SBAR Resources
SBAR Resources
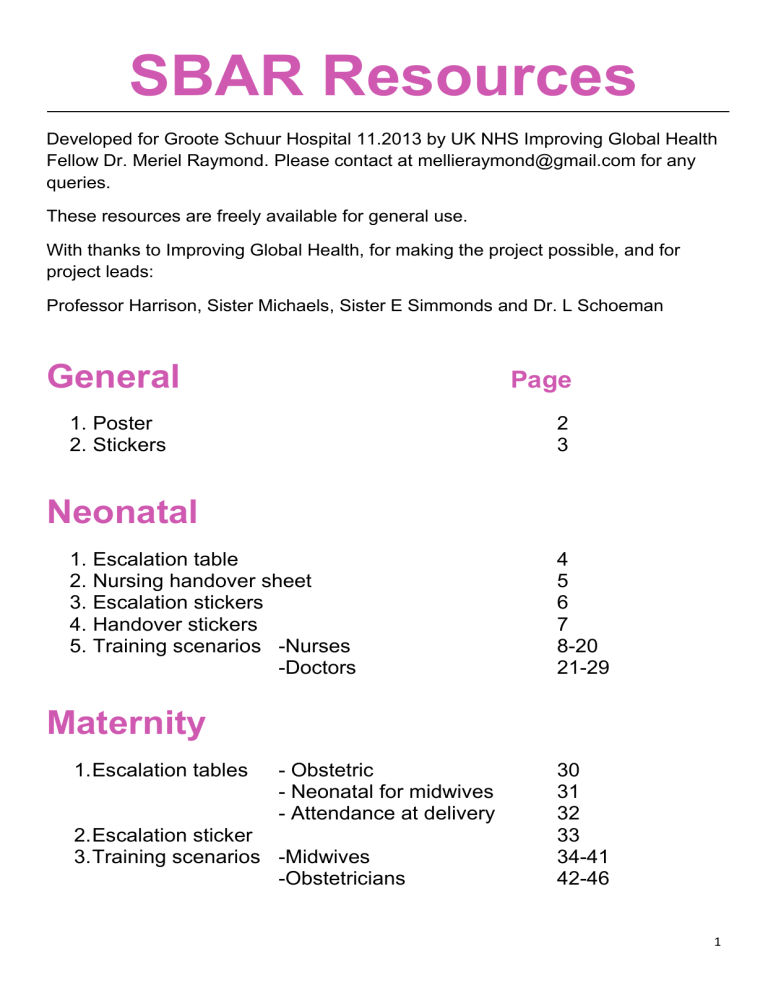
Developed for Groote Schuur Hospital 11.2013 by UK NHS Improving Global Health
Fellow Dr. Meriel Raymond. Please contact at mellieraymond@gmail.com for any queries.
These resources are freely available for general use.
With thanks to Improving Global Health, for making the project possible, and for project leads:
Professor Harrison, Sister Michaels, Sister E Simmonds and Dr. L Schoeman
General
Page
1. Poster
2. Stickers
2
3
Neonatal
1. Escalation table
2. Nursing handover sheet
3. Escalation stickers
4. Handover stickers
5. Training scenarios -Nurses
-Doctors
Maternity
1. Escalation tables - Obstetric
- Neonatal for midwives
2. Escalation sticker
- Attendance at delivery
3. Training scenarios -Midwives
-Obstetricians
4
5
6
7
8-20
21-29
30
31
32
33
34-41
42-46
1
2
3
Neonatal
Escalation SBAR
A 30-60 second report
Before calling the dr:
1. Assess the baby
2. Read most recent notes
3. Have chart in hand
S
B
A ituation ackground ssessment
R ecommendation
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about Baby Boy or Girl ____ who is ____ old
I’m calling because... the baby is blue, grunting, irritable, jaundiced, hypoglycaemic etc.
Include vital signs here in an emergency situation
The baby was admitted because of....
Gestation
Born via: C/S (give reason)
Maternal history
Problem list
Weight
NSVD
HIV Y/N very low birth weight, respiratory distress etc.
Forceps Ventouse Apgars:
Ventilation/O
2
:
Medications
Test results
Vital signs :
Intubated
Airway / Breathing
Circulation
RR
HR
CPAP Nasal cannulae
Oxygen Saturations
BP
___litres O
2
Temperature Blood Glucose
I think this patient might have .....
an infection, Hypoxic Ischaemic Encephalopathy, RDS etc.
Or: “I’m not sure what’s wrong with this patient, but I am worried”
I have already... increased the oxygen, put the baby on monitoring, started phototherapy etc.
I think this baby needs....
CPAP, intubation, antibiotics, review etc.
I think this needs doing within the next ____ mins/hrs/days
How often should I do observations? When shall I call you back if there is no improvement?
Can I repeat the plan back to you?
4
Neonatal SBAR Handover
Situation
Background
Assessment
This sheet is intended as a prompt for nursing handover
Name of patient
Location
Age
Current issues 1.
Reason for admission
Gestation
Weight
2.
3.
Delivery/Apgars
Maternal HIV
Problem list 1.
Y/N
2.
3.
Ventilation/O
2
:
Intubated CPAP Nasal cannulae
Medications
Test results e.g. TSB, Hb
Social issues
Vital signs
___litres O
2
-
Airway/Breathing Sats
-
Circulation
Likely diagnosis
BP
Target sats
Target mean BP
Temperature
RR
HR
Blood Glucose
Recommendation Tests e.g. repeat TSB/TCB/DXt
Treatment
Review Y/N in __mins/hrs
Care plan
Feeding
Discharge plan Transfer Y/N
5
Neonatal SBAR escalation/transfer sticker
Developed Neonatal Department, Groote Schuur Hospital 11.2013 by UK NHS Improving Global Health Fellow Dr. Meriel Raymond
Lead contact Sister Michaels karenmics@yahoo.com/ Prof Harrison mc.harrison@uct.ac.za
Name of patient
Location
Date & time of call
Situation Name/location of caller
Name of doctor receiving call
Age of baby
Presenting problem
Background
Assessment
Recommendation
Reason for admission
Gestation:
Born via:
Weight:
C/S (?reason) NSVD Forceps/Ventouse
HIV exposure Y/N Maternal history
Problem list
Ventilation/O
2
:
Medications
Intubated CPAP Nasal cannulae
Test results
Vital signs
Airway/Breathing
Circulation
Possible diagnosis
Sats
HR
Temperature
RR
BP
Blood Glucose
What does the caller recommend?
-Review Y/N in ____mins/hrs
-Tests
-Treatment
-Transfer ETD
Frequency of observations
When to call back
ETA
Repeat plan back
Apgars:
___litres O
2
6
Neonatal SBAR handover sticker
Developed Neonatal Department, Groote Schuur Hospital 11.2013 by UK NHS Improving Global Health Fellow Dr. Meriel Raymond
Lead contact Sister Michaels karenmics@yahoo.com/ Prof Harrison mc.harrison@uct.ac.za
Name of patient
Location
Date & time
Situation
Background
Assessment
Recommendation
Age
Current issues 1.
2.
3.
Reason for admission
Gestation
Weight
Delivery/Apgars
Maternal HIV
Problem list 1.
2.
3.
Y/N
Ventilation/O
2
Intubated
Medications
Test results
Vital signs
Airway/Breathing
Circulation
Sats
HR
CPAP
RR
BP
Nasal cannulae
Temperature Blood Glucose
Likely diagnosis
Tests
Treatment
Review
Feeding
Discharge plan
Y/N
___litres O
2
7
SBAR NEONATAL NURSE TRAINING
Written by Dr. Meriel Raymond, UK NHS Improving Global Health Fellow, in conjunction with the neonatal department at Groote Schuur Hospital, Cape Town
Contents:
1.
2.
3.
4.
Neonatal Escalation SBAR table
Case Scenario 1
Case Scenario 2
Case Scenario 3
5.
6.
Quiz answers
References and project lead contacts
7.
8.
Appendix 1 Neonatal SBAR escalation/transfer sticker
Appendix 2 Nursing/Doctors Neonatal SBAR handover sheet
9. Appendix 3 Neonatal Nurse/Doctors SBAR handover sticker
10. Pre-training quiz
11. Post-training quiz
12. Feedback sheet
8
S
B
A ituation ackground ssessment
Neonatal Escalation
SBAR
A 30-60 second report
Before calling the dr:
4. Assess the baby
5. Read most recent notes
6. Have chart in hand
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about Baby Boy or Girl ____ who is ____ old
I’m calling because the baby is..... blue, grunting, irritable, jaundiced, hypoglycaemic etc.
Include vital signs here in an emergency situation
The baby was admitted because of....
Gestation
Born via: C/S (give reason)
Maternal history
Problem list
Ventilation/O
2
: Intubated
Medications
Test results
Vital signs :
CPAP
Weight very low birth weight, respiratory distress etc.
NSVD Forceps
HIV Y/N
Nasal cannulae
Ventouse
___litres O
2
Apgars:
Airway / Breathing RR
Circulation HR
Oxygen Saturations
BP
Disability Temperature Blood Glucose
I think this patient might have..... an infection, Hypoxic Ischaemic Encephalopathy, RDS etc.
It is fine to say
“I’m not sure what’s wrong with this patient, but I am concerned” “I’m uncomfortable” “this is unsafe”
R ecommendation
I have already... increased the oxygen, put the baby on monitoring, started phototherapy etc.
I think this baby needs.... CPAP, intubation, antibiotics, review etc.
I think this needs doing within the next ____ mins/hrs/days
How often should I do observations? When shall I call you back if there is no improvement?
Can I repeat the plan back to you?
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
9
SBAR NEONATAL NURSE TRAINING SCENARIOS
Scenario 1 (Adapted from Institute for Healthcare Improvement, 2011)
Zechariah is a 3-week old infant in ICU. He was at 27 weeks gestation when born by vaginal delivery. The premature labour was thought to be brought on by chorioamnionitis. Apgars were 5, 9, 9. Maternal HIV and RPR were negative.
He received antibiotics in the first week of life, but there have been no signs of infection since then.
He has been progressing well after a short period of CPAP and remains in 24% flow support. He is receiving continuous tube feedings. Recently he has had some regurgitation of formula. He has demonstrated a steady weight increase, and currently weighs 1.5kg. He is on vitamins but not on any antibiotics.
For the first time today, he has had a couple of episodes of apnoea. When Sue, the evening nurse, came on and did her assessment she noted he was tachypnoeic with a respiratory rate of 75. As she was documenting her assessment, Zechariah had a bradycardic episode and his oxygen saturation decreased to 75. His heart rate returned to 130 with stimulation and Sue increased the oxygen to 28%. His saturations are now 92%. The blood glucose is 3.8. His muscle tone is diminished and his colouring is mottled. His abdomen isn’t distended. The day nurse reported that he had slept a lot today and his mother felt he wasn’t as alert as usual.
Exercise
The facilitator will talk through how to use the table to make a report to the doctor on-call.
Remember:
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
Ideal answers are overleaf but please don
’t cheat!
10
Neonatal
Escalation SBAR
A 30-60 second report
Before calling the dr:
7. Assess the baby
8. Read most recent notes
9. Have chart in hand
S
B ituation ackground
My name is ____, I am calling from ICU Who am I speaking to?
I am calling about Baby Boy Zechariah who is 3 weeks old
I’m calling because the baby is having episodes of apnoea and bradycardia today for the first time
He was admitted because of prematurity .
He was born at 27/40 gestation. Weight- 1.5kg
Born via NSVD - p remature labour thought to be brought on by chorioamnionitis
Apgars were... 5, 9, 9
Maternal history, HIV- negative RPR- negative
Problem list so far- He initially had antibiotics in the first week of life because of the chorioamnionitis.
He was doing well after a short period of CPAP. He is on continuous tube feeding, and has had regurge of formula, but otherwise has not had any other problems
Medications- He is on vitamins but no antibiotics
Test results- nil performed recently
A ssessment
Vital signs :
A- Airway- The airway is patent
B- Breathing- RR 75 and sats 92% on O2 28%. Previously noted desaturation to 75%.
C- Circulation- HR 130, decreased earlier, increased again with stimulation. He looks mottled.
D- Disability- He has slept more today, is less alert, and his muscle tone is less. The abdomen is soft and non-tender. The blood sugar is 3.8.
I think this patient might have...
an infection causing the bradycardia and low saturations. This might be because he has been regurgitating and aspirated his feeds.
R ecommendation
I have already increased the oxygen from 24% to 28%. We are doing a full set of observations every
15 minutes and he is on a saturation monitor.
I think he needs prompt assessment by a doctor to perform further investigations, and assess whether he needs antibiotics or not. I think this needs doing with the next 20 minutes
Can I repeat the plan back to you?
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
11
Scenario 2 ( Adapted from Limpopo Initiative in Newborn Care, 2011)
Baby Khanyile is brought to the neonatal unit from the postnatal ward. Her mother says she is going stiff and not feeding well.
She is 5 days old. She was born at 38/40 by emergency C-section for prolonged labour and foetal distress. Apgars were 6, 7, 10. Her mother had
HTN in pregnancy; maternal HIV and RPR were negative. Her birth weight was 3350 g and today she weighs 3540g. Apart from poor feeding, there have been no initial problems reported on the postnatal ward. The baby has not had any tests done, and is not on any medications.
She is breathing well and has a good circulation. Respiratory rate is 50 per minute, and saturations are 95% on room air. There is no grunting or chest in-drawing. HR is 120. Her temperature is 36.4oC. Blood glucose is 2.5mmol/l. She has increased tone and has irregular jerky movements. The fontanelle is full. She is jaundiced.
Exercise
Get into pairs. Assign someone as the doctor, and someone as the nurse. Use the coloured SBAR table provided to help you structure what you want to say. What other information are you missing in order to be able to fill in the table?
Remember:
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
Ideal answers are overleaf but please don’t cheat!
12
Neonatal
Escalation SBAR
A 30-60 second report
Before calling the dr:
1. Assess the baby
2. Read most recent notes
3. Have chart in hand
S ituation
My name is ----, I am calling from ---- Who am I speaking to?
I am calling about Baby Girl Khanyile who is 5 days old
I’m calling because the baby is hypoglycaemic, with increased tone and jaundice. Her mother says she is going stiff and not feeding well.
B
A ackground ssessment
She was admitted from postnatal ward today because of poor feeding
Gestation was 38/40
Her birth weight was 3350 g and today she weighs 3540 g
Born via emergency C-section for prolonged labour and foetal distress
Apgars were... 6, 7, 10
Maternal history- Her mother had HTN in pregnancy; HIV negative
Problem list so far- no initial problems reported
Medications nil
Test results- nil
Vital signs :
Breathing- Respiratory rate is 50 per minute. There is no grunting or chest in-drawing.
Circulation- HR is 120.
Disability- She has increased tone and has irregular jerky movements. The fontanelle is full.
She is jaundiced. Her temperature is 36.4
o
C. Her blood sugar is 2.5.
I think this child might have a missed HIE. Otherwise she might have sepsis.
R ecommendation
I have already..
started dextrose for the hypoglycaemia, as she is not feeding well. We’re avoiding oral feeds because we are concerned about the baby’s conscious level.
I am performing a full set of observations every 15 minutes. She is on a sats monitor.
I think she needs review to consider sending blood tests and perhaps a lumbar puncture/CFM monitoring. I think this needs doing within the next ten minutes .
Can I repeat the plan back to you?
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
13
Scenario 3 ( Adapted from Limpopo Initiative in Newborn Care, 2011)
Emergency CASE
– new admission– ABC-SBAR
A small baby, Lebo is brought to the nursery from labour ward. Her weight is 1.4 kg She is gasping, cyanosed and her Heart Rate is 120 per minute. She is pale, and extremely lethargic. Her blood glucose is 2.0 mmol / l
You start oxygen therapy via bag and mask. She starts breathing regularly on her own in 30 seconds. Respiratory rate is 80 / min, there is grunting and flaring and severe chest in drawing. She remains cyanosed, and saturations are 72%. The axillary temperature is 35.2
0
C. She has decreased tone and less than normal movement. Her fontanelle is normal. There is no jaundice, abdominal distension, or vomiting.
Exercise
Get into pairs. Assign someone as the doctor, and someone as the nurse. Communicate the above information using the SBAR model as if you are talking over the telephone. Use the coloured table provided to help you.
This is an emergency scenario, so it is better to use an ABC-SBAR structure.
Remember:
ABC - Airway, Breathing, Circulation
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
14
S ituation
Neonatal
Escalation SBAR
Before calling the dr:
1. Assess the baby
2. Read most recent notes
3. Have chart in hand
A 30-60 second report
My name is ___, I am calling from the nursery Who am I speaking to?
I am calling about Baby Girl Lebo who was born today
I’m calling because the baby has severe respiratory distress
Include vital signs here in an emergency situation
Breathing- She has a respiratory rate of 80, and saturations of 72% with cyanosis despite oxygen via nasal cannulae
Circulation- Her heart rate is 120 but she is pale
Disability- Blood sugar is 2.0
I am unsure of the gestation but her weight is 1.4 kg.
B ackground
A ssessment
R ecommendation
I have already... increased the oxygen and we are setting up CPAP
I think this baby may need intubation if CPAP is not successful
I need you to come immediately
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
15
Quiz Answers
1. Although the number of children dying under the age of 5 is decreasing, the proportion of children dying in the first month of life is increasing
True False. A 2013 UN report states that the number of children dying before the age five worldwide has declined from 12.4 million in 1990 to 6.6 million in
2012, despite population growth. However, as the rate of under-five deaths overall declines, the proportion that occurs during the first month after birth is increasing (UN, 2013).
2. Poor communication was the most common cause of avoidable infant death and disability in the USA in 2004
True False . In root cause analysis of nationally reported cases of infant death and permanent disability in the USA, communication issues among team members were the single most important factor identified (Joint Commission on Accreditation of Healthcare Organizations, 2004) . Faulty or delayed communication was considered the primary cause of the adverse event in 72% of cases.
3. The World Health Organisation recommends hospitals to have standardised hand-over
True False. The WHO collaborating centre published patient safety solution recommendations in 2007 (WHO Collaborating Centre for Patient Safety
Solutions, 2007) . “Improvement of communication during patient handover” was the third of nine solutions. The first strategy put forward to achieve this was ensuring a “standardized approach to hand-over communication between staff”, proposing the use of the SBAR (Situation, Background, Assessment, and Recommendation) technique.
4. Structured communication tools can only be used in clinical conversations
True False . At one hospital in Illinois, USA, SBAR was used for all clinical handovers, but also for ethics committee proposals and minutes of administrative meetings (Haig, 2006).
5.
When stating the “S” (situation) section of the SBAR communication, you should take as long as you need
True False. This is a brief description of the problem e.g. I’m calling because the baby is grunting.
It should take roughly 8 seconds. Remember, the whole of SBAR should take 30-60 seconds.
6. You can only use the structured communication tool SBAR if you know what is wrong with the patient
True False. It is completely acceptable, and safer, to say “I’m not sure what’s wrong, but I’m concerned”, than nothing at all (Leonard 2004).
7. The use of the structured communication tool SBAR has been shown to decrease unexpected patient deaths
True False. One study showed that training nurses in ABC and SBAR decreased unexpected patient deaths (De Meester, 2013)
16
References
Ascension Health. (2005). Premier Safety Institute . Retrieved from SafetyShare: https://www.premierinc.com/safety/safety-share/07-06downloads/09-sbar-perinatal-report.pdf
De Meester. (2013). SBAR improves nurse-physician communication and reduces unexpected death: A pre and post intervention study. Resuscitation ,
84(9):1192-6.
Haig. (2006). SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf , 32(3):167-75.
Institute for Healthcare Improvement. (2011, June). SBAR Training Scenarios and Competency Assessment.
Retrieved October 4, 2013, from http://www.ihi.org/knowledge/Pages/Tools/SBARTrainingScenariosandCompetencyAssessment.aspx
Leonard. (2004). The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care , 13:85 –90.
Limpopo Initiative in Newborn Care. (2011, August). Exercise Module in Sick and Small Newborns.
Joint Commission on Accreditation of Healthcare Organizations. (2004). Sentinel event alert Issue 30 . Retrieved March 7, 2006, from http://www.jcaho.org/about+us/
Jefferson InterProfessional Education Center. (n.d.). Interprofessional communication SBAR module.
Retrieved October 2013, from Jeffline: http://jeffline.jefferson.edu/jcipe/learning/didactic_files/SBAR%20IPE%20teaching%20plan%20v2.pdf
UN. (2013). http://www.un.org/millenniumgoals/childhealth.shtml
. Retrieved September 25, 2013, from Millenium Development Goals and Beyond 2015.
WHO Collaborating Centre for Patient Safety Solutions. (2007). Patient Safety Solutions . Retrieved September 19, 2013, from http://www.jointcommissioninternational.org/WHO-Collaborating-Centre-for-Patient-Safety-Solutions/
Project Leads
Dr. Meriel Raymond, UK NHS Improving Global Health Fellow
Prof. Mike Harrison, Neonatal consultant, Head of Neonatology Department
Sister Karen Michaels, Sister of Neonatal ward mellieraymond@gmail.com mc.harrison@uct.ac.za karenmics@yahoo.com
17
Pre-training quiz
(Adapted from Jefferson InterProfessional Education Center)
SBAR is a structured communication tool which stands for Situation, Background, Assessment and Recommendation.
Please circle true or false related to the following statements:
1. Although the number of children dying under the age of 5 is decreasing, the proportion of children dying in the first month of life is increasing
True False
2. Poor communication was the most common cause of avoidable infant death in the USA in 2004
True False
3. The World Health Organisation recommends hospitals to have standardised hand-over
True False
4. Structured communication tools can only be used in clinical conversations
True False
5. When stating the “S” (situation) section of the SBAR communication, you should take as long as you want
True False
6. You can only use the structured communication tool SBAR if you know what is wrong with the patient
True False
7. The use of the structured communication tool SBAR has been shown to decrease unexpected patient deaths
True False
18
Post-training quiz
(Adapted from Jefferson InterProfessional Education Center)
Please circle true or false related to the following statements:
1. Although the number of children dying under the age of 5 is decreasing, the proportion of children dying in the first month of life is increasing
True False
2. Poor communication was the most common cause of avoidable infant death in the USA in 2004
True False
3. The World Health Organisation recommends hospitals to have standardised hand-over
True False
4. SBAR is only appropriate in clinical conversations
True False
5. When stating the “S” (situation) section of the SBAR communication, you should take as long as you want
True False
6. You can only use the structured communication tool SBAR if you know what is wrong with the patient
True False
7. The use of the structured communication tool SBAR has been shown to decrease unexpected patient deaths
True False
19
SBAR training feedback
Please give your job title-
1. On a scale of 1 to 10 (with 1 being not confident at all and 10 being extremely confident)... a. How confident are you that the SBAR process will improve patient safety?
Not confident Somewhat Confident Extremely Confident
1 2 3 4 5 6 7 8 9 10 b. How confident are you that you will implement the SBAR process in the future?
Not confident
1 2 3
Somewhat Confident
4 5 6 7
Extremely Confident
8 9 10
2. How would you rate this training (where 1 is very poor and 10 is excellent) in terms of: a. Content
1 2 3 4 5 6 7 8 9 10 b. Presentation
1 2 3 4 5 6 7 8 9 10 c. Appropriateness
1 2 3 4 5 6 7 8 9 10
3. Anything you liked?
4. Anything that could have been done better?
5. List two things that you learned from this session today:
-
-
20
SBAR NEONATAL DOCTOR TRAINING
Written by Dr. Meriel Raymond, UK NHS Improving Global Health Fellow, in conjunction with the neonatal department at Groote Schuur Hospital, Cape Town
Contents:
1.
2.
3.
4.
Case Scenario 1
Case Scenario 2
Case Scenario 3
Case Scenario 4
21
SBAR NEONATAL DOCTOR TRAINING SCENARIOS
Scenario 1 (Adapted from Institute for Healthcare Improvement, 2011)- Intern to registrar
Zechariah is a 3-week old infant in ICU. He was at 27 weeks gestation when born by vaginal delivery. The p remature labour was thought to be brought on by chorioamnionitis. Apgars were 5, 9, 9. Maternal HIV and RPR were negative.
He received antibiotics in the first week of life, but there have been no signs of infection since then.
He has been progressing well after a short period of CPAP and remains in 24% flow support. He is receiving continuous tube feedings. Recently he has had some regurgitation of formula. He has demonstrated a steady weight increase, and currently weighs 1.5kg. He is on vitamins but not on any antibiotics.
For the first time today, he has had a couple of episodes of apnoea. The day nurse reported that he had slept a lot today and his mother felt he wasn’t as alert as usual. When the evening nurse came on and did her assessment she noted he was tachypnoeic with a respiratory rate of 75.
As she was documenting her assessment, Zechariah had a bradycardic episode and his oxygen saturation decreased to 75. His heart rate returned to 130 with stimulation and the nurse increased the oxygen to 28%, with saturations of 92%.
You are the intern. The nurse has now called you to ask for help. When you arrive, the baby has mild signs of respiratory distress (intercostal recession, respiratory rate of 60, saturations of 93% on 28% O
2
). HR remains at 130, and his colouring is mottled. Temperature is 37.5
o
C. The blood glucose is 3.8.
His muscle tone is diminished. The abdo men isn’t distended.
You are concerned that the baby may need further investigations and possible treatment for an infection.
Exercise
Get into pairs. Assign someone as the intern, and someone as the registrar (and swap for the next task so you each get a turn). Use the coloured
SBAR table provided to help you structure what you want to say.
Ideal answers are overleaf but please don’t cheat! Remember:
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
22
Recommendation - What would I do to correct it?
S ituation
B ackground
A ssessment
R ecommendation
Neonatal
Escalation SBAR
A 30-60 second report
Before calling the dr:
10.
11.
12.
Assess the baby
Read most recent notes
Have chart in hand
My name is ___, I am calling from ICU Who am I speaking to?
I am calling about Baby Boy Zechariah who is 3 weeks old
I’m calling because the baby is having episodes of apnoea and bradycardia today for the first time
He was admitted because of prematurity .
He was born at 27/40 gestation. Weight- 1.5kg
Born via NSVD - premature labour thought to be brought on by chorioamnionitis
Apgars were... 5, 9, 9
Maternal history, HIV- negative RPR- negative
Problem list so far- He initially had antibiotics in the first week of life because of the chorioamnionitis.
He was doing well after a short period of CPAP. He is on continuous tube feeding, and has had regurge of formula, but otherwise has not had any other problems
Medications- He is on vitamins but no antibiotics
Test results- nil performed recently
Vital signs :
E- Airway- The airway is patent
F- Breathing- RR 75 and sats 92% on O
2
28%. Previously noted desaturation to 75%.
G- Circulation- HR 130, decreased earlier, increased again with stimulation. He looks mottled.
The temperature is 37.5.
He has slept more today, is less alert, and his muscle tone is less. The abdomen is soft and non-tender. The blood sugar is 3.8.
I think this patient might have...
an infection causing the bradycardia and low saturations. This might be because he has been regurgitating and aspirated his feeds.
I have already... asked the nurses to do a full set of observations every 15 minutes and he is on a saturation monitor.
I think this baby needs...
a gas, blood tests and cultures sending, so I am putting in a line, and a chest X-ray, which I am arranging. I also think he needs antibiotics regardless, as an infection is the most likely underlying problem.
I need your advice as to whether this is the right thing to do.
When shall I call you back if there is no improvement? Shall I let you know the results?
23
Scenario 2 ( Adapted from Limpopo Initiative in Newborn Care, 2011)- Medical officer to registrar
Baby Khanyile is brought to the neonatal unit from the postnatal ward. Her mother says she is going stiff and not feeding well.
She is 5 days old. She was born at 38/40 by emergency C-section for prolonged labour and foetal distress. Apgars were 6, 7, 10. Her mother had
HTN in pregnancy; maternal HIV and RPR were negative. Her birth weight was 3.35kg and today she weighs 3.54kg. Apart from poor feeding, there have been no initial problems reported on the postnatal ward. The baby has not had any tests done, and is not on any medications.
Respiratory rate is 50 per minute, and saturations are 95% on room air. There is no respiratory distress. HR is 120 and the baby is pink. Her temperature is 36.4
o
C. Blood glucose is 2.8mmol/l. She has increased tone and has irregular jerky movements. The fontanelle is full. She is jaundiced.
You are the medical officer, and are called by the nurse to assess the baby. You are concerned about the possibility of infection causing the jaundice, and so send off a TSB along with other tests. The ward TSB comes up above the line for phototherapy, which you ask the nurses to set up. However, you are still concerned about the baby’s neurology. You want the registrar to see the baby with you.
Exercise
Get into pairs. Assign someone as the medical officer, and someone as the registrar. Use the coloured SBAR table provided to help you structure what you want to say.
Remember:
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
Ideal answers are overleaf but please don’t cheat!
24
Neonatal
Escalation SBAR
A 30-60 second report
Before calling the dr:
4. Assess the baby
5. Read most recent notes
6. Have chart in hand
S ituation
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about Baby Girl Khanyile who is 5 days old
I’m calling because the baby is hypoglycaemic, with increased tone and jaundice. Her mother says she is going stiff and not feeding well.
B
A ackground ssessment
The baby was admitted because of poor feeding from postnatal ward today
Gestation was 38/40 Weight Her birth weight was 3.35kg and today she weighs 3.54kg
Born via emergency C-section for prolonged labour and foetal distress
Apgars were... 6, 7, 10
Maternal history- Her mother had HTN in pregnancy; HIV negative
Problem list so far- no initial problems reported
Medications nil
Test results- nil
Vital signs :
Breathing- Respiratory rate is 50 per minute. There is no grunting or chest in-drawing.
Circulation- HR is 120.
She has increased tone and has irregular jerky movements. The fontanelle is full. is jaundiced. Her temperature is 36.4
o
C. Her blood sugar is 2.8.
She
I think this child might have... jaundice and hypoglycaemia secondary to poor feeding. Otherwise it might be a missed HIE, or sepsis.
R ecommendation
I have already..
started dextrose for the hypoglycaemia, as she is not feeding well. We’re avoiding oral feeds because we are concerned about the baby’s conscious level. Phototherapy has been started.
The nurses are performing a full set of observations every 15 minutes. She is on a sats monitor. I’ve sent bloods for inflammatory markers and a lab bilirubin.
I think this baby needs...
a lumbar puncture/CFM monitoring if she doesn’t improve with the dextrose.
I think this needs doing within the next fifteen minutes. Is this going to be possible?
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
25
Scenario 3 ( Adapted from Limpopo Initiative in Newborn Care, 2011)- Emergency, Intern to Registrar
Emergency CASE
– new admission– ABC-SBAR
A small baby, Lebo is brought to the nursery from labour ward without any notes or other information. She is gasping, cyanosed and her Heart
Rate is 120 per minute. She is pale, and extremely lethargic. Her blood glucose is 2.0 mmol / l
You are the intern on the ward. You start oxygen therapy via bag and mask. She starts breathing regularly on her own in 30 seconds.
Respiratory rate is 80 / min, there is grunting and flaring and severe chest in drawing. She remains cyanosed, and saturations are 72%. Her weight is 1.4 kg and the axillary temperature is 35.2
0
C. She has decreased tone and less than normal movement. Her fontanelle is normal.
There is no jaundice, abdominal distension, or vomiting.
Exercise
Get into pairs. Assign someone as the intern, and someone as the registrar/consultant. Communicate the above information using the SBAR model as if you are talking over the telephone. Use the coloured table provided to help you.
This is an emergency scenario, so it is better to use an ABC-SBAR structure.
Remember:
ABC - Airway, Breathing, Circulation
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
26
Neonatal
Escalation SBAR
A 30-60 second report
Before calling the dr:
4. Assess the baby
5. Read most recent notes
6. Have chart in hand
S ituation
My name is ----, I am calling from the nursery Who am I speaking to?
I am calling about Baby Girl Lebo who was born today
I’m calling because the baby has severe respiratory distress
Include vital signs here in an emergency situation
Airway- The airway is patent
Breathing- She has a respiratory rate of 80, and saturations of 72% with cyanosis despite oxygen via nasal cannulae
Circulation- Her heart rate is 120 but she is pale
Disability- Blood sugar is 2.0
I am unsure of the gestation but her weight is 1.4 kg.
B ackground
A ssessment
R ecommendation
I have already... increased the oxygen and we are setting up CPAP
I think this baby may need intubation if CPAP is not successful
I need you to come immediately
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
27
Scenario 4 (Adapted from DeBoer, 1997)- Emergency, Registrar to consultant
Registrar-consultant
Baby Ramasala is born at 42/40 gestation via normal vaginal delivery to a healthy primaparous mother with no complications. The antenatal anomaly scan was normal. She weighs 3.4kg Apgars are 6, 8. The medical officer is called to labour ward as the midwives are concerned about the baby. She is admitted to ICU1 and receives 40% O2 via CPAP- the saturations are 90% on this. In the first few hours after birth, the baby starts to desaturate, and you as the registrar are called by the medical officer. You diagnose bilateral pneumothoraces, aspirate them, and site chest drains. There is minimal improvement in the gases or respiratory effort. You intubate the baby under sedation. BP remains low at 60 systolic, and saturations remain in the 80s. The gas shows that a metabolic acidosis is developing. Lab bloods are pending.
Exercise
Get into pairs. Assign someone as the registrar, and someone as the consultant. Communicate the above information using the SBAR model as if you are talking over the telephone. Use the coloured table provided to help you.
This is an emergency scenario, so it is better to use an ABC-SBAR structure.
Remember:
ABC - Airway, Breathing, Circulation
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
28
S ituation
Neonatal Escalation
SBAR
A 30-60 second report
Before calling the dr:
1. Assess the baby
2. Read most recent notes
3. Have chart in hand
My name is Dr.___
I am calling from ICU1 Who am I speaking to?
I am calling about Baby Girl Ramasala who was born today
I’m calling because the baby is desaturating and hypotensive despite intubation
Include vital signs here in an emergency situation
Breathing- Saturations are 80% despite optimum oxygen therapy. The baby had b/l pneumothoraces which have been aspirated, and chest drains sited.
C- BP is 60 systolic, HR is 180
B ackground
The baby was admitted because of....
Gestation 42/40 Weight poor saturations
3.4kg
Born via: NSVD
Maternal history
Apgars: 6,8
Normal antenatal anomaly scan HIV Y/ N
Medications- the baby is sedated
Test results- the gas pH is worsening. The labs are awaited- I have sent basic bloods and cultures.
I think this patient might have..... PPHN, sepsis, congenital cardiac abnormality
It is fine to say
“I’m not sure what’s wrong with this patient, but I am concerned” “I’m uncomfortable” “this is unsafe”
A ssessment
R ecommendation
I think this baby needs.... oscillation, dobutamine, possibly broad spectrum antibiotics, blood transfusion, echocardiogram, ?consultant review.
I think this needs doing within the next
Can I repeat the plan back to you? ten mins. Is it possible for you to come?
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
29
Obstetric
Escalation SBAR
A 30-60 second report
Before calling the dr:
1. Assess the patient
2. Read most recent notes
3. Have chart in hand
S
B
A ituation ackground ssessment
R ecommendation
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about patient ____ who is AN/Intrapartum/PN
I’m calling because...
I’m concerned about FHR, contraction pattern, BP, vaginal bleeding etc.
Include vital signs here in an emergency situation
The patient has been admitted because....
Gravida __ Para __ @ __ /40
Significant Medical and Obstetric History, HIV + RPR
Problems in current pregnancy
Significant meds/allergies
Blood/urine results
Maternal vital signs :
Airway / Breathing - RR O
2
sats Circulation - HR, BP, fluid balance
In labour: Membranes: Intact/SROM @____on ____ PROM Y/N
Temperature
Presentation Fifths palpable Cervical dilation Station Position
FHR/CTG: heart rate____ , interpretation
I think this patient might have.....
an infection, an APH, foetal distress from prolonged labour etc.
Or “I’m not sure what’s going on with this patient, but I am worried”
I have already... commenced CTG monitoring, increased IVI etc.
I think this patient needs....
an emergency C-section, an epidural, antibiotics, review etc.
I think this needs doing within the next...... ___mins/hrs
How often should I do observations? When shall I call you back if there is no improvement?
Can I repeat the plan back to you?
30
Midwife Neonatal
Escalation SBAR
A 30-60 second report
Before calling the dr:
1. Assess the baby
2. Read most recent notes
3. Have chart in hand
S
B
A ituation ackground ssessment
R ecommendation
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about Baby Boy or Girl ____ who is ____ old
I’m calling because... the baby is blue, grunting, irritable, jaundiced, hypoglycaemic etc.
Include vital signs here in an emergency situation
The baby was admitted because of....
Gestation Weight
Born via: C/S (give reason)
Maternal history
NSVD
HIV Y/N poor feeding, jaundice etc.
Forceps Ventouse Apgars:
Problem list
Medications Test results
Vital signs :
Airway / Breathing
Circulation
RR
HR
Oxygen Saturations
Temperature Blood Glucose
I think this patient might have .....
an infection, respiratory distress etc.
Or: “I’m not sure what’s wrong with this baby, but I am worried”
I have already... increased the oxygen, put the baby on monitoring, started phototherapy etc.
I think this baby needs....
antibiotics, review etc.
I think this needs doing within the next ____ mins/hrs/days
How often should I do observations? When shall I call you back if there is no improvement?
Can I repeat the plan back to you?
Developed GSH, 10.2013 by UK NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contacts Prof Harrison mc.harrison@uct.ac.za and Sister Eileen Simmonds. Adapted Lourdes Perinatal SBAR 2005.
31
Paediatric
Attendance at
Delivery SBAR
A 30-60 second report
Before calling the dr:
1. Assess the mother
2. Read most recent notes
3. Have chart in hand
S
ituation
My name is ____, I am calling from____ Who am I speaking to?
I am calling about patient____ in bed____
I’m calling to request your attendance at..... C/S (em/planned) NSVD Forceps/Ventouse
Indication for type of delivery
We need your attendance because
...
of Foetal distress, prematurity, twins, etc.
B
A
ackground ssessment
Gestation
PROL Y/N
Maternal history, HIV + RPR
Problems this pregnancy
Maternal abx:
Maternal steroids:
Foetal position
EFW
Date:
Date:
Time:
Time:
FH/CTG
It is fine to say “We’re not sure if there will be a problem with the baby, but we’re concerned and would like you there”
R
ecommendation
I would like you to attend at _________ within the next ___mins
Paediatric registrar required Y/N
Can I repeat the plan back to you?
Developed for Groote Schuur Hospital 11.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za
; Eileen Simmonds. Adapted (Ascension Health, 2005)
32
Obstetric SBAR escalation/transfer sticker
Developed for Groote Schuur Hospital 11.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond. Lead contact Eileen Simmonds
Name of patient
Location
Date & time of call
Situation Name/location of caller
Name of doctor receiving call
Age of patient
AN/Intrapartum/PN
Presenting problem
Background
Assessment
Recommendation
Reason for admission
Gravida __ Para __ @ __ /40
Membranes: Intact/SROM @____on ____
Significant Medical and Obstetric History
PROM Y/N
HIV Y/N RPR Y/N
Problems in current pregnancy
Significant meds/allergies
Blood/urine results
Vital signs Airway/Breathing RR Oxygen saturations
Circulation HR BP
Temperature Blood Glucose
In labour: Presentation Fifths palpable Cervical dilation Station Position
FHR/CTG : heart rate____ , interpretation
Possible diagnosis
What does the caller recommend?
-Obstetric Review Y/N
-Anaesthetic Review
-Delivery by
Y/N
C-section in ____mins/hrs in ____mins/hrs
Ventouse/Forceps
-Tests/Treatment
-Transfer ETD
Frequency of observations
ETA
When to call back in ____mins/hrs
Repeat plan back
33
SBAR MIDWIFE TRAINING
Written by Dr. Meriel Raymond, UK NHS Improving Global Health Fellow, in conjunction with the neonatal and obstetric departments at Groote Schuur Hospital, Cape Town
Contents:
Case Scenario 1
Case Scenario 2
Case Scenario 3
References
34
SBAR MIDWIFE TRAINING SCENARIOS
Scenario 1- Obstetric
(Adapted from Institute for Healthcare Improvement, 2011)
Esihle Mantashe, a 25-year-old primipara, is in the recovery room after a low forceps delivery of a 4kg term male. She is given syntometrine IM just after delivery.
Forty-five minutes after delivery, her vital signs are BP 100/60, pulse 88 and respirations 16. Her fundus is firm and is at level of umbilicus, no clots observed. She has continuous trickle of bright red lochia. No change in perineal oedema, ice pack applied and pads changed. Pads weight indicates 300cc of blood loss.
Fifteen minutes later the fundus is massaged and remains firm at umbilical level and midline. A constant trickle of bright red lochia persists with no clots expressed. Peripads weighed showing an additional 200 cc blood loss. Vital signs are now BP 90/52, pulse 110 and respirations 20.
You would like an emergency obstetric review.
Exercise
Get into pairs. Assign someone as the midwife, and someone as the obstetric doctor. Use the coloured SBAR table provided to help you structure what you want to say. What other information are you missing in order to be able to fill in the table?
This is an emergency scenario, so it is better to put the vital signs in the Situation rather than the Assessment section
Remember:
Situation - What is going on with the patient?
ABC - Airway, Breathing, Circulation
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
35
Obstetric
Escalation SBAR
A 30-60 second report
Before calling the dr:
1. Assess the patient
2. Read most recent notes
3. Have chart in hand
S
B ituation ackground
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about patient Esihle Mantashe who is AN/Intrapartum/ PN
I’m calling because I’m concerned about PPH, with a rising pulse and dropping BP
Include vital signs here in an emergency situation
ABC Airway / Breathing - RR 20 from 16
Circulation - HR 110 from 88
The patient has been admitted in labour
O
2
sats
BP 90/52 from 100/60
Fluid balance Blood loss thought to be 500ml. There is a continuous trickle of bright red lochia.
Gravida _ 1 _ Para _ 1 _ @ 40 /40
Significant Medical and Obstetric History, HIV + RPR- forceps delivery of a 4kg infant 45 mins ago.
Problems in current pregnancy- nil
Significant medications (antibiotics, steroids, magnesium sulphate), drug allergies- nil
Blood/urine results - nil Rhesus pos/neg- unknown
A ssessment
R ecommendation
Maternal vital signs :
temp
Cervical dilation Foetal position
FHR/CTG : heart rate____ , interpretation
I think this patient might have..... PPH from the fundus not contracting down, with cardiovascular compromise
It is fine to say
“I’m not sure what’s going on with this patient, but I am concerned” “I’m uncomfortable” “this is unsafe”
I have already... given syntometrine post delivery. I have massaged the fundus twice but it remains firm at umbilical level and midline . Perineal ice packs haven’t helped. I’ve increased the IVI, and am repeating observations every 5 minutes.
I think this patient needs.... another IV line, an O- blood transfusion, and obstetric review
I think this needs doing within the next...... _ 5 __mins
How often should I do observations? When shall I call you back if there is no improvement?
Can I repeat the plan back to you?
Developed for Groote Schuur Hospital 10.2013 by UK NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Eileen Simmonds. Adapted from Lourdes Perinatal SBAR.2005
.
36
Scenario 2: Attendance at delivery (Adapted from Edwards, Dec/Jan 2009)
At 16.00, at Groote Schuur labour ward, you accept a transferred patient from Somerset Hospital, Aneni Biri. She is a 32yo gravida 3, para 2 with preterm labor at 30 weeks ’ gestation. Estimated foetal weight is unknown. This morning she attended Somerset labour ward with labour pains. Her membranes ruptured at 08.30. She was given 12 mg betamethasone at 10:00 a.m.
Currently she's 2 centimeters, 50 percent effaced, and –3 station. The position is breech. The CTG baseline is 160, and shows late decelerations.
As the midwife you are concerned about preterm labour which you are unable to stop, and foetal distress. You think that an emergency C-section is indicated, and would like the paediatric doctor to attend.
Exercise
Get into pairs. Assign someone as the midwife, and someone as the paediatric doctor. Use the coloured SBAR table provided to help you structure what you want to say.
Remember:
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
Ideal answers are overleaf but please don’t cheat!
37
Paediatric
Attendance at
Before calling the dr:
1. Assess the mother
2. Read most recent notes
3. Have chart in hand
Delivery SBAR
A 30-60 second report
S
B ituation ackground
My name is ----, I am calling from labour ward Who am I speaking to?
I am calling about patient Aneni Biri in room 2
I’m calling to request your attendance at an emergency C-section
We need your attendance because of.... preterm labour, breech presentation and foetal distress
Gestation- 30/40
Membranes Intact / SROM @__ 08.30
__ on__ today _
Maternal history, HIV + RPR
Problems this pregnancy
Maternal abx Nil
Maternal steroids 12mg bethamethasone given at 10.00
A ssessment
FHR/CTG- baseline of 160 with late decelerations
Foetal position Breech
R ecommendation
I would like you to attend within the next 10 mins in theatre
Paediatric Registrar required Y/ N
Can you please confirm you are coming?
38
Scenario 3- Review of baby ( Adapted from Limpopo Initiative in Newborn Care, 2011)
Baby Khanyile is on the postnatal ward. Her mother says she is going stiff today and not feeding well.
She is 5 days old. She was born at 38/40 by emergency C-section for prolonged labour and foetal distress. Apgars were 6, 7, 10. Her mother had
HTN in pregnancy; maternal HIV and RPR were negative. Her birth weight was 3.35kg and today she weighs 3.54kg. Apart from poor feeding, there have been no initial problems reported on the postnatal ward. The baby has not had any tests done, and is not on any medications.
She is breathing well and has a good circulation. Respiratory rate is 50 per minute, and saturations are 97% on room air. There is no grunting or chest in-drawing. HR is 120. Her temperature is 36.4oC. Blood glucose is 2.8mmol/l. She has increased tone and has irregular jerky movements.
The fontanelle is full. She is jaundiced.
Exercise
Get into pairs. Assign someone as the paediatric doctor, and someone as the midwife. Use the coloured SBAR table provided to help you structure what you want to say.
Remember:
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
Ideal answers are overleaf but please don’t cheat!
39
Midwife Neonatal
Escalation SBAR
Before calling the dr:
1. Assess the baby
2. Read most recent notes
3. Have chart in hand
A 30-60 second report
S ituation
My name is ----, I am calling from ---- Who am I speaking to?
I am calling about Baby Girl Khanyile who is 5 days old
I’m calling because the baby is hypoglycaemic, with increased tone and jaundice. Her mother says she is going stiff and not feeding well.
B ackground
She was admitted to the ward after birth because of poor feeding
Gestation was 38/40
Her birth weight was 3350 g and today she weighs 3540 g
Born via emergency C-section for prolonged labour and foetal distress
Apgars were... 6, 7, 10
Maternal history- Her mother had HTN in pregnancy; HIV negative
Problem list so far- no initial problems reported
Medications nil
Test results- nil
Vital signs :
Breathing- Respiratory rate is 50 per minute. Sats 97% on room air. There is no grunting or
A ssessment chest in-drawing.
Circulation- HR is 120.
Disability- She has increased tone and has irregular jerky movements. The fontanelle is full.
She is jaundiced. Her temperature is 36.4
o
C. Her blood sugar is 2.8.
I think this child might have... something neurological wrong with itan infection, or hypoxia.
R ecommendation
I have already..
advised Mum to avoid oral feeds because we are concerned about the baby’s conscious level.
I am performing a full set of observations every 15 minutes.
I think she needs prompt review and transfer to the nursery. Please come and see her within the next ten minutes.
Can I repeat the plan back to you?
Developed Neonatal Department, Groote Schuur Hospital 09.2013 by NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Prof Harrison mc.harrison@uct.ac.za. Adapted (Ascension Health, 2005)
40
References
Ascension Health. (2005). Premier Safety Institute . Retrieved from SafetyShare: https://www.premierinc.com/safety/safety-share/07-06downloads/09-sbar-perinatal-report.pdf
De Meester. (2013). SBAR improves nurse-physician communication and reduces unexpected death: A pre and post intervention study. Resuscitation ,
84(9):1192-6.
Edwards. (Dec/Jan 2009). SBAR for Maternal Transports: Going the Extra Mile. Nursing for Women's Health , Volume 12, Issue 6, pages 515
–520.
Haig. (2006). SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf , 32(3):167-75.
Institute for Healthcare Improvement. (2011, June). SBAR Training Scenarios and Competency Assessment.
Retrieved October 4, 2013, from http://www.ihi.org/knowledge/Pages/Tools/SBARTrainingScenariosandCompetencyAssessment.aspx
Leonard. (2004). The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care , 13:85
–90.
Limpopo Initiative in Newborn Care. (2011, August). Exercise Module in Sick and Small Newborns.
Joint Commission on Accreditation of Healthcare Organizations. (2004). Sentinel event alert Issue 30 . Retrieved March 7, 2006, from http://www.jcaho.org/about+us/
Jefferson InterProfessional Education Center. (n.d.). Interprofessional communication SBAR module.
Retrieved October 2013, from Jeffline: http://jeffline.jefferson.edu/jcipe/learning/didactic_files/SBAR%20IPE%20teaching%20plan%20v2.pdf
UN. (2013). http://www.un.org/millenniumgoals/childhealth.shtml
. Retrieved September 25, 2013, from Millenium Development Goals and Beyond 2015.
WHO Collaborating Centre for Patient Safety Solutions. (2007). Patient Safety Solutions . Retrieved September 19, 2013, from http://www.jointcommissioninternational.org/WHO-Collaborating-Centre-for-Patient-Safety-Solutions/
41
SBAR OBSTETRICIAN TRAINING
Written by Dr. Meriel Raymond, UK NHS Improving Global Health Fellow, in conjunction with the Obstetric department at
Groote Schuur Hospital, Cape Town
Contents:
Case Scenario 1
Case Scenario 2
42
SBAR OBSTETRICIAN TRAINING SCENARIOS
Scenario 1- Medical officer to registrar
(Adapted from Institute for Healthcare Improvement, 2011)
Esihle Mantashe, a 25-year-old primipara, is in the recovery room after a low forceps delivery of a 4kg term male. She is given syntometrine IM just after delivery.
It is an hour after delivery and the midwife notes she has lost 500ml of blood. There is a continuous trickle of bright red lochia but no clots expressed. The BP is 90/52 from 100/60 15 minutes before, and p110 from 88 15 mins before. The fundus is massaged but remains firm at umbilical level and midline.
The midwife calls you, the medical officer, for an emergency review.
You arrive at 1 hr 5 mins post delivery. You insert another IV line and arrange for a 4 unit blood transfusion and pitocin infusion. You ask the midwife to catheterise the patient. There is a further 500ml of vaginal blood loss over the next 30 minutes. The vitals have changed to RR 25, BP
82/44, p130.
You are concerned that this woman needs surgical exploration to stop the blood loss.
Exercise
Get into pairs. Assign someone as the medical officer, and someone as the registrar. Use the SBAR table provided to help you structure what you want to say.
This is an emergency scenario, so it is better to put the vital signs in the Situation rather than the Assessment section
Remember:
Situation - What is going on with the patient?
ABC - Airway, Breathing, Circulation
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
43
Obstetric
Escalation SBAR
A 30-60 second report
Before calling the dr:
4. Assess the patient
5. Read most recent notes
6. Have chart in hand
S
B ituation ackground
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about patient Esihle Mantashe who is AN/Intrapartum/ PN
I’m calling because I’m concerned about PPH, with a rising pulse and dropping BP
Include vital signs here in an emergency situation
ABC Airway / Breathing - RR 25
Circulation - HR 130
O
2
sats
BP 82/44
Fluid balance Blood loss of l litre. There is a continuous trickle of bright red lochia.
The patient has been admitted in labour
Gravida _ 1 _ Para _ 1 _ @ 40 /40
Significant Medical and Obstetric History, HIV + RPR- forceps delivery of a 4kg infant 1hr 30 mins ago.
Problems in current pregnancy- nil
Significant medications (antibiotics, steroids, magnesium sulphate), drug allergies- nil
Blood/urine results - nil Rhesus pos/neg- unknown
Maternal vital signs :
temp
Cervical dilation Foetal position
FHR/CTG : heart rate____ , interpretation
A ssessment
R ecommendation
I think this patient might have..... PPH from the fundus not contracting down, with cardiovascular compromise
It is fine to say
“I’m not sure what’s going on with this patient, but I am concerned” “I’m uncomfortable” “this is unsafe”
I have already... given syntometrine post delivery. Massaging the fundus hasn’t helped. I’ve arranged a 4 unit blood transfusion and am running it stat. There is a pitocin infusion running.
I think this patient needs.... uterine compression or surgical exploration
I think this needs doing within the next...... _ 5 __mins
How often should I do observations? When shall I call you back if there is no improvement?
Can I repeat the plan back to you?
Developed for Groote Schuur Hospital 10.2013 by UK NHS Improving Global Health Fellow Dr. Meriel Raymond; lead contact Eileen Simmonds. Adapted from Lourdes Perinatal SBAR.2005
.
44
Scenario 2: Junior registrar to consultant (Adapted from Edwards, Dec/Jan 2009)
At 16.00, at Groote Schuur labour ward, you accept a transferred patient from Somerset Hospital, Aneni Biri. She is a 32yo gravida 3, para 2 with preterm labour at 30 weeks
’ gestation. No problems this pregnancy. Her first baby was born by emergency C-section for pre-eclampsia and foetal distress, and the second was a normal vaginal delivery. This morning she attended Somerset with labour pains. Her membranes ruptured at 08.30.
She was given 12 mg betamethasone at 10:00 a.m.
Currently she's 2 centimeters dilated, 50 percent effaced, and
–3 station. The position is breech. The CTG baseline is 130, and shows late decelerations. It is otherwise normal. Maternal vital signs are normal.
As the junior registrar you are concerned about the possibility of foetal distress, and think this may warrant an emergency C-section, but would like advice as to whether this labour could be safely delayed with tocolytics and monitoring.
Exercise
Get into pairs. Assign someone as the registrar, and someone as the consultant. Use the SBAR table provided to help you structure what you want to say.
Remember:
Situation - What is going on with the patient?
Background - What is the clinical background or context?
Assessment - What do I think the problem is?
Recommendation - What would I do to correct it?
Ideal answers are overleaf but please don’t cheat!
45
Obstetric
Escalation SBAR
A 30-60 second report
Before calling the dr:
1. Assess the patient
2. Read most recent notes
3. Have chart in hand
S
B
A ituation ackground ssessment
R ecommendation
My name is ____, I am calling from ____ Who am I speaking to?
I am calling about patient Aneni Biri who is AN/ Intrapartum /PN
I’m calling because...
I’m concerned about an abnormal CTG in preterm labour and would like some advice
Include vital signs here in an emergency situation
The patient has been admitted to Somerset hospital in labour and transferred here
Gravida 3 __ Para 2 __ @ 30 __ /40
Significant Medical and Obstetric History, HIV + RPR- Her first baby was born by emergency Csection for pre-eclampsia and foetal distress, and the second was a normal vaginal delivery
Problems in current pregnancy- nil
Significant meds/allergies- 1 dose 12mg betamethasone at 10.00
Blood/urine results
Maternal vital signs :
Vital signs are normal
In labour: Membranes ruptured at 08.30 today
Presentation- breech Cervical- 2 centimeters dilated Station –3 station
FHR/CTG: heart rate 130, late decelerations
I think this patient might have.....
preterm labour with foetal distress
Or “I’m not sure what’s going on with this patient, but I am worried”
I think this patient needs....
either an emergency C-section, or tocolysis, and need your advice on which would be more appropriate.
Can I repeat the plan back to you? When would you want me to call you back?
46
47