electrical resistance between the inside of the axon and the extracellular fluid, thereby reducing the leaky cable properties of the underlying axon membrane. The insulating sheath of myelin is interrupted every few millimeters, exposing the bare axonal membrane. This naked region is called a Node of Ranvier, and is the site where all of the voltage-gated sodium channels are localized (their tight packing may reach a density of several thousand channels per square micrometer of membrane); there are no sodium channels beneath the myelin. Thus, when a node of Ranvier is depolarized to threshold, Na+ channels in the nodal membrane open and the node becomes an active locus. The current then spreads effectively inside the axon through the internodal region to the next node, which becomes depolarized , and the process repeats, 'jumping' from node to node, a process called saltatory conduction (L. saltare, to jump). Myelination greatly increases conduction velocity; if the squid giant axon were myelinated its conduction velocity would increase by a factor of 100! Myelination also changes the quantitative relation between fiber diameter and conduction velocity; the relationship now becomes directly proportional so that doubling the diameter doubles the conduction velocity. Fig. 3. Myelin Parameters If fast conduction is so great, why aren’t all axons big? (There is a 100-fold range in human axon diameters (from 0.2 to 20 µm).) The explanation for the huge range in diameters lies in the 5 fact that there is not an unlimited amount of space or precursor materials in the body for axons; a compromise is struck between the need for speed and the need for content. The choice becomes whether to make all axons the same size, or make some big at the expense of others - one axon that can conduct at 90 m/sec takes up as much space as nine smaller axons that conduct at 30 m/sec. So for the sacrifice of several milliseconds in conduction time, an enormous increase in information content can be obtained - nine fibers can tell you a lot more than one fiber can. Furthermore, processing by the central nervous system (CNS) of information of any complexity requires a fair amount of time (tens of milliseconds), and supplying this information to the brain over 90 m/sec axons would be gross mismatching, because the long central computation time precludes a very rapid response. Thus, Nature has struck a balance between conflicting needs in the evolution of the nervous system, and the outcome is an efficient and economical compromise between speed and content. In the human nervous system, two of the most extreme examples of the speed vs content struggle are olfactory axons and muscle spindle afferent axons. The latter, which you will study later, convey feedback sensory information to the CNS from muscles, and play an important role in the fine tuning of movements. Such information is needed in a hurry by the CNS while one is, say, playing a Chopin scherzo on the piano, and muscle spindle afferents are the largest and fastest conducting of all axons (about 20 microns diameter, 100 m/s in velocity). On the other hand, responses to olfactory stimuli are not very rapid; the axons in the olfactory nerve are only about 0.2 µm in diameter, and so conduct slowly. However, there is enough space for about 100,000 olfactory axons in the olfactory nerve which, at about 1 mm diameter, is about the size of the squid giant axon. The net result is a very rich input to the CNS, but you cannot savor an odor in fifty milliseconds; you need more central computing time. Finally, if myelin is so great for increasing conduction velocity, why aren’t all axons myelinated? You may recall that, for nonmyelinated fibers, conduction velocity increases as the square root of diameter, whereas in myelinated axons, conduction velocity is proportional to fiber diameter. A graph of these relations is shown in Fig. 4. Notice that below a diameter of about one micrometer, the conduction velocity is faster in the nonmyelinated fiber (see Appendix If for details). Nature has discovered this by trial and Fig. 4. Axons with diameters below about error, and only the smallest axons (diameters less 1.0 µm are nonmyelinated. than one micrometer) in mammals are nonmyelinated. Acute Hyperkalemia and CBIGK. Let’s review one more time the physiology of acute hyperkalemia, and consider the role calcium ions as a treatment - the C in CBIGK. The causes are usually due to K+ escaping rapidly from cells (hemolytic anemia, crush accident, electrocution, severe infection). Acute hyperkalemia is most dangerous in the heart where the elevated extracellular potassium depolarizes cells, disrupting the rhythm of the master clock (in the S-A node) that triggers each beat of the heart. Normally, cells there, called pacemakers, undergo spontaneous depolarizations (see figure below), and when they reach threshold, they fire APs, which spread to the muscle fibers throughout the heart and trigger contraction. Hyperkalemia depolarizes these cells, disrupting the exquisite timing of the clock. New pacemakers - mavericks - 6 Normal pacemaker activity of the heart's master clock (S-A node). Cells there undergo spontaneous depolarization and fire APs when they reach threshold (about once per second). Abnormal depolarization of these cells by hyperkalemia can disrupt this pattern. can arise anywhere in the conduction system, disrupting the synchrony of muscle contraction, causing the EKG arrhythmias . The maverick pacemakers can be silenced by administering calcium ions, thereby restoring the normal synchronous pattern of excitation and contraction. How calcium ions exert this quieting effect on sodium channels is described in detail in Appendix II. In brief, the mechanism is unlike anything that we have discussed: calcium ions act by binding to fixed negative charges on the outside surface of cells and trick the sodium channels into thinking that the membrane has been hyperpolarized, thereby raising the threshold for action potential initiation. 7 APPENDIX I: Details of extracellular recordings and threshold a. Extracellular recording from a single axon. Consider a simple experiment: a single axon is dissected from a nerve trunk, and is gently laid across two widely separated (ca. 10 cm) electrodes (Fig. A1). An action potential is initiated with a stimulator (not shown) and propagates from left to right. The recordings can look very different, depending on the electrode arrangement (Fig.A3). Figs. A1 and A2. Extracellular recordings from a single axon. Action potential propagates from left to right (arrows). In Fig. A1 the nerve is in Ringers solution; in Fig. A2, part of the nerve is lifted into an insulating medium. In the first panel (Fig. A3), the response is very small - the individual bumps can barely be resolved above the background noise of the recording system. Matters are greatly improved if the axon is lifted out of the saline into an insulating medium, such as paraffin oil or moist air (Fig. A2); this gets rid of most of the short-circuiting effect of the saline; a thin film of saline will, however, cling to the axon and provide an extracellular current path). So you see right away that the amplitude of externally recorded signals depends a lot on the geometry of the external fluid. The negative deflection occurs as the active locus of the action potential passes the first electrode. When it passes the second electrode, the deflection is of course reversed in sign. Ordinarily, it is impractical to dissect such a long length (10 cm) of nerve; usually the recording electrodes are less than one cm apart. In such a case, the second wave overlaps the first, and a diphasic potential is recorded (Fig. A3, panel C). This adds a further complexity, because it now is difficult to know exactly what happens at each individual electrode because of the overlap of the two waveforms. So, in experimental studies, the action potential is usually blocked between the electrodes (by crushing the nerve, or by local cooling). Because the action potential never reaches the second electrode, the response is now a pure Fig. A3. Extracellular monophasic potential (Fig. A3, panel D). recordings of electrical activity in a nerve trunk. b. With extracellular stimulation, will depolarization occur at the negative or positive electrode? Answer: The axon will be depolarized at the negative electrode. As the negative electrode is moved close to the axon, it makes the outside of the axon negative at that point. Making the outside negative is equivalent to making the inside positive (it's the potential difference that matters), so an action potential is initiated at the cathode. c. When recording compound APs, why is it better to have the recording electrode far from the stimulating electrode? Answer: to give time for slow and fast conducting APs to separate in time. 8 d. Why do large axons have a lower threshold to extracellular stimulation than do small axons? A large diameter and a small diameter axon are placed near stimulating electrodes (Fig. A4). Current flows between the stimulating electrodes, mostly in the extracellular fluid (because of the low resistance). Some of the current will enter the axons under the positive electrode, flow through the axoplasm, and out of the axon at the negative electrode. The axon will be depolarized at the negative electrode. We can represent this situation schematically with two resistors: r1 (representing a ring of membrane under each electrode) and r2 (representing the internal resistance of the axon). Now r1 is inversely proportional to the axon diameter, but r2 varies inversely with the square of fiber diameter: r2 is proportional to 1/d2. The applied voltage V will be dropped across the 3 resistors arranged in series. We are interested in ΔV across the resistor, r1, under the cathode (when ΔV is large enough, the membrane will be depolarized to threshold). This is just a voltage divider, and the potential change across r1 is simply: Fig. A4. Left: spread of current between stimulating electrodes. Right: Schematic diagram of axon. r1 = resistance of a "ring" of membrane, r2 = internal resistance between "rings". Substituting the proportionate diameter values: where k is a constant of proportionality. Simplifying: Thus, as d increases, ΔVr1 will also increase. In other words, for a given stimulus, the potential change will be greater in a large diameter axon. e. What factors determine optimal myelin thickness, and optimal internodal distance? As shown in Fig. 3 (reproduced below), assume we have a fiber of constant thickness T (note that T = axon + myelin thickness). How much of the total diameter T should be devoted to axon, and how much to myelin, in order to maximize conduction velocity? As we increase axon diameter (keeping T constant), the internal resistance of the axoplasm of course decreases. This will increase conduction velocity. However, as axon diameter increases, the myelin thickness must be decreased in order to keep the overall diameter (T) constant. Thinner myelin will make the internode leakier, resistively and capacitatively, and this will reduce conduction velocity. Thus there will be a balance point between axon diameter and myelin thickness, and at this point conduction velocity will be maximal (for the given fiber diameter T). Purely theoretical considerations show that the axon diameter should be about two-thirds of the overall fiber diameter in order to achieve maximum conduction velocity. In real axons, as you might expect, the value falls between 60% and 80%. In other words, without recourse to theoretical considerations, 9 evolution has selected the optimum design for maximizing conduction velocity. Fig. 3 (reproduced). Myelin Parameters The optimum internodal distance is more complex, and depends on many factors. It turns out that internodal length is not too critical for conduction velocity, although, in general, large diameter fibers have longer internodal distances than do small diameter fibers. Usually, the length of fiber between nodes is about 100 times the fiber diameter (in human nerve, most nodes are separated by about 1-2 mm). Appendix II: Calcium and excitability To understand the basics of the cardiac arrhythmias, we need to know a little bit about how heart beats are triggered (details come next spring). In brief, there is a master clock in the wall of the right atrium that triggers each beat. The clock comprises a clump of connected cells (the sino-atrial (SA) node) that depolarize spontaneously (and synchronously). When they reach threshold, each fires one action potential. Axon-like processes carry the APs out to all of the muscle fibers, initiating muscle contraction (systole). In fact, a kind of backup system exists, because all cells in the cardiac conduction system depolarize spontaneously. It’s just that the ones in the SA node depolarize fastest and so get to threshold first, setting the overall tempo of beats. But the backups can make trouble during hyperkalemia. During hyperkalemia, the conduction cells are at risk. The depolarization moves Vm closer to threshold, making it easier to fire an action potential, but it also inactivates some sodium channels, making it harder to fire an action potential. Maverick pacemakers can arise for either reason. In the latter case (block of conduction), other pacemaker cells distal to the block will keep depolarizing spontaneously, and when they get to threshold, they will fire an AP. It’s bad news either way, because now these mavericks are driving part of the heart at a rate that is independent of the rest, and when heart muscle fibers don’t contract synchronously, the heart cannot pump blood effectively. If other maverick pacemakers arise, the situation can deteriorate rapidly, leading ultimately to ventricular fibrillation, a condition in which no blood is pumped. Calcium ions and excitability. Calcium ions are one of the most important intracellular signaling molecules in the body, participating in a bewildering variety of important cellular events, such as muscle concentration, cellular motility, bone deposition, and exocytosis. You will study these mechanisms in the months ahead. Ca++ is also important in governing the threshold for the action potential, which is the rationale for giving calcium when cardiac arrhythmias emerge during hyperkalemia. 10 How does calcium affect AP threshold? The key features are illustrated in Fig. A5, which shows the effects of extracellular Ca++ on the surface negativity of the membrane. By way of Fig. A5. Calcium ions screen fixed negative charges, increasing the membrane electric field (Vm). A. In the normal situation, some charges are screened, and the local Vm is -70 mV. B. If [Ca++] in the ECF increases, more charges are screened, and the local Vm hyperpolarizes to -80 mV, thereby moving farther from threshold for an AP. C. In hypocalcemia, more fixed negative charges are exposed, reducing the local Vm to -50 mV, leading to spontaneous AP generation. introduction to this arcane but important phenomenon, the outside surfaces of all plasma membranes are studded with fixed negative charges (they are negative headgroups of phospholipid molecules and also anionic carbohydrate residues bound to membrane proteins, including sodium channels -see cartoon to the right). These fixed negative charges make the outside of the membrane a little bit more negative than it would otherwise be, but the negativity is exceedingly localized in space – a tiny nanodomain near the membrane surface. For example, if a positive ion in the ECF approaches the membrane, it would not even begin to detect the presence of the fixed negative charges until it was within a few nanometers of the surface (less than the thickness of the membrane itself!). That's because all the other free ions and water molecules in the bulk ECF block its electrical 'view' of the fixed charges beyond this short distance. Membrane proteins, however, lie within the nanodomain, and thus ‘see’ that the outside of the membrane is made negative by the fixed negative charges. Making the outside of the membrane negative is equivalent to a depolarization. A microelectrode recording Vm would, however, never see this nanodomain. For example, in Fig. A5A, a microelectrode would record a Vm of -80 mV, but the ‘local’ Vm perceived by sodium channels and other membrane proteins is less, only -70 mV, owing to the unscreened fixed negative charges on the outside surface of the membrane. In summary, unscreened fixed negative charges reduce the electric field across the membrane, making it easier for sodium channels to start conducting. As shown in Fig. A5B, giving extra calcium ions screens naked fixed negative charges, hyperpolarizing the local Vm, making it more difficult for the cell to fire an action potential. The binding of calcium is entirely electrical; no special ‘receptor’ is involved. In summary, pacemaker cells in the conduction system of the heart are depolarized by the high [K+]o, and maverick pacemakers arise. Calcium ions administered intravenously bind to surface membranes, increasing the threshold for AP generation. The clinical hope, of course, is that the normal pacemakers will take over once again and restore the normal excitation of the heart muscle. 11