Lesions of the Petrous Apex - University of Texas Medical Branch
advertisement

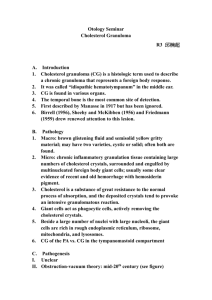
Lesions of the Petrous Apex Resident Physician: Nikunj A. Rana, M.D. Faculty Mentor/Discussant: Dayton Young, M.D. The University of Texas Medical Branch – UTMB Health Department of Otolaryngology Grand Rounds Presentation January 28, 2015 Series Editor: Francis B. Quinn, Jr., MD, FACS -- Archivist: Melinda Stoner Quinn, MSICS Outline I. II. III. IV. V. VI. VII. Anatomy Clinical Presentation Common Lesions Cholesterol Granulomas Surgical Approaches Outcomes References Skull Base Tumors IAC Jugular Foramen Mastiod/Middle ear EAC Petrous Apex Axial CT Anatomy Axial CT Anatomy • The petrous apex is the pyramidal, medial projection of the petrous portion of the temporal bone. • The normal petrous apex is relatively simple in form with only one principal variation: the degree of pneumatization. • That is, the apex may be variably pneumatized with aerated connections to the middle ear or may contain predominantly marrow fat. 80% adult mastoid aerated • 30% adult petrous region aerated, 7% asymmetric (Brackman) • Medial View Medial View • The petrous apex is the pyramidal, medial projection of the petrous portion of the temporal bone. • Can be anatomically described as a pyramid- shaped structure that can be divided in a posterior and an anterior part by a line passing in the coronal plane through the internal auditory canal • Chole, RA. “Petrous apicitis: surgical anatomy,” Annals of Otology, Rhinology and Laryngology, vol.94, no.3, pp. 254–257,1985. Axial CT Anatomy Axial CT Anatomy • The petrous apex of the temporal bone is located anteromedial to the inner ear within the angle created by the greater wing of the sphenoid bone anteriorly and the occipital bone posteriorly. • The anterior margin of the petrous apex forms the medial posterior wall of the middle cranial fossa. Superior View Superior View • The petrous apex of the temporal bone is located anteromedial to the inner ear within the angle created by the greater wing of the sphenoid bone anteriorly and the occipital bone posteriorly. • The anterior margin of the petrous apex forms the medial posterior wall of the middle cranial fossa. Inferior View Inferior View The most inferior and medial exocranial margin of PA is separated from the clivus by • the foramen lacerum • • Above the foramen lacerum, the ICA exits the medial opening of the carotid canal on its way to the cavernous sinus. Chapman PR, Shah R, Cure JK, Bag AK. Petrous Apex Lesions: Pictorial Review. AJR:196, March 2011 Superior View What makes the petrous apex anatomically complex is its medial location in the skull base and its intimate relationship to other clinically important structures including: • the cavernous sinus • Dorello canal • Meckel cave. Outline I. II. III. IV. V. VI. VII. Anatomy Clinical Presentation Common Lesions Cholesterol Granulomas Surgical Approaches Outcomes References Clinical Presentation Very Broad Primary Lesions Bone Penumatized air cells ICA “Down-going” intracranial processes “Up-going” invasive nasopharyngeal or sinonasal lesions via sinus of Morgagni Given its location, the petrous apex is susceptible to multiple pathologic processes including intrinsic lesions of bone, pneumatized air cells, or the petrous internal carotid artery; invasive “downgoing” intracranial pro- cesses; or invasive “upgoing” infiltrating nasopharyngeal or sinonasal lesions. Chapman PR, Shah R, Cure JK, Bag AK. Petrous Apex Lesions: A Pictorial Review. AJR 2011; 196:WS26–WS37 Clinical Presentation Close proximity to Trigeminal Ganglion in Meckel’s Cave Petrosphenoidal ligament –> Dorello Canal (superior envagination) abducens nerve Gradenigo’s syndrome: retro-orbital pain, otorrhea, ipsilateral CN VI palsy • Gradenigo’s syndrome: retro-orbital pain, otorrhea, ipsilateral CN VI palsy • Compression of IAC hearing loss and vestibular dysfunction • CN VII: late if slow growing mass, early if neoplasms or IAC involvement • Pain more common with neoplasms • Mastoid: CN IX neck pain • Middle Fossa and Superior petrosal region: CN V retro-orbital and facial pain • Posterior Fossa: CN IX/X and first 3 cervical roots Other Cranial Nerves Compression of IAC Facial Nerve Hearing loss Vestibular Dysfunction Facial paralysis Early with IAC involvement or neoplasms Late with slow growing mass Mastoid: CN IX neck pain Implications of Complex Anatomy Broad, non-specific presentations Clinical presentations NOT enough Imaging Studies Key CT- bone evaluation MRI T1 weighted – Fat hyperintense MRI T2 weighted – CSF/water hyperintense Implications of Complex Anatomy • Clinical presentations of these lesions, therefore, can be quite variable and depend largely on involvement of numerous intimately adjacent intra- and extracranial structures, especially the cranial nerves. • Given this variability, petrous apex lesions cannot be diagnosed accurately on the basis of clinical findings alone. • Fortunately, many of these lesions have characteristic MRI and CT appearances that can often allow a precise diagnosis. Outline I. II. III. IV. V. VI. VII. Anatomy Clinical Presentation Common Lesions Cholesterol Granulomas Surgical Approaches Outcomes References Razek AA, Huang BY. Lesions of the Petrous Apex: Classification and Findings at CT and MR Imaging. RadioGraphics 2012; 32:151–173 Lesion CT T1 Weighted MRI T2 Weighted MRI Enhancement PA Effusion 1. Bony preservation 2. Intact trabeculae Hypointense Hyperintense No Mucocele 1. Hypodense 2. Expansile smooth border 3. Normal bony architecture Hypointense Hyperintense No Cholesteatoma 1. Loss of normal air cells 2. Non-enhancing 3. Isointense CSF Hypointense Hyperintense No Cholesterol Granuloma 1. Expansile smooth border 2. Occasional rim enhancement 3. Isointense with brain Hyperintense Hyperintense No Encephalocele Smooth bony erosion Hypointense Hyperintense No Bone Marrow Non-expansile Hyperintense Hypointense No Lesion CT T1 Weighted MRI T2 Weighted MRI Enhancement PA Effusion 1. Bony preservation 2. Intact trabeculae Hypointense Hyperintense No Mucocele 1. Hypodense 2. Expansile smooth border 3. Normal bony architecture Hypointense Hyperintense No Cholesteatoma 1. Loss of normal air cells 2. Non-enhancing 3. Isointense CSF Hypointense Hyperintense No Cholesterol Granuloma 1. Expansile smooth border 2. Occasional rim enhancement 3. Isointense with brain Hyperintense Hyperintense No Encephalocele Smooth bony erosion Hypointense Hyperintense No PA Effusion The petrous apex air cell system may develop an effusion associated with an upper respiratory tract infection. This may be apparent in an asymptomatic patient who has a MRI for an unrelated condition. PA Effusion PA Effusion Petrous apex effusions are non-enhancing, non-expansile, petrous apex lesions which demonstrate Fig. 3. Radiological imaging of petrous apex effusion. (a)Axial computed tomography image showing preservation of intact trabeculae (arrows); distinguish from CG (b)Axial, T1-weighted magnetic resonance imaging (MRI) showing a non-expansile lesion with low signal intensity. (c)Axial, T2-weighted MRI showing a non-expansile lesion with high signal intensity. (d)Axial, T1-weighted, post-contrast MRI showing a nonenhancing lesion. PA Effusion The petrous apex air cell system may develop an effusion associated with an upper respiratory tract infection. This may be apparent in an asymptomatic patient who has a MRI for an unrelated condition. Lesion CT T1 Weighted MRI T2 Weighted MRI Enhancement PA Effusion 1. Bony preservation 2. Intact trabeculae Hypointense Hyperintense No Mucocele 1. Hypodense 2. Expansile smooth border 3. Normal bony architecture Hypointense Hyperintense No Cholesteatoma 1. Loss of normal air cells 2. Non-enhancing 3. Isointense CSF Hypointense Hyperintense No Cholesterol Granuloma 1. Expansile smooth border 2. Occasional rim enhancement 3. Isointense with brain Hyperintense Hyperintense No Encephalocele Smooth bony erosion Hypointense Hyperintense No Bone Marrow Non-expansile Hyperintense Hypointense No Petrous apex mucoceles • Petrous apex mucoceles are uncommon. Similarly to mucoceles found elsewhere in the head and neck, they are most likely caused by postinflammatory obstruction of a pneumatized petrous apex air cell. • An obstructed air cell containing respiratory epithelium that maintains its ability to secrete mucous. • The continued production and accumulation of mucoid material within the obstructed air cell, along with the associated inflammatory response: expansion, remodeling, and ultimately permeative erosion or destruction of the bony margins. • CT of mucoceles shows a smoothly expansile bone lesion that may cause septal erosion and can be difficult to distinguish from a cholesterol granuloma. Mucocele Mucocele CT of mucoceles shows a smoothly expansile bone lesion that may cause septal erosion and can be difficult to distinguish from a cholesterol granuloma. Radiological imaging of petrous apex mucocele. (a) Axial, T1-weighted magnetic resonance imaging (MRI) showing bilateral petrous apex mucoceles exhibiting smooth expansion and low signal intensity. (b) Axial, T2-weighted MRI showing bilateral petrous apex mucoceles with characteristic high signal intensity (isointense to fluid). (c) Axial, diffusion-weighted MRI showing that these lesions are not diffusion-restricted, which distinguishes them from petrous apex epidermoids. Lesion CT T1 Weighted MRI T2 Weighted MRI Enhancement PA Effusion 1. Bony preservation 2. Intact trabeculae Hypointense Hyperintense No Mucocele 1. Hypodense 2. Expansile smooth border 3. Normal bony architecture Hypointense Hyperintense No Cholesteatom a 1. Loss of normal air cells 2. Non-enhancing 3. Isointense CSF Hypointense Hyperintense No Cholesterol Granuloma 1. Expansile smooth border 2. Occasional rim enhancement 3. Isointense with brain Hyperintense Hyperintense No Encephalocele Smooth bony erosion Hypointense Hyperintense No Bone Marrow Non-expansile Hyperintense Hypointense No Petrous apex cholesteatomas Petrous apex cholesteatomas and epidermoids make up 4%–9% of all petrous apex lesions. • Cholesteatomas may be classified as acquired or congenital, with congenital cholesteatomas of the petrous apex being more common. • Congenital cholesteatomas arise from aberrant ectoderm that is trapped during embryogenesis; at histologic analysis, they consist of cysts lined with stratified squamous epithelium and filled with keratinous debris • • These lesions classically occur in children and young adults. Mafee MF, Kumar A, Heffner DK. Epidermoid cyst (cholesteatoma) and cholesterol granuloma of the temporal bone and epidermoid cysts affecting the brain. Neuroimaging Clin N Am 1994;4(3): 561–578. Cholesteatoma Cholesteatoma Radiological imaging of petrous apex epidermoid (right ear). (a) Axial computed tomography image showing an expansile lesion in the right petrous apex. (b) Axial, T1- weighted magnetic resonance imaging (MRI) showing an expansile lesion in the right petrous apex with low signal intensity. (c) Axial, T2-weighted MRI showing an expansile lesion in the right petrous apex with high signal intensity. (d)Axial, T1-weighted, post- contrast MRI showing a nonenhancing lesion. Lesion CT T1 Weighted MRI T2 Weighted MRI Enhancement PA Effusion 1. Bony preservation 2. Intact trabeculae Hypointense Hyperintense No Mucocele 1. Hypodense 2. Expansile smooth border 3. Normal bony architecture Hypointense Hyperintense No Cholesteatom a 1. Loss of normal air cells 2. Non-enhancing 3. Isointense CSF Hypointense Hyperintense No Cholesterol Granuloma 1. Expansile smooth border 2. Occasional rim enhancement 3. Isointense with brain Hyperintense Hyperintense No Encephalocele Smooth bony erosion Hypointense Hyperintense No Bone Marrow Non-expansile Hyperintense Hypointense No Cholesterol Granuloma Cholesterol Granuloma Radiological images of petrous apex cholesterol granuloma. (a)Axial computed tomography image showing erosion of trabeculae and smooth expansion in the petrous apex. (b)Coronal, T1-weighted, pre-contrast magnetic resonance imaging (MRI) showing a non-enhancing, expansile lesion in the petrous apex with high signal intensity. (c)Axial, T1-weighted, post- contrast MRI showing an expansile lesion with high signal intensity which does not enhance. (d)Axial, T2-weighted MRI showing an expansile petrous apex lesion with high signal intensity. Lesion CT T1 Weighted MRI T2 Weighted MRI Enhancement PA Effusion 1. Bony preservation 2. Intact trabeculae Hypointense Hyperintense No Mucocele 1. Hypodense 2. Expansile smooth border 3. Normal bony architecture Hypointense Hyperintense No Cholesteatom a 1. Loss of normal air cells 2. Non-enhancing 3. Isointense CSF Hypointense Hyperintense No Cholesterol Granuloma 1. Expansile smooth border 2. Occasional rim enhancement 3. Isointense with brain Hyperintense Hyperintense No Encephalocele Smooth bony erosion Hypointense Hyperintense No Bone Marrow Non-expansile Hyperintense Hypointense No Encephalocele Encephalocele Radiological imaging of petrous apex cephalocoele. (a) Axial computed tomography image showing bilateral smooth erosion extending from Meckel’s cave to the petrous apex. (b) Axial, T1-weighted, pre-contrast magnetic resonance imaging (MRI) showing bilateral lesions isointense to cerebrospinal fluid (CSF) (low-signal intensity). (c) Axial, T2-weighted MRI showing bilateral lesions isointense to CSF (high signal intensity). (d) Axial, T1- weighted, post-contrast MRI showing bilateral lesions which do not enhance. (e) Axial, constructive interference in the steady state (‘CISS’) MRI focused on the right petrous apex cephalocoele, showing a lesion isointense to CSF. (f) Axial, constructive interference in the steady state MRI focused on the left petrous apex cephalocoele, showing the trigeminal nerve embedded within the cephalocoele. Lesion CT T1 Weighted MRI T2 Weighted MRI Enhancement PA Effusion 1. Bony preservation 2. Intact trabeculae Hypointense Hyperintense No Mucocele 1. Hypodense 2. Expansile smooth border 3. Normal bony architecture Hypointense Hyperintense No Cholesteatoma 1. Loss of normal air cells 2. Non-enhancing 3. Isointense CSF Hypointense Hyperintense No Cholesterol Granuloma 1. Expansile smooth border 2. Occasional rim enhancement 3. Isointense with brain Hyperintense Hyperintense No Encephalocele Smooth bony erosion Hypointense Hyperintense No Bone Marrow Non-expansile Hyperintense Hypointense No Bone Marrow Bone Marrow Radiological imaging of petrous apex marrow. (a) Axial computed tomography image showing a non-expansile lesion in the left petrous apex. (b) Axial, T1-weighted, pre-contrast magnetic resonance imaging (MRI) showing a left-sided lesion isointense to fat (bright signal). (c) Axial, T2-weighted MRI showing a left-sided lesion isointense to fat (dark signal). (d)Axial, T1-weighted, post-contrast MRI with fat suppression, showing suppression of the fat signal in the marrow. Cholesterol Granuloma Composition Cystic lesions containing cholesterol crystals surrounded by Foreign body giant, fibrous tissue reaction, Chronic inflammation More liquid in nature Cyst wall: Fibrous connective tissue NOT keratinizing squamous epithelium (cholesteatoma) Therefore complete excision not necessary Cholesterol Granuloma Most common lesion of PA 30x less common than acoustic neuroma Etiology Theory 1 (older): Obstruction-vacuum hypothesis Theory 2 (new): Exposed Marrow hypothesis Jackler 2003, Hoa 2012 Problems with the Classic (Obstruction-Vacuum) Hypothesis: Impaired ventilation of mucosalined pneumatic tracts in the middle ear, mastoid, paranasal sinuses, and lung are very common, but CG is rare. The extraordinary levels of temporal bone pneumatization typically observed in PA CG cases is indicative of excellent ventilation and freedom from inflammatory mucosal disease. Were underpressure due to gas absorption alone sufficient to trigger hemorrhage, CG ought to be frequent in otitis media with effusion. Jackler, RK. Cho, M. A New Theory to Explain the Genesis of Petrous Apex Cholesterol Granuloma. Otology & Neurotology:January 2003 - Volume 24 - Issue 1 - pp 96-106. Obstruction-Vacuum Hypothesis Temporal Bone Mucosal Swelling Resorption of Gas in Petrous Cavity Negative Pressure Hemorrhage into temporal bone air cells Degradation of Hemosiderin + Cholesterol • Temporal bone mucosal swelling + resorption of gas that is present • Negative pressure and hemorrhage into the temporal bone air cells • Degradation of hemosiderin and cholesterol which inflammatory granulomatous reaction Inflammatory Granulomatous Reaction Problems with Obstruction-Vacuum Hypothesis Impaired ventilation of mucosa-lined pneumatic tracts Extraordinary levels of t-bone pneumatization in PA CG cases Middle ear Mastoid Paranasal sinuses Lung indicative of excellent ventilation freedom from inflammatory mucosal disease If underpressure sufficient to trigger hemorrhage, why OME CG? Exposed Marrow Hypothesis PA Pneumatization Hematopoietic Marrow Budding Mucosa Bony Interface Hemorrhage Hemosiderin + Lipids PA Outflow Obstruction Substrate for CG Cyst Formation Jackler RK, Cho M. A new theory to explain the genesis of petrous apex cholesterol granulomas. Otol Neurotol. 2003; 24:96–106. Exposed Marrow Hypothesis As cellular tracts penetrate the apex during young adulthood, budding mucosa invades and replaces hematopoietic marrow. The bony interface becomes deficient, with coaptation of richly vascular marrow and the mucosal air cell lining. Hemorrhage from the exposed marrow coagulates within the mucosal cells and occludes outflow pathways. Sustained hemorrhage from exposed marrow elements provides the engine responsible for the progressive cyst expansion. As the cyst expands, bone erosion increases the surface area of exposed marrow along the cyst wall. This exposed marrow theory explains the unique proclivity of the healthy and well-pneumatized PA to form a CG. Marrow in the petrous apex serves as a source for both hemosiderin and lipids. Cholesterol crystals that result from both breakdown of these lipids within the marrow instigate an inflammatory reaction that is believed to be necessary for formation of these cysts (1,11). Some have suggested that the variability in aggressiveness of the cholesterol granuloma is related to the richness of the adjacent blood supply Hoa M, House J, Linthicum FH. Petrous Apex Cholesterol Granuloma: Maintenance of Drainage Pathway, the Histopathology of Surgical Management and Histopathologic Evidence for the Exposed Marrow Theory. Otol Neurotol. 2012 August ; 33(6) Hoa M, House J, Linthicum FH. Petrous Apex Cholesterol Granuloma: Maintenance of Drainage Pathway, the Histopathology of Surgical Management and Histopathologic Evidence for the Exposed Marrow Theory. Otol Neurotol. 2012 August ; 33(6) Hoa M, House J, Linthicum FH. Petrous Apex Cholesterol Granuloma: Maintenance of Drainage Pathway, the Histopathology of Surgical Management and Histopathologic Evidence for the Exposed Marrow Theory. Otol Neurotol. 2012 August ; 33(6) Clinical Presentation Most commonly asymptomatic, found due to work up of other problems (HA) Hearing loss (64.7%), vestibular symptoms (56%), tinnitus (50%), headache (32.3%), facial twitching (23.5%), facial paresthesia (20.6%), otorrhea (11.8%), diplopia (5.9%), facial weakness (2.9%) Aggressive CG Type I: CN VIII involvement Type II: Superior PA SNHL + tinnitus Followed by vertigo + dizziness HA + facial pain Middle + posterior fossa dural irritation Type III: Meckel’s Cave CN V or CN VI Possible OM from ET compression Mosnier I, Cyna-Gorse F, Grayeli AB, Fraysse B, Martin C, Robier A et al. Management of cholesterol granulomas of the petrous apex based on clinical and radiologic evaluation. Otol Neurotol 2002;23:522–8 Aggressive CG • • • First type, sensorineural hearing loss and tinnitus are the commonest presenting symptoms, followed by vertigo and dizziness. In such cases, involvement of the vestibulocochlear nerve is typical. Second type is related to a cholesterol granuloma located in the superior part of the petrous apex, in which compressional symptoms such as headache and facial pain are the principal features; this type is related to middle and posterior fossa dural irritation. Third type: involvement of either the trigeminal or the abducens nerve, signifying compression of the Meckel’s cave region. Rarely, recurrent otitis media can be a feature, indicating pressure on the eustachian tube. Mosnier I, Cyna-Gorse F, Grayeli AB, Fraysse B, Martin C, Robier A et al. Management of cholesterol granulomas of the petrous apex based on clinical and radiologic evaluation. Otol Neurotol 2002;23:522–8 Park KC, Wong G, Stephens JC, Saleh HA. Endoscopic transsphenoidal drainage of an aggressive petrous apex cholesterol granuloma: unusual complications and lessons learnt. The Journal of Laryngology & Otology (2013), 127, 1230–1234. To Drain or Not to Drain? Solid tumors + cholesteatoma Goal of Drainage? Sx = surgical; no symptoms = non-surgical Controversial Natural hx not well defined for small cysts Drain large lesions or sx’s CN involvement Delaying surgery in presence of sx’s = no real advantage • Solid tumors/cholesteatoma removed when first identified, rather than after symptoms develop b/c these symptoms frequently reveal further involvement of other vital structures • Drainage: establish outflow drainiage pathway that is maintained so that CG expansion does not result in recurrence of patient symptoms • Sx = surgical, no symptoms (still controversial, b/c symptoms can be cuased by other things, ie non-specific HA) = nonsurgical • Natural hx not well defined for small cysts • Drain large lesions or sx’s pain/visual changes, diplopia, hearing loss, vertigo, facial nerve weakness • Delaying surgery in presence of symptoms offers no real advantage Outline I. II. III. IV. V. VI. VII. Anatomy Clinical Presentation Common Lesions Cholesterol Granulomas Surgical Approaches Outcomes References Surgical Approaches Serviceable Hearing: Air cells + otic capsule Above Below MCF approach: pros/cons Attic Root of zygomatic arch Infralabyrinthine Infracochlear Anterior Non-serviceable hearing: translabyrinthine Infratemporal fossa A/B/C Approaches Endoscopic Transphenoidal Petrous Angle: 10-20 degrees Good for patients in which there is space between medial wall of cyst and lateral wall of paraclival ICA CI in patients where cysts are hidden behind ICA Shoman, N. Donaldson, AM Ksiazek, J, Pensak, ML, Zimmer, LA. First Stage in Predicative Measure for Transnasal Transsphenoidal Approach to Petrous Apex Cholesterol Granuloma. Laryngoscope, 123:581–583, 2013 Approaches – Endoscopic Transphenoidal • Feasablity of endoscopic approach is based on petrous angle (angle centered at vomer, extending between medial aspect of the C3 segment of ICA and occipital protuberance) • Majority of temporal bones have petrous angle 10-20 degrees (82.8%) Neal 2013 Outline I. II. III. IV. V. VI. VII. Anatomy Clinical Presentation Common Lesions Cholesterol Granulomas Surgical Approaches Outcomes References Outcomes Successful Tx: absence of growth + improvement in symptoms Open: largest study 82%, smaller studies 90-100% Symptoms improvement 90% (71/79, 6 studies) Recurrence 12.5% (15/120, 9 studies) Complication rate: 24.3% (n=115, 9 studies) Hearing loss/CSF leak Endoscopic: resolution rate 98.5%, complication rate 13.2%, Restenosis 20% (9/45), most common epistaxis, 1 CSF leak symptomatic/recurrence 7.5% (4/45) Stent: 45% (23/45) 1/23 developed symptoms after (4.3%) As opposed 10.7% if non-stented Outcomes Absence of continuous growth in combination with an improvement in symptoms Eytan DJ, Kshettry VR, Sindwani R, Woodard TD, Recinos PF. Surgical outcomes after endoscopic management of cholesterol granulomas of the petrous apex: a systematic review. Neurosurg Focus 37 (4):E14, 2014 Outcomes Successful Tx: absence of growth + improvement in symptoms Endoscopic: resolution rate 98.5%, complication rate 13.2%, most common epistaxis, 1 CSF leak Restenosis 20% (9/45), symptomatic/recurrence 8.8% (4/45) Stent: 51%% (23/45) 1/23 developed symptoms after (4.3%) As opposed 10.7% if non-stented P = 0.6 Outcomes • Absence of continuous growth in combination with an improvement in symptoms • Stent more likely to be placed in narrow drainage pathway; sample bias? Outcomes CN affected for short period have better prognosis Follow up MRI of CG shows cyst remains full of fluid but hypointense T1, return of hyperintense T1 suggest inadequate drainage in a symptomatic lesion Radiologic characteristics = successful long term drainage Stable size- maximal diameter Presence of cyst aeration Placement of drainage stent ***sx recurrence can occur with re-accumulation within cysts w/o enlargement; therefore stable size may not be best Outcomes • CN affected for short period have better prognosis • Follow up MRI of cholesterol granuloma shows cyst remains full of fluid but hypointense T1, return of hyperintense T1 suggest inadequate drainage in a symptomatic lesion • Lesion size, resolution of patient symptoms, occurrence of complications and presence of aeration have been reported • Most common cause of recurrence is obstruction of the drainage site by fibrous tissue Long Term Lesion size, resolution of patient symptoms, occurrence of complications, and presence of aeration have been reported Most common cause of recurrence is obstruction of the drainage site by fibrous tissue Revision rate of surgery 41% (7/17) 18% revision with stent (2/11) 83% revision w/o stent (5/7) p=.035 Post-operative Imaging Magnetic resonance imaging characteristics of petrous apex cholesterol granuloma: Left Image: drainage catheter leading from the petrous apex cholesterol granuloma cyst cavity to the middle-ear cavity, on coronal, T2-weighted image. Hoa M, House J, Linthicum FH. Petrous Apex Cholesterol Granuloma: Maintenance of Drainage Pathway, the Histopathology of Surgical Management and Histopathologic Evidence for the Exposed Marrow Theory. Otol Neurotol. 2012 August ; 33(6) Final Thoughts Lesions of PA present broadly Imaging key to dx CG can be incidental findings Operate on CG only if large OR sx’s of CN involvement Endoscopic management is safe option (anatomy) Stent placement may be beneficial Long term f/u with MRI Future works: mucosal flaps + gel foam Faculty Discussion: Dayton Young, MD - Page 1 Dr. Rana, that was a very good presentation, very thorough. I think you covered mostly, maybe all the aspects that would come up in this kind of a case. Petrous apex lesions are different from most lesions that you learn about in medicine. The diagnosis usually isn’t based on a biopsy, because it’s so hard to get to. It’s in the middle of the head. So we do rely a lot on imaging, and we know a lot about imaging. The two lesions that I think most about as I think back about patients I’ve seen are first of all, the very common cholesterol granuloma and the other one is bone marrow. So, these are things which you’ve got to be prepared to look for. You’ll be asked to interpret an image that’s been found during an otherwise normal scan, or in the diagnostic search for the cause of a headache. And you will have to explain that it’s normal bone marrow. Otherwise, that becomes the focus of the headache, and you want to avoid going down that pathway. The cases that you’re really going to be looking at are either really big or associated with some sort of neurological sign. Faculty Discussion: Dayton Young, MD - Page 2 The other place where I’ve seen these most often is in a postoperative mastoid. It’s not uncommon to go into a mastoid for a revision surgery and you find a cholesterol granuloma right there. And it’s probably based on blood products that were there from the original surgery. There’s often nothing to do about them - you end up draining them at the time. They are a characteristic brown color when you see them and usually make no difference clinically. Surgical approach - You described a number of surgical approaches, a lot of them had been tried earlier on back when Gradenigo’s syndrome was big and before antibiotics. A lot of these approaches were developed by people who were draining abscesses. The surgical approach will be different on every patient, usually based on the pneumatization of the temporal bone and the sphenoid sinus. If you have a sphenoid sinus that is well pneumatized and is abutting the petrous apex, it’s a straight shot into the petrous apex sometimes. Other times in the T-bone scan there’s a well pneumatized air cell tract right underneath the cochlea. Sometimes there’s plenty of space to do an infralabyrinthine approach and sometimes in front of the cochlea. It really does depend on the patient’s anatomy. The middle cranial fossa approach is probably the least favored approach. The drainage route would be a stent of some kind placed up underneath the dura and into the middle ear space. It doesn’t work well because it’s not dependent drainage. That was a good presentation. Thank you, Dr. Rana. References Chole, RA. “Petrous apicitis: surgical anatomy,” Annals of Otology, Rhinology and Laryngology, vol.94, no.3, pp. 254– 257,1985. Chapman PR, Shah R, Cure JK, Bag AK. Petrous Apex Lesions: Pictorial Review. AJR:196, March 2011 Razek AA, Huang BY. Lesions of the Petrous Apex: Classification and Findings at CT and MR Imaging. RadioGraphics 2012; 32:151–173 Mafee MF, Kumar A, Heffner DK. Epidermoid cyst (cholesteatoma) and cholesterol granuloma of the temporal bone and epidermoid cysts affecting the brain. Neuroimaging Clin N Am 1994;4(3): 561–578. Jackler RK, Cho M. A new theory to explain the genesis of petrous apex cholesterol granulomas. Otol Neurotol. 2003; 24:96–106. Mosnier I, Cyna-Gorse F, Grayeli AB, Fraysse B, Martin C, Robier A et al. Management of cholesterol granulomas of the petrous apex based on clinical and radiologic evaluation. Otol Neurotol 2002;23:522–8 Park KC, Wong G, Stephens JC, Saleh HA. Endoscopic transsphenoidal drainage of an aggressive petrous apex cholesterol granuloma: unusual complications and lessons learnt. The Journal of Laryngology & Otology (2013), 127, 1230–1234. Brackmann DE, Toh E. Surgical management of petrous apex cholesterol granulomas. Otol Neurotol 2002;23:529–33 Giddings NA, Brackmann DE, Kwartler JA, “Transcanal infracochlear approach to the petrous apex,” Otolaryngology— head and neck surgery, vol.104, no.1, pp. 29–36,1991. Shoman, N. Donaldson, AM Ksiazek, J, Pensak, ML, Zimmer, LA. First Stage in Predicative Measure for Transnasal Transsphenoidal Approach to Petrous Apex Cholesterol Granuloma. Laryngoscope, 123:581–583, 2013 Eytan DJ, Kshettry VR, Sindwani R, Woodard TD, Recinos PF. Surgical outcomes after endoscopic management of cholesterol granulomas of the petrous apex: a systematic review. Neurosurg Focus 37 (4):E14, 2014 Isaacson B, Kutz JW, Roland PS. “Lesions of the petrous apex: diagnosis and management,” Otolaryngologic Clinics of North America, vol. 40, no. 3, pp. 479–519, 2007. Lesions of the Petrous Apex Resident Physician: Nikunj A. Rana, M.D. Faculty Mentor/Discussant: Dayton Young, M.D. The University of Texas Medical Branch – UTMB Health Department of Otolaryngology Grand Rounds Presentation January 28, 2015 Series Editor: Francis B. Quinn, Jr., MD, FACS -- Archivist: Melinda Stoner Quinn, MSICS