Cardiac Rhythms

Kingston General Hospital
May 2008
In
INDEX
Introduction
Cardiac Conduction System
Introduction to Cardiac Monitoring
Recording Electrical Events
Waves of the ECG Complex
Intervals and Segments
Rhythm Regularity
Measurement of Heart Rate
Systematic Analysis of Rhythm Strips
Describing Rhythms
Normal Sinus Rhythm
Arrhythmias- Patient Assessment
Arrhythmias originating in the sinus node
Junctional Rhythms
Ventricular Rhythms
Atrial Arrhythmias
Atrio-ventricular blocks
Practice Strip Answers
References
Page 2
Page 3
Page 5
Page 9
Page 10
Page 16
Page 22
Page 23
Page 25
Page 26
Page 27
Page 28
Page 29
Page 33
Page 37
Page 42
Page 45
Page 52
Page 56
INTRODUCTION
The electrocardiogram (ECG or EKG) is a recording of the electrical activity of the heart.
The heart has it’s own electrical or conduction system.
Normally the electrical signals are initiated and travel through the heart’s conduction system in a specific order. This is accomplished by a process known as depolarization
. The pathway receiving the electrical stimulus is negatively charged (polarized). It must be made positive so that the impulse can be conducted. This process is called depolarization. These cells later recharge or repolarize in preparation for receiving the next electrical impulse. As depolarization and repolarization occur, certain electrical signals are seen on the ECG.
This learning guide will help you identify those signals on the ECG.
The patient will be hooked up to an ECG monitor that is at the bedside (hardwire), or a battery operated system (telemetry). Telemetry(softwire) is a portable box that is worn
by the patient , and the rhythm is displayed centrally at the nursing desk.
CARDIAC CONDUCTION SYSTEM
The heart has both electrical and mechanical properties.
The electrical event occurs first followed by the mechanical event.
Normal electrical conduction:
•the cardiac impulse begins in the sinoatrial (SA) node and travels to the right and left atria
•the atria depolarize and generate the p wave on the electrocardiogram
•the conduction then travels to the atrioventricular (AV) node where the conduction speed is reduced
•conduction then speeds up and travels down the Bundles of His, and the right and left bundle branches to the Purkinje fibers
•the Purkinje fibers distribute the impulse rapidly and uniformly and ultimately depolarize the ventricular myocardium- this generates the QRS wave on the electrocardiogram
Mechanical Events:
•after the P wave is generated the atria contract. This contraction contributes 20% of the blood flow to the ventricle. This is called atrial kick
•after the QRS wave is generated the ventricles contract
•the reduction in depolarization speed at the AV node allows time after the atrial mechanical contraction for the ventricles to fill before they contract.
CARDIAC CONDUCTION SYSTEM
Escape rhythms
Automatic Cardiac Tissues
There are different conduction tissues in the heart that can act as pacemakers and initiate the electrical sequence. These are: SA node, atrial tissues, AV node, and the ventricles.
These tissues each have their own intrinsic or pre-set rate. Normally the SA node initiates the electrical sequence because it has the highest intrinsic rate. If the SA node cannot sustain this rate for some reason, the pacemaker with the next highest rate would then take over as the pacemaker of the heart. This is called an escape rhythm and is the heart’s emergency pacing system.
It is very uncommon to see an atrial escape rhythm , even though they are the next pacemaker in line. The AV node (junction) is the pacemaker that most often escapes
when the SA node fails.
INTRODUCTION TO CARDIAC MONITORING
The ECG monitor:
The patient must be attached to a heart monitor in order to see the electrical signals from the heart. This is done by applying electrodes (sticky sensors) to the patient’s
skin. Wires attached to a cable are snapped on to the electrodes. The cable is attached to the monitor. A signal will now appear on the monitor.
Monitoring Guidelines:
1) Electrodes:
•prepare skin- shave if required, cleanse with alcohol and abrade skin with backing on electrode
•electrodes will dry out over time:
•change if monitor signal is poor or patient is complaining of itchiness underneath electrode
•use new unopened package of electrodes each time
2) Documentation:
•6 second monitor strips are placed on the chart on each shift and when arrhythmias are detected
•evaluation of the rhythm strip by the nurse is documented with the strip
*pt’s name and CR number on strip
*do not tape over important information- it will fade and disappear over time
INTRODUCTION TO CARDIAC MONITORING
The electrodes detect the heart’s electrical activity.
There may be 3 or 5 electrodes attached to your patient.
Placement of electrodes :
•RA-right arm-below right clavicle
•LA-below left clavicle
white
black 3 lead 5 lead
•LL-left leg-left lower rib cage or abdomen red
•RL-right lower rib cage or abdomen green
•C- 5 th ICS anterior axillary line brown
3 lead system: RA LA and LL electrodes
•these electrodes form a triangle around the heart
•you can choose to monitor leads I, II, or III with a 3 lead system-these are called limb leads
5 lead system: RA LA LL RL C electrodes
•the C electrode can be positioned in any one of 6 designated positions on the left anterior chest- these are called the V1-V6 positions and are called chest leads
•the RL electrode is a ground electrode and is not used as a recording electrode
•with a 5 lead system you can choose to monitor leads I,II,III,aVR,, aVL , aVF , V1-V6
INTRODUCTION TO CARDIAC MONITORING
The electrical activity is picked up between 2 electrodes. A different pair is used to record each lead. One electrode is considered negative and one positive. It is the positive one that is recording the electrical activity.
•Lead 1- uses the RA (neg) and LA (positive ) for electrical recording
•Lead 2 -uses the RA(neg) and LL(positive) for recording
•Lead 3-uses the LA(now neg) and LL (positive) for recording
•These limb leads record the electrical conduction of the heart from three different viewpoints. They are called bipolar leads because they use a pair of electrodes to
record the activity
Remember it is the positive electrode that records the heart’s electrical activity- think of the positive electrode like a camera, watching the electrical activity of the heart.
• The electrical activity of the heart remains the same but each lead views this activity from a different angle.
INTRODUCTION TO CARDIAC MONITORING
• Recording the electrical waves:
•an upward deflection will be recorded on the monitoring paper if the conduction goes towards the positive electrode
•a downward deflection will be recorded on the monitoring paper if the conduction goes away from the positive electrode
• Lead 2 - the positive electrode is the LL which is positioned just below the heart
•normal conduction in the heart is down and to the left, therefore Lead 2 will pick up the conduction (or depolarization) coming towards it -the waves will be recorded as upright on the monitoring paper
•Lead 2 is the limb lead usually used in monitoring
RECORDING ELECTRICAL EVENTS
The recording paper is graph paper which records at a specific speed.
The horizontal lines measure the amplitude of events in millimeters or millivolts
One horizontal line measures 1 mm
The vertical lines measure the duration in seconds of any events.
Between 2 vertical lines the measure is .04 of a second. This is called a small box.
You’ll notice that every 5th vertical line is bolded. This is called a large box and measures .04x5= .20 of a second.
The next section discusses what events will be seen on the recording paper.
WAVES OF THE ECG COMPLEX
The P wave represents the depolarization of the atria. Atrial depolarization begins in the SA node and spreads through both atria.
The p wave is small, rounded and usually upright.
Atrial repolarization is usually not seen on the ECG because it is hidden in the subsequent QRS waveform and is of low voltage.
WAVES OF THE ECG COMPLEX
The largest wave in the ECG is the QRS complex.
The electrical impulses spreading through the ventricles produce the QRS complex.
Therefore the QRS represents ventricular depolarization.
Normal QRS duration (interventricular conduction time )is .
05-.10 seconds
Abnormal QRS duration is > .12 seconds .
•Indicates that conduction has been delayed in the ventricles
Q wave
•the first downward wave of the QRS complex
• precedes the R wave
•often absent on the ECG
R wave
•the first upward wave of the QRS complex
•an upward wave is always called an R wave
•a second upward wave is called an R prime ( R’)
S wave
•the downward wave following the R wave
An upward wave is always called an R wave
The downward wave before the R is called the Q wave
The downward wave after the R wave is called the S wave
Ventricular contraction following the QRS creates the pulse.
WAVES OF THE ECG COMPLEX
A B
2 small squares= .08 seconds NORMAL
A
2 small squares= .08 seconds NORMAL
B
3 ½ small squares= .14 seconds WIDE
WAVES OF THE ECG COMPLEX
Even though we call this complex the QRS complex, not all QRS complexes have all three components.
The examples above illustrate different QRS complexes and the names of all the components.
WAVES OF THE ECG COMPLEX
The T wave represents ventricular repolarization or recovery.
The T wave follows the QRS and is smooth and rounded. It is usually upright.
Inverted T waves:
If a T wave is upside down (inverted) this is usually an abnormal finding.
It can indicate myocardial ischemia.
Notched or pointed T waves:
Heavily notched or sharply pointed T waves in adults may indicate MI or pericarditis.
Tall T waves:
Tall T waves suggest an MI or hyperkalemia
If any of the above are new findings on the monitor a 12 lead ECG should be done
PRACTICE YOUR Ps and Qs!
P
QRS
T
P
QRS
T
P
QRS
T
P
QRS
T
P
T
P
QRS
T
P
QRS QRS
T
P
T
P
QRS
T
P
QRS
T
P
QRS
INTERVALS AND SEGMENTS
This is the segment between the P wave and the QRS.
•This represents the time interval between when the atria depolarize and when the ventricles depolarize. The electrical impulse is spreading to the AV node, Bundle of His and Purkinje fibers.
•This is considered a baseline from which we measure changes in the ST segment.
INTERVALS AND SEGMENTS
The PR interval is measured from the beginning of the P to the beginning of the QRS.
If there is no Q wave then it is measured from the beginning of the P wave to the beginning of the R wave.
• It represents atrial and atrioventricular conduction time. This includes atrial depolarization, the normal conduction delay in the AV node, and the passage of the electrical impulse through the bundle of His and the bundle branches.
•If conduction is occurring normally then this will take between 0.12 and .20 of a second or 3 to 5 small boxes
• Short P-R interval:
•AV conduction time is shortened: could be due to:
•initial impulse in the junction (AVnode) or
•another (faster)conduction pathway betweeen atria and ventricles
• Long P-R interval:
•AV conduction time is longer than normal: could be due to:
•a conduction delay in the AV junction
•a conduction delay through the atria
INTERVALS AND SEGMENTS
The ST segment is the segment after the QRS and before the T wave.
This segment represents ventricular repolarization.
Normal ST segment :
•horizontal and flat
•level with the PR segment or baseline
• J point :
•the junction between the ST segment and the QRS is called the J point
If the ST segment is more than 1 mm (1 small square) above the baseline it is considered elevated
If the ST segment is more than 1 mm below the baseline for .08 seconds
(2 small squares) after the J point, it is considered depressed
• ST depression:
•The ST segment falls below the baseline for .08sec (2 small squares) past the J point
•indicates myocardial ischemia
• ST elevation:
•The ST segment is above the baseline
•acute ST elevation indicates myocardial injury
•prolonged ST elevation may indicate something other than myocardial injury: pericarditis, ventricular aneurysm or cardiac contusion
If any of the above are new findings on the monitor a 12 lead ECG should be done
Intervals and Segments
The QT interval is measured from the beginning of the QRS until the end of the T wave.
•The QT interval represents ventricular depolarization and repolarization.
• Normal QT interval:
• usually between 0.36 and 0.44 second
• varies greatly according to age, gender ,heart rate, and whether the patient is asleep
• should be less than 1/2 the distance between two consecutive R waves (R-R interval) when the rhythm is regular
Prolonged QT interval:
Repolarization means that the muscle cell resets itself so it can depolarize again.
Measured on an ECG, the time between the Q wave and the T wave is prolonged in this condition. This leads to a longer vulnerable period. If the next QRS begins before the end of repolarization, an arrhythmia or irregular heart beat could occur, such as ventricular fibrillation, or Torsades de Pointes which could be fatal. This condition is diagnosed on a 12 lead ECG.
A 12 lead ECG should be done if the QT appears prolonged
•Cause:congenital, medications (Amiodarone, Haldol, Procainamide,Sotalol, some antibiotics ), hypokalemia and hypomagnesemia, intracranial or subarachnoid hemorrhage
Intervals and Segments
PR
PR
PR
J point
ST
ST
ST
QT
QT
QT
PR =.16 sec NORMAL
ST -depressed 1mm for .08 sec past the J point-ABNORMAL
QT- less than ½ the R -R
NORMAL
PR = .32 sec PROLONGED
ST - slightly depressed, but not
1mm- baseline-NORMAL
QT- less than ½ the R-R
NORMAL
PR = .20 seconds NORMAL
ST - baseline-NORMAL
QT - more than ½ the R-R
PROLONGED
RHYTHM REGULARITY
Rhythm Regularity:
• Refers to the regularity of the QRS complexes
•
Measure the distance between the QRS complexes-this is referred to as the R-R interval
There are three ways to describe regularity:
Regular rhythms
•
R-R intervals are all the same or vary slightly.
• In regular rhythms the QRSs usually look alike
Regular but interrupted
• Most of the R-R intervals are constant
• Interrupted by premature beats or a pause
Irregular
•
R-R intervals vary
•
Not due to premature beats or pauses, but because the actual rhythm is irregular
MEASUREMENT OF HEART RATE
1
3 seconds
2 3 4
6 seconds
5 6
6 SECOND METHOD
To determine HR:
•
There are small line markers on the top of the graph paper
• These occur every 3 seconds
Count # of QRS complexes in a 6 second strip.
Multiply by 10.
Above example:
QRS’s in 6 seconds = 6
6 X 10 = 60 beats/min
MEASUREMENT OF HEART RATE
How to calculate the heart rate on ECG paper
300
150
100
75
60
50
43
37
33
30
1 big box BIG BOX METHOD
Alternate method to determine HR (for regular rhythms only)
• There are 300 big boxes in one minute
•
If there was one big box between each QRS the HR would be 300 / minute
•
If there were 2 big boxes between each QRS the HR would be 300/2=
150/min
• Try to find a QRS on a bolded line
• Count the number of big boxes to the next QRS
• Divide into 300
SYSTEMATIC ANALYSIS OF RHYTHM STRIPS
The key to identifying rhythms correctly is to systematically analyze the cardiac rhythm strip.
1. Determine the atrial and ventricular rate (HR)
If these rates are different then you know to look more closely a the relationship between the p and the QRS
2. Measure R-R. a. Is the rhythm regular, regular but interrupted, or irregular?
3. P waves a. Are they present and do they all look the same? b. Is there a QRS after each one?
4. PR interval a. Normal is .12-.20 seconds (3-5 small boxes) b. Is each PR interval the same?
5. QRS duration a. Normal is <.12 seconds or 3 small boxes b. Are they all the same and point in the same direction?
6. Examine the ST segment a. Is it at baseline (even with the PR segment) b. Is there ST elevation or ST depression?
7. Examine the T waves a. Normal is upright and rounded b. Are they inverted or flattened
8. Measure the QT interval a. Normal is < ½ the R-R interval b. Is it changed from previously
9. Are there premature beats.
a. Is there a p in front of the QRS?
10. b. Is the QRS normal or widened?
Analyze the rhythm.
Rhythms are always described by the above format.
The first part of the description tells us where the rhythm originates.
The second part of the description tells us how fast the rhythm is.
Examples:
Sinus bradycardia:
•
The rhythm originates in the sinus node and the rate is < 60 beats per minute
Ventricular tachycardia:
•
The rhythm originates in the ventricles and the rate is > 100 beats per minute
NORMAL SINUS RHYTHM
Normal Sinus Rhythm
Sinoatrial node
Rhythm
Regular
Rate
(per minute)
60 -100
P wave
Upright
Uniform
PRI
(seconds)
0.12-0.20
QRS
(seconds)
0.06-0.10
The only rhythm that is considered normal is normal sinus rhythm.
Mechanical events are optimal in normal sinus rhythm.
An arrhythmia is any cardiac rhythm that is not normal sinus rhythm.
Arrhythmias fall into the following categories:
•
Arrhythmias originating in the sinus node
•
Junctional rhythms
•
Ventricular rhythms
•
Atrial arrhythmias
•
AV conduction disturbances
ARRYTHMIAS- PATIENT ASSESSMENT
Arrhythmias can occur for a number of reasons.
If the patient is symptomatic, then there must be immediate intervention
Guide your nursing assessment with the following questions:
1. Is the patient oxygenating well? a. Check the O
2
saturation
2. Is there evidence of ischemia ?
b. Is the patient having chest pain? c. Check for high blood pressure. d. Assess for heart failure.
3. Are the electrolytes abnormal? a. Check the potassium, magnesium and calcium levels
4. What medications is the patient on? a. Check for medications that can cause bradycardia b. Check for medications that can cause prolonged QT intervals and may precipitate tachycardia
Arrhythmias Originating in the
Sinus Node
Sinus Tachycardia
Sinus Bradycardia
Sinus Arrhythmia
Sinoatrial (SA) Block
Sinus Arrest
Sick Sinus Syndrome
Sinus Tachycardia
Sinoatrial node
Rhythm Rate
(per minute)
100 -160
P Wave PRI
(seconds)
0.12-0.20
QRS
(seconds)
0.06-0.10
Regular Upright
Uniform
Causes
Exercise, anxiety, fever, pain, hyperthyroidism, medications
Nursing Implications
Treat the cause
Sinus Bradycardia
Sinoatrial node
Rhythm Rate
(per minute)
P Wave PRI
(seconds)
QRS
(seconds)
Regular 40-60 Upright
Uniform
0.12-0.20
0.06-0.10
Causes
Sleep, athletic heart, increased vagal tone, beta-adrenergic blockade
Nursing Implications
Treat if there is hemodynamic compromise
Sinus Arrhythmia
Sinoatrial node
Rhythm
Irregular
Rate
(per minute)
Usually
60 -100
P Wave
Upright
Uniform
PR Interval
(seconds)
0.12-0.20
irregular rhythm associated with respiratory cycles;
HR á with inspiration &
HR â with expiration
QRS
(seconds)
0.06-0.10
Sinoatrial (SA) Block
Rhythm
Regular but interrupted
Rate
(per minute)
Usually
60-100
P Wave
Upright, uniform but entire cycle missing
PRI
(seconds)
0.12 – 0.20
QRS
(seconds)
<0.12
Causes
Coronary artery disease, medications, carotid sinus sensitivity and increased vagal tone
Nursing Implications
Treat if the pauses are long and there is hemodynamic compromise
Sinus Arrest
Rhythm Rate
(per minute)
P Wave
Escape rhythm
PRI
(seconds)
Regular but interrupted
Any rate No sinus
P’s
N/A
QRS
(seconds)
<0.12 (junctional)
>0.12 (ventricular)
Causes
Coronary artery disease, medications, carotid sinus sensitivity and increased vagal tone
Nursing Implications
Treat if the pauses are long and there is hemodynamic compromise
Sick Sinus Syndrome
A cluster of symptoms arising from a pathology in the sinus node. Results in dramatic changes in heart rate -bradycardia " tachycardia, interspersed with sinus arrests, pauses and blocks.
Escape beats common after long sinus pauses.
Rhythm Rate
(per minute)
P Wave PRI
(seconds)
QRS
(seconds)
Irregular Varies wildly
Too fast – too slow
May or may not be present, shape varies
If present, varies
Varies
See answers beginning on page 52
Causes
Ischemic disease, medication, inflammatory disease, surgical injury, idiopathic
Nursing Implications
Treat underlying cause (digoxin, beta blockers), pacemaker
Junctional Rhythms
Junctional Rhythm
Premature Junctional Contraction
Accelerated Junctional Rhythm
Junctional Tachycardia
Junctional Escape Rhythm
Junctional Rhythm
AV node 2 nd
1 st
Simultaneous
Atrium depolarized
1 st , then ventricles.
Upside down P wave
BEFORE QRS
Atria & ventricles depolarized simultaneously.
NO visible P wave, obscured by QRS
Ventricles depolarized 1 st , then atria.
Upside down P wave
AFTER QRS
Premature Junctional
Contractions (PJC)
Rhythm Rate
(per minute)
P Wave PRI
(seconds)
QRS
(seconds)
Regular but interrupted
Occurs at any rate
Inverted before or after QRS or not visible
<0.12 if P precedes QRS
<0.12
Causes
MI, Digoxin toxicity, hypoxia, stimulants
Nursing Implications
Remove the cause eg. Digoxin toxicity
AV node
Junctional Rhythm
Rhythm Rate
(per minute)
P Wave PRI
(seconds)
QRS
(seconds)
Regular 40-60 If visible, inverted
(before or after
QRS)
If able to measure
<0.12
<0.12
Causes
MI, Digoxin toxicity, Hypoxia, vagal stimulation
Nursing Implications
If symptomatic- atropine. Treat the cause eg. Digoxin toxicity
Accelerated Junctional
AV node
Rhythm Rate
(per minute)
60 -100
P Wave
Regular If visible, inverted (before or after QRS)
Causes
MI, stimulant drugs, caffeine, dig toxicity
Nursing Implications
Remove the cause
PRI
(seconds)
If able to measure
<0.12
Junctional Tachycardia
QRS
(seconds)
<0.12
Rhythm
Rate
(per minute)
P Wave PRI
(seconds)
Regular >100 If visible, inverted
(before or after
QRS)
Causes
Digoxin toxicity, heart disease, stimulants
Nursing Implications
If able to measure
<0.12
Identify and treat the cause eg. Digoxin toxicity
QRS
(seconds)
<0.12
Junctional Escape Rhythm
Rhythm
Regular
Irregular
Rate
(per minute)
40-60
P Wave
If present inverted before or after QRS
PRI
(seconds)
<0.12
Causes
MI, Digoxin toxicity
Nursing Implications
Identify and treat the cause eg. Digoxin toxicity
QRS
(seconds)
<0.12
See answers beginning on page 52
Ventricular Arrhythmias
Premature Ventricular Contraction
(PVC)
Accelerated (Idio)ventricular rhythm
Ventricular Tachycardia
Ventricular Fibrillation
Ventricular Escape Rhythm
Bundle Branch Blocks
Premature Ventricular
Contraction
Rhythm
Rate
(per minute)
P Wave PRI
(seconds)
QRS T wave
(seconds)
Regular but interrupted by PVC’s
Occurs at any rate
Not seen on
PVC’s
N/A >0.12 In opposite direction of
QRS
Causes
Heart disease, hypokalemia, hypoxia , hypomagnesemia, stimulants, caffeine, stress, anxiety,digoxin, significant anemia
Nursing Implications
Assess frequency of PVC’s and potential cause(s).
Bigeminy
Multifocal PVC’s
Accelerated Ventricular
Rhythm
Rhythm Rate
(per minute)
P Wave PR Interval
(seconds)
QRS
(seconds)
Usually regular
Causes
40-100 Usually not seen
Not measureable
Common after MI, administration of fibrinolytics
Nursing Implications
Usually well tolerated. This is the patient’s escape rhythm, so antiarrhythmics are not used
>0.12
Ventricular Fibrillation (VF)
Rhythm Rate
(per minute)
P Wave PR Interval
(seconds)
Not detectable
Causes
Can’t be counted
None Not detectable
Significant underlying cardiac disease, AMI, hypokalemia, hypoxia, hypomagnesemia, drugs
Nursing Implications
Code Blue- defibrillation
QRS
(seconds)
Not detectable
Ventricular Escape Rhythm
Rhythm Rate
(per minute)
20-40
P Wave
Usually regular
Usually not seen
Causes
Massive MI, hypoxia
Nursing Implications
Usually pulseless- CODE BLUE, CPR
PR Interval
(seconds)
Not measureable
QRS
(seconds)
>0.12
See answers beginning on page 52
Atrial Arrhythmias
Premature Atrial Contractions (PAC)
Atrial Tachycardia
Atrial Flutter
Atrial Fibrillation
Premature Atrial Contractions
Rhythm
Interrupted by PAC
Rate
(per minute)
Varies
P Wave
P of PAC different from underlying rhythm P’s
PRI
(seconds)
Differs from underlying rhythm
Causes
Electrolyte imbalance, stress, hypoxia, digoxin toxicity
Nursing Implications
Check electrolytes, O
2 saturation. Remove the cause.
QRS
(seconds)
<0.12
Atrial Fibrillation
Rhythm
Irregular
Rate
(per minute)
A: 350-650
V: slow to rapid
P Wave
Fibrillatory
(fine to coarse)
PRI
(seconds)
N/A
QRS
(seconds)
<0.12
CausesValvular HD,MI , thyrotoxicosis, lung disease
Nursing Implications
Assess BP as patient has lost atrial kick.
Lack of co-ordinated contraction in the atria predisposes patients to embolic events- anticoagulation required
Acute-cardiovert or control rate with beta blockers, calcium channel blockers
>48 hours- anticoagulation required x 3 weeks prior to cardioversion
See answers beginning on page 52
Heart Blocks
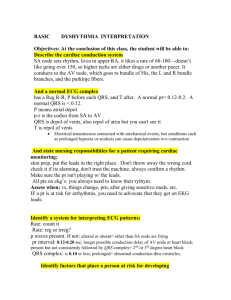
1. What is heart block?
Heart block is an arrhythmia usually caused by ischemia or an MI. It can also be caused by drugs such as beta blockers, calcium channel blockers, digoxin or any drug trying to slow down a fast rhythm and overshoots the mark!
2. What is being blocked in a heart block?
The signal from the SA node is trying to get through to the AV node (creating a p wave) and then to the ventricle (creating a QRS). In heart block the signal from the SA node through the AV node is either slowed down (causing a longer P-R interval) or blocked altogether , so there is a p wave but no QRS.is triggered by the p wave.
The key to heart blocks:
The signal is getting through:
1 all of the time (but taking longer than normal-.20 sec)
2 some of the time
3 none of the time
These are called first degree (#1), second degree (#2)and third degree (#3) heart blocks.
PR interval
3. What are the three types or degree of heart block?
Look at a normal sinus rhythm:
You can see the p waves and you can see where the QRS begins- the measurement from the beginning of the P to the beginning of the QRS is the PR interval. A normal P-
R interval should be no longer than .20 seconds or one big box on the EKG paper.
The PR interval represents the electrical depolarization from the SA node through the atria and the AV node. If the PR interval is normal then the signal is taking the normal amount of time to travel this far.
The signal should then travel to the ventricles to create a QRS.
3.1 First degree heart block:
Measure the PR interval. You will notice that it is longer than .20 seconds or one big block. It is taking longer than normal time to get from the SA node through the AV node to the ventricles. It does get to the ventricles all the time.
This is SR with a first degree heart block.
3.2 Second degree heart blocks:
By definition a second degree heart block has signals getting through some of the time.
So you will see p’s with QRS’s after them and you will see p’s without QRS’s after them.
The SA node will fire at a constant rate- some of the time the signal gets through the AV node to the ventricle and sometimes it doesn’t..
There are 2 kinds of second degree heart block:
The first kind can be called one of two names: Type 1 second degree or Wenckebach.
3.2.1 Second degree type 1-Wenckebach
You can see the p waves without a QRS . The signal is getting through the AV node some of the time.
Look at the PR intervals before the dropped beat- the PR starts out normal, then gets longer with the next beat, longer with the subsequent beat and then doesn’t get through.
So the PRs leading up to the dropped beat get longer and longer then drop.
The heart rate in this patient is still 70 bpm, so the patient probably has a good blood pressure. Usually this rhythm is benign and is transient due to a MI. However it still bears watching.
3.2.2 Second degree type 2
Second degree type 1- PRs- longer,longer, longer and drop Predictable
Second degree type 2-PRs- all the same and then drop a QRS without warning Unpredictable
You can see the p’s without the QRS. The other Ps are followed by a QRS and all the
PRs are the same . The signal is getting through to the AV node some of the time. – therefore it is a second degree heart block.
The PRs of the other beats are all the same.
This heart block is much more serious and can progress to third degree heart block
(complete heart block). This patient requires a pacemaker.
3.3 Third degree heart block (complete)
Third Degree Heart Block
In third degree heart block the SA node is firing a signal at a regular rate. The top arrows show where the p’s are.
However the signal is not getting through the AV node to create a QRS.
When this happens either the AV node or the ventricle will generate a rate by themselves. If the AV node generates it the QRS will be narrow. If the ventricle generates it the QRS will be wide. The QRS is marked by the arrows at the bottom.
If you measure the PR intervals, none of them are the same. There are p’s in the middle of QRS’s. This tells you that there is no connection between the p and the QRS.
The SA node and the ventricle are depolarizing independently of each other. None of the p waves are conducted through the AV node to the ventricle.
This heart block is serious as the ventricular rate can go as low as 20 or stop altogether.
This patient requires a pacemaker.
AV Blocks
1 p for every QRS
Constant Prolonged P-R Interval
More p’s than QRS
P-R constant?
1 0 AV block
NO YES
2 0 type 2 AV block
Includes 2:1 AV conduction
Regular R-R?
Diagram
NO
YES
: AV blocks on the right side of the diagram are the most serious and
2 0 AV block type 1 (Wenckebach) require a permanent pacemaker. AV blocks on the left side are less serious, transient, or the causes can be reversed.
NO YES
Ventricular escape Junctional escape
Atrioventricular (AV)
Conduction Disturbances
First Degree AV Block
Second Degree AV Block
Type I (Wenckebach)
Type II
Third Degree (Complete) AV Block
First Degree AV Block
Rhythm
Depends on underlying rhythm
Rate
(per minute)
Can occur at any rate
P Wave upright
Uniform
Precede QRS
PR Interval
(seconds)
Prolonged
> 0.20
QRS
(seconds)
< 0.12
Causes
AV node ischemia,dig toxicity,drugs (beta blockers, calcium channel blockers), ablation
Nursing Implications
Remove the cause. Treat the cause
2
nd
Degree Heart Block
Type I - Wenckebach
Rhythm Rate
(per minute)
P Wave PRI
(seconds)
QRS
(seconds)
Usually irregular
Atrial usually
60-100
Ventricular
< atrial
Sinus P’s Gradually # ’s until QRS dropped
<0.12
if block at
AV
>0.12
if block at bundle branches
CausesDrugs , MI, chronic degenerative conduction disease.
Nursing Implications
Usually due to MI, is transient and only requires observation
If symptomatic- atropine, pacemaker
2
nd
Degree Heart Block
Type II
Rhythm
Regular
Or
Irregular
Rate
(per minute)
Atrial usually
60-100
Ventricular
< atrial
P Wave
Sinus P’s
2 or > before each QRS
PRI
(seconds)
Constant for conducted beats
QRS
(seconds)
<0.12
if block at AV
>0.12
if block at bundle branches
CausesDrugs , MI, chronic degenerative conduction disease, hypoxia
Nursing Implications
Definitive treatment is a pacemaker as this can progress to complete AV block or asystole.. Atropine can be tried for symptoms, but may paradoxically slow the heart rate.
Third Degree AV Block
Rhythm
Regular
Rate
(per minute)
Atrial 60 -100
Ventricular
Block at AV 40-60
Block at bundle branches 20-40
P Wave
Sinus P’s with no relation to
QRS
PRI
(seconds) varies
QRS
(seconds)
Block at AV
<0.12
Block at bundle branches
> 0.12
CausesDrugs , MI, chronic degenerative conduction disease, hypoxia
Nursing Implications
Definitive treatment is a pacemaker . Atropine can be tried for symptoms, but may paradoxically slow the heart rate.
See answers beginning on page 52
Rate: Atrial __40____ Ventricular __40______ Regular?___
Yes _______________
P waves _Yes-all the same_____ Followed by QRS?__
Yes__ PRI __0.16 QRS___ 0.08___
ST segment __baseline__________________ T wave ___upright____________
QT Interval ____less than ½ the R-R interval
I nterpretation
PRACTICE STRIP ANSWERS
Practice Strips page 32
Rate: Atrial __70____ Ventricular __70_______ Regular ?___No- slows down and speeds up
P waves ____Yes-all the same Followed by QRS ?__Yes_____ PRI __0.14 QRS _0.08_____
ST segment ___depressed_______________ T wave upright______________
QT Interval ______1/2 the R-R interval
Interpretation _______Sinus arrhythmia______________________________________
Rate : Atrial __none__ Ventricular ___60______ Regular ?___yes________________
P waves ___none___________ Followed by QRS ?_no____ PRI _none_ QRS ___0.06__
ST segment ______lightly depressed____ T wave __upright_____________
QT Interval _____can’t measure____
Practice Strips Page 36
Iterpretation _________junctional rhythm___________________________________
Practice Strips page 41
Rate: Atrial __300___ Ventricular __80_______ Regular ?____No________________
P waves __f waves_________ Followed by QRS ?__sometimes PRI _not measured_____ QRS __0.10________
ST segment ____hard to tell________________________ T wave __can’t see____________________
QT Interval Practice Strips page 44
3 second arrows show f waves
Interpretation __________atrial flutter with variable conduction from A to V hidden in the QRS
Rate: Atrial ___no p_____ Ventricular __90_________ Regular ?__irregular____________________
P waves _no________________ Followed by QRS ?_no______ PRI __none____ QRS __0.08________
ST segment _____hard to tell- could be depressed_____________ T wave _upright_____________________
QT Interval ________0.28 normal________________
Interpretation ________atrial fibrillation with controlled ventricular response (less than 100/ minute)
QT interval
Rate: Atrial ____80____ Ventricular __60_________ Regular ?____No__________________
P waves _yes-all the same______ Followed by QRS ?_not all______ PRI _0.16-0.32 prolonging_____ QRS __0.06____
ST segment ____baseline________________ T wave _____upright__________
Interpretation _______second degree type 1 AV block___(Wenckeback)_____________________
REFERENCES
Arrows indicate p waves hidden in the complex
Rate: Atrial ___80_____ Ventricular __30_________ Regular ?____yes__________________
P waves ___upright_______________ Followed by QRS ?_no______ PRI __all different____ QRS __0.16_(wide)_______
ST segment ______depressed______________________ T wave __inverted____________________
QT Interval ______0.28 normal_________________
Interpretation __________3 rd degree AV block ___________________________________________________
References
1. Daly, S., Weinstein E., Ambrose, M., Charnow, J., (eds) et al. (1993)
Deciphering Difficult ECG’s. Pennsylvania: Springhouse Corporation.
2. Dubin, D. (2000) Rapid Interpretation of EKG’s. 6th edition. Florida: COVER
Publishing Company.
3. Ellis, Karen (2002) EKG Plain and Simple. New Jersey: Prentice Hall.
4. Hudak, C., Gallo B., Gonce Morton, P.,(1998) Critical Care Nursing: A Holistic
Approach. 7th edition. New York: Lippincott.
4. Stein, E. (1997) Clinical Electrocardiography: A Self Study Course.
Philadelphia: Lea & Febiger.
5. Vinsant, M., Spence, M. (1989) Commonsense Approach to Coronary Care: A
Program: 5th edition. Toronto: The C.V Mosby Company.
6. Woods, S., Sivarajan Froeclicher,E., Underhill Motzer, S. (2000) Cardiac
Nursing. 4th edition. New York: Lippincott.
7. Online- the Medstud.com
RHYTHM INTERPRETATION
TEST
Please check with your CE to see which test is appropriate for you to complete
Please evaluate the following strips in a systematic way. Describe the dysrhythmia by the predominant underlying rhythm and then any other rhythm or extra beats that are on the strip. e.g.- SR with PVC’s or
SR with first degree HB
Filling out the test completely should lead you to an accurate interpretation
Thank you
1. What is the ventricular rate_________?
• Is it regular?________
• Are there any premature QRS’s?______
•
Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
• What is the rate ? ____________
• Are the each followed by a QRS? ________
3. What is the P-R interval ? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
• Is it regular?________
• Are there any premature QRS’s?______
• Ask yourself -Are the premature QRSs wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Marks
1
1
2
2
2
1
1
Mark
1. What is the ventricular rate_________?
•
Is it regular?________
•
Are there any premature QRS’s?______
• Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
/10
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
• Is it regular?________
• Are there any premature QRS’s?______
• Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
• What is the rate? ____________
• Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
•
Is it regular?________
•
Are there any premature QRS’s?______
•
Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
• What is the rate? ____________
• Are the each followed by a QRS? ________
3. What is the P-R interval? __________
• Is it constant? __________
• If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
•
Is it regular?________
•
Are there any premature QRS’s?______
•
Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
• If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
• Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
•
Is it regular?________
•
Are there any premature QRS’s?______
•
Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
•
Is it regular?________
• Are there any premature QRS’s?______
• Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
1
Marks
1
1
2
2
1
2
/10
1. What is the ventricular rate_________?
•
Is it regular?________
•
Are there any premature QRS’s?______
•
Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
•
Is it regular?________
• Are there any premature QRS’s?______
• Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
1. What is the ventricular rate_________?
• Is it regular?________
• Are there any premature QRS’s?______
• Ask yourself- Are the premature QRS’s wide or narrow?_______
2. P waves
•
What is the rate? ____________
•
Are the each followed by a QRS? ________
3. What is the P-R interval? __________
•
Is it constant? __________
•
If not constant what is happening to the P-R?
___________________________________
4. What is the QRS duration?__________
•
Is this a normal QRS duration?________
Ask yourself:
Could there be a hidden p wave in the ST segment or T wave? _____
5. Identify the conduction pathway for this rhythm on the following diagram
6. State the rhythm diagnosis _____________________________
Mark
Marks
1
1
2
2
1
1
2
/10
RHYTHM INTERPRETATION
Test # 2
Please check with your CE to see which test is appropriate for you
Please evaluate the following strips in a systematic way. Describe the dysrhythmia by the predominant underlying rhythm and then any other rhythm or extra beats that are on the strip. e.g.-
Normal Sinus rhythm with Premature Ventricular Contractions (NSR with PVCs) or
Normal Sinus Rhythm (NSR) with first degree Heart Block (HB)
For test purposes each rhythm strip will be assumed to be a 6 second strip.
Identify the normal PR interval as 0.12-0.20 and abnormal as > 0.20 as
in the learning guide
Identify the normal QRS interval as 0.06-0.10 and abnormal as > 0.10
as in the learning guide
Filling out the test completely should lead you to an accurate interpretation.
Each test strip will be marked out of 5 for a total score out of 25.
Thank you
Strip #1
2. a) What is the ventricular rate? _________ a) Is it regular? _________
2. P waves
a) What is the rate? ____________ b) Is each P wave followed by a QRS? ________
3. a) What is the P-R interval? __________
b) Is it constant? __________
7. a) What is the QRS duration? __________ b) Is this a normal QRS duration? ________
8. State the rhythm diagnosis. _____________________________
Strip #2
1. a) What is the ventricular rate? _________
b) Is it regular? ________
3. P waves a) What is the rate? ____________
3. a) What is the P-R interval? __________
7. a) What is the QRS duration? __________
8. State the rhythm diagnosis. _____________________________
Strip #3
1. a) What is the ventricular rate? _________ b) Is it regular? ________
2. P waves
a) What is the rate? ____________
3. a) What is the P-R interval? __________
7. a) What is the QRS duration? __________ b) Is this a normal QRS duration? _________
8. State the rhythm diagnosis. _____________________________
Strip #4
1. a) What is the ventricular rate? _________
b) Is it regular? ________
2. P waves
a) What is the rate? ____________
b) Are they each followed by a QRS? ________
3. a) What is the P-R interval? __________
7. a) What is the QRS duration? __________ b) Is this a normal QRS duration? ________
8. State the rhythm diagnosis. _____________________________
Strip #5
1. a) What is the ventricular rate? _________
b) Is it regular? ________
c) Are there any premature QRS’s? ______
Qhc- 01.701.8402000
2. P waves
a) What is the rate? ____________
3. a) What is the P-R interval? __________
b) Is it constant? __________
7. a) What is the QRS duration? __________
8. State the rhythm diagnosis. _____________________________