PSYC 181: Drugs and Behavior Exam 1 Review Sheet
advertisement

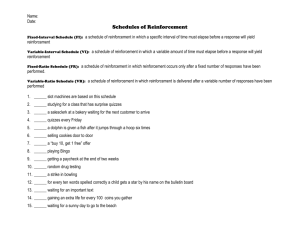
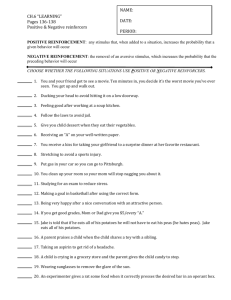
PSYC 181: Drugs and Behavior Exam 1 Review Sheet Smoking o The number one preventable cause of death o Approximately 430,000 people die from smoking-related illness in the U.S. each year (1/5 of all deaths) o 70% of smokers have tried to quit at least once; most quitters try 5 to 7 times before they succeed o Only 1 in 5 physicians receive training in smoking cessation; however there are few effective treatments for addiction Drug Abuse o Definition: The use of any drug in a manner that deviates from the approved medical or social patterns in a given culture. o Three criteria of drug abuse: 1. Pattern of pathological use 2. Impairment in social or occupational functioning caused by the pattern of pathological use 3. Duration of at least one month o Some drugs may be considered abused if used at all (e.g. heroin, ecstasy), or if used in one situation but not others o Some cultures may use drugs and not consider it abuse (peyote, bhang) o A lot of drug use falls outside the realm of medical use, such as non-medical drug use, experimental drug use, recreational use, and circumstantial use * Remember, drug abuse is not the same as drug addiction! Drug Addiction o Definition: A behavioral pattern of drug use, characterized by: Compulsive use Compulsive drug-seeking High tendency to relapse after withdrawal. o Addiction does not necessarily imply dependence (e.g. LSD) Names of Drugs o Brand, trade, proprietary e.g. Desoxyn o Generic, trivial, nonproprietary e.g. methamphetamine o Chemical name e.g. N,alpha-dimethylphenethylamine o Street name e.g. “ice” or “crank” Classes of Psychoactive Drugs o Opiates (narcotics): Similar to opium in composition or effect; has analgesic properties, causes sleepiness; e.g. morphine, heroin, codeine, hydrocodone (Vicodin), Dilaudid, Demerol o Depressants: Depress the Central Nervous System (CNS) Barbiturates: Seconol, Nembutal Benzodiazepines: diazepam (Valium), Ativan, flunitrazepam (Rohypnol), GHB o Stimulants: cocaine, amphetamine, methylphenidate (Ritalin), nicotine, caffeine o Hallucinogens: LSD, psylocin, psylocibin o Dissociative Anesthetics: PCP (phencyclidine), Ketamine o Cannabinoids: tetrahydrocannibanol (THC- marijuana) o Designer Drugs: MDMA (ecstasy). The drags have characteristics of both hallucinogens and stimulants History of Drug Abuse o Largely a man-made, corporate developed, government endorsed problem o The legal and social status of a drug is separate of the drug’s addictiveness; many illegal drugs do not produce addictiveness. o Drug addiction emerged in the U.S. with the use of morphine (derived from opium) during the Civil War (Soldier’s disease) Opium • Extracted from the unripe seed capsule of the poppy plant • Grows wild in Asia; most legal production is in India and Turkey • Contains morphine, codeine, nosapine (narcotin), papaverine, narceine, thebain, etc. o Stickney and Poor’s paregoric (mixture of opium and alcohol) o Mrs. Winslow’s Soothing syrup: used to calm children; contain 85mg of morphine per fluid ounce. o Products containing opium and other narcotics were required to pay a special tax on each bottle. Tax was paid by sealing the unopened bottle with a stamp. o Heroin was originally marketing by Bayer as a cough syrup without the nasty side effects of morphine (diacetylmorphine 2 acetyl groups added to morphine) o Cocaine toothache drops were popular with children and parents o Coca wine (cocaine fortified wines; popular before the temperance movement o Panacea (a “cure-all”); promoted to cure the opium or alcohol habit. o Pure Food and Drug Act (1906): regulated food, drugs, and drug claims, created the FDA o Harrison Tax Act (1914): opiates and cocaine were outlawed due to trade war with China o Boggs Amendment to the Harrison Act (1951): criminalized illicit drug use o Drug Abuse Control Act (1965): attempted to make addictive drugs illegal o Controlled Substances Act (1970): classified drugs into schedules: Schedule I: no medical use (heroin, LSD, marijuana) Schedules II to V: various restrictions on medical use, varies by state Schedule VI: some states use this classification for inhalants (glues and paints) and Sudafed Unscheduled: aspirin, Tylenol, etc. o Analogue Drug Act (1985) : passed power to make drugs illegal to the DEA o Date Rape Prohibition Act (2000 – 2001): outlawed GHB, Rohypnol Pharmaceutical Companies and Drug Development o The typical profit margin of a pharmaceutical company is three times that of any other industry represented by Fortune o Insomnia is the most the prevalent neuropsychological disorder, followed by migraines and depression o The U.S. is the only country with a “free pricing policy.” This results in higher profits as well as more research and development o Drug Development Outline: Discern unmet medical need Discover mechanism of action of disease Identify the target protein Screen known compounds against target Chemically develop promising leads Fine 1 or 2 potential drugs Toxicity; pharmacology Clinical trials Pharmacology o Definition: The branch of medicine that deals with the uses, effects and modes of actions of drugs o Drug: A substance that is used primarily to bring about a change in some existing process or state; be it psychological, physiological or biochemical. o Sources of psychoactive agents: Naturally Occurring • Ephedrine: extracted from mua hunag plant indigenous to China • Cocaine: from the leaves of the coca plant • Opium: extracted from the unripe seed pods of the opium poppy Semisynthetics • Heroin: made from morphine • LSD: from the fungi that grow on grain Synthetics • Methadone: synthetic opiate • Amphetamine: powerful stimulant Pharmacokinetics o Definition: The area of pharmacology dealing with the absorption, distribution, biotransformation, and excretion of drugs (a drug’s ability to get to its receptor). o Factors include route of administration, absorption and distribution, inactivation, and elimination: Route of administration: • Oral (via digestive system) • Parenteral injection: through the skin • Subcutaneous (sc): under skin (relatively slow) • Intramuscular (im): through muscle (slowest distribution) • Intravenous (iv): through vein (fastest distribution) • Intraperitoneal (ip): through the peritoneal cavity (relatively fast & easy) • Pulmonary absorption: inhalation (quick route to brain) • Topical application: applied externally on skin (really slow) • Half-life is the time for the plasma drug concentration to fall to half of its peak level; it varies as a function of route of administration and is a measure of how long a drug lasts • Effects of route of administration on rate of absorption are due to many factors: o Surface area available for absorption o Blood circulation at the site of administration o Amount of drug destroyed immediately o Extent of binding to inert substances Absorption and distribution: • Drug transport across membranes is the most important factor in achieving active dose at the site of action. • Mechanism of transport: passive diffusion (down concentration gradient); limited by: o Size and shape of drug o Lipid solubility of drug o Degree drug is ionized (charged) o More ionized → less lipid soluble → less absorption → less effect Degree of ionization: drugs are usually a weak acid or a weak base o Drugs that are weak acids ionize more in basic (alkaline) environments o Drugs that weak bases ionize more in acidic environments o A pH less than 7 is acidic. A pH greater than 7 is basic. o Drug must be able to survive low pH; digestive track has enormous surface area so drug may still get significant absorption • Blood brain barrier limits the ability of the drug to reach the brain Inactivation: metabolism (biotransformation) to inactive forms (liver major site) Elimination: expulsion of metabolites or unchanged drug by kidneys, lungs, sweat, saliva, feces, or milk (kidney major site) • Pharmacodynamics o Definition: The study of the biochemical effects of drugs and their mechanism of action (what a drug does when it reaches its receptor). o Receptors: The molecules a drug interacts with to initiate its biological effects (where the drug must bind in order to produce a pharmacological effect) To have an effect, the drug must reach its receptor o D + R = DR > pharmacological effect o Most drug receptor interactions involve non-covalent interactions that are reversible (drug associates and then rapidly dissociates) o Law of Mass Action/Dose-Effect Curve: D + R = DR* > effect The active complex (DR*) leads to a cellular response that is in proportion to the fraction of receptors occupied Drugs do not produce new or unique response but only modify the rate of ongoing cellular events The magnitude of a drug effect should be proportional to the number of receptors occupied by the drug (logarithmic relationship; 10 times as much drug to achieve just twice the effect) A drug should have a maximal effect when all receptors are occupied Overall relationship is described by the dose-effect curve; major characteristics are: • Potency [location (left to right) on a dose-effect curve] • Maximum effect: achieved when increase in dose produce no further increase in effect; drugs vary in their ability to produce an effect; they may act at different receptors and have more or less efficacy at the same receptor. o Potency How strong a drug is; depends on receptor accessibility, affinity, efficacy o o ED50 (Effective Dose) dose that produces an effect in 50% of a population LD50 (Lethal Dose) dose that kills 50% (aka TD = toxic dose) TI (Therapeutic Index) LD50/ED50 (lethal dose divided by effective dose) Safety Margin = LD50 – ED50 (lethal does minus the effective dose) Agonist: a drug that binds to receptor and has pharmacological effect Antagonist: drug that binds to receptor and has no direct biological effect, but blocks the action of an agonist or transmitter at that receptor o Competitive antagonist Binds to the same receptor as agonist Shifts dose-effect curve for agonist to the right Effect can be overcome by a sufficient dose o Noncompetitive antagonist: Shifts dose-effect curve to the right, but cannot be overcome with dosage (decreases maximum effect) Can bind irreversibly or reversibly to prevent agonist from binding Poisons are noncompetitive antagonists Tolerance and Sensitization o Tolerance: decreased response with repeated administration, or a higher dose is required to produce the original effect (dose-effect curve shifts to the right) o Cross tolerance: tolerance to one type of drug leads to tolerance to others (especially within same drug class, but can also occur across classes) o Sensitization: increased response with repeated administration, or a lower dose is required to produce the original effect (dose-effect cure shifts to the left) o Cross sensitization: sensitization to one type of drug leads to sensitization to others (often seen in stimulants; e.g. sensitization to cocaine may result in sensitization to amphetamine) o Tolerance and sensitization may involve pharmacokinetic (dispositional) changes, pharmacodynamic changes (neuroadaptation), or behavioral factors (learning). Behavioral Pharmacology o Definition: The study of the relationship between the physiological actions of drugs and their effects on behavior and psychological function. o Drugs alter the probability of the occurrence of behaviors; they do not create new behaviors o The behavioral effects of drugs are due to interactions amongst the pharmacological actions and drugs, the state of the organism (“set”) and the surrounding environmental circumstances of drug administration (“setting”) o Evaluation of behavioral effects of drugs: Primary evaluation unconditioned effects on behavior: • Motor activity • Seizures • Eating and drinking Secondary evaluation tests of more specific functions: • Either unconditioned or conditioned (learned) • Analgesia • Learning and memory: o Spatial Radial Maze task o Morris Water Maze test o Augmented Startle Response o Nonrecurring-Items Delayed Nonmatching-to-Sample Test o Anxiety (Elevated Plus Maze) • • Schedules of reinforcement: o Positive Reinforcement: presentation increase the probability of the preceding behavior o Negative reinforcement: removal increases the probability of the preceding behavior o Punishment: decrease the probability of a behavior o Ratio schedules: reinforcement is based on the number of response made: Fixed ratio (e.g. FR10 = reinforcement is given after every 10 responses) Variable ratio (e.g. VR10 = reinforcement is given after an average of 10 responses) Continuous reinforcement (FR1): reinforcement is given for every response o Interval schedules: reinforcement of a behavior is based on the amount of time that has elapsed since the last reinforcement” Fixed interval (e.g. FI5 reinforcement is given after 5 minutes) Variable interval (e.g. VI5 = reinforcement is given after an average of 5 minutes) * produces the steadiest response o Differential reinforcement of low rate schedules (DRL): reinforcement is given after a fixed amount of time, but if a response is made before the time is up, the “clock resets” Operant procedures are used for two reasons: o To question the stimulus properties of drugs (“what it feels like”) o To question the reinforcing/incentive properties of drugs (“will you work for it?”) o Drugs as discriminative stimuli (SD) SD = The stimulus that signals availability of reinforcement; animals learn to respond when the appropriate SD is present • Drugs can serve as an SD • SD is related to the interoceptive cues of drug • • Method: “ask” animals about the interoceptive cues associated with various drugs. E.g. a rat presses the left lever if on morphine and receives food. Rat also receives food if presses right lever if given saline. If the drug is like morphine, the rat will press the left lever. Using these discrimination techniques, animals can help to classify drugs just like humans