Ultrasound Findings of Ectopic Pregnancy
advertisement
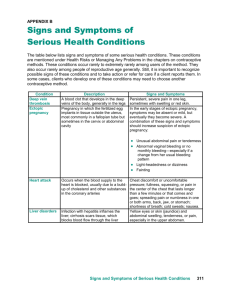
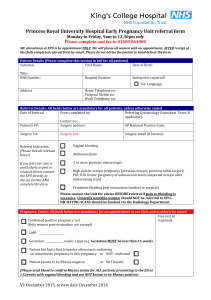
Ultrasound Findings of Ectopic Pregnancy Claudia Diaz, HMS III Radiology - BIDMC May 2008 Objectives Index case DDX of abdominal pain Clinical presentation Diagnostic Tests Transvaginal Ultrasonography Female Reproductive Anatomy Imaging of index case Transvaginal sonographic findings Additional patient cases Ectopic pregnancy locations Ectopic pregnancy facts & management Take-home points Image: http://www.aafp.org/afp/20051101/1707.pdf Patient Index Case HPI: 32-year-old G1P1 with LMP 8 wks ago, presenting with 3 weeks of ongoing LLQ pain. Reports mild vaginal bleeding for the last 10 days. Negative pregnancy test and normal ultrasound 3 weeks ago. EXAM: VITALS: T 98.4 HR 100 RR 20 BP 123/67 ABDOMEN: Tender to palpation in LLQ with radiation to RLQ. PELVIC: No active bleeding. Mild cervical motion tenderness, left adnexal tenderness. LABS: HCG: 3610 Differential diagnosis DDX for abdominal pain in women of reproductive age includes: Pregnancy-related: Ectopic pregnancy, spontaneous abortion. Gynecologic: Endometritis, pelvic inflammatory disease, tubo- ovarian abscess, endometriosis, ovarian neoplasm, ovarian torsion/rupture/hemorrhage, uterine fibroids. Non-gynecologic: Appendicitis, bowel obstruction, diverticulitis, IBD, UTI, pyelonephritis, nephrolithiasis. Clinical Correlates Clinical Triad Abdominal Pain Vaginal Bleeding Amenorrhea These clinical findings are non-specific and also occur in patients who spontaneously abort. Physical exam findings Enlarged uterus. Vaginal bleeding. Pelvic pain with manipulation of cervix. Palpable adnexal mass. Æ Red flags for ruptured ectopic pregnancy: Significant abdominal tenderness, hypotension, guarding and rebound tenderness. Diagnostic Tests Urine pregnancy test. B-hCG measurement. Less commonly used: diagnostic curettage & serum progesterone levels. Radiologic test of choice: Transvaginal ultrasound. Human Chorionic Gonadotropin (B-hCG) Levels Normal intrauterine pregnancy: B-hCG levels should rise by at least 66% over 48hrs. Levels of hCG that plateau in first 8wks of pregnancy indicate abnormal pregnancy (SAB or ectopic). Transvaginal ultrasonography should detect an intrauterine pregnancy when B-hCG level is >1500mIU/mL (~1500-2000mIU/mL). Risk of ectopic pregnancy high if hCG above discriminatory factor without an intrauterine gestational sac. Transvaginal ultrasonography: the modality of choice How does it work? High-frequency sound waves directed into the body and manner in which sound is reflected back to transducer is recorded. Æ Advantages: no ionizing radiation, inexpensive, Æ Æ minimal invasive. Disadvantages: operator dependent, moderate resolution. Transabdominal US is no longer considered to be sufficient for proper diagnosis. Transvaginal US is the imaging of choice for evaluation of ectopic pregnancy: Intrauterine pregnancies are reliably diagnosed earlier. Sensitivity: 67 to 100. Specificity: 100 (virtual certainty). Image: http://www.stjohnsmercy.org/ healthinfo/test/gyn/TP124.asp# Diagnosing suspected ectopic following TVS Image: http://www.aafp.org/afp/20051101/1707.html Female Reproductive Anatomy http://infertility.health-info.org/reproductive-anatomy-physiology/reproductive-anatomy-physiology-home.html Index Case U RO U - Uterus measuring approximately 7.2 x 4.8 x 4.9 cm. RO - Right ovary. PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Index Case RIGHT ADNEXA: 1.4-cm ring-shaped structure containing a yolk sac and living embryo. PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Index Case Embryonic crown-rump length (CRL) consistent with a 6w3d pregnancy. Embryonic cardiac activity measuring 120 beats per minute is documented. CRL Patient underwent operative laparoscopy with right salpingectomy. PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. “Double Sac” Sign Earliest sonographic sign of IUP is “double sac” sign: Æ True gestational sac – double echogenic rings surrounding hypoechoic fluid (sac). - inner ring: decidua capsularis. - outer ring: decidua parietalis. Æ Visible at 4-5wks of gestation. Doubilet, Peter M. & Carol B. Benson. Emergency Obstetrical Ultrasonography. Seminars in Roentgenelogy, Vol XXXIII, No 4(Oct), 1998: pp 339-343. Likelihood of Ectopic pregnancy based on transvaginal sonographic findings Ultrasound Finding Likelihood of ectopic pregnancy (+B-hCG, vaginal pain or bleeding, no IUP) Extrauterine embryo with cardiac activity 100% Adnexal fluid w/ yolk sac or apparent embryo w/out heartbeat 100% Tubal ring 95% Complex or solid adnexal mass w/out tubal ring, yolk sac, or embryo (excluding masses w/in ovary) 92% No significant adnexal abnormality 5% Æ OTHER COMMON RADIOLOGIC FINDINGS: Æ Æ Æ Free fluid in pelvis and/or abdomen. “Ring of fire” – mass in adnexa surrounded by hypervascular flow on doppler. Pseudogestational sac in uterus. Doubilet, Peter M. & Carol B. Benson. Emergency Obstetrical Ultrasonography. Ultrasonography. Seminars in Roentgenelogy, Vol XXXIII, No 4(Oct), 1998: pp 339339-343. Patient Case #2 HPI: 31-year-old G1P0 at 7 weeks GA by LMP with ultrasound findings suspicious for ectopic pregnancy. Treated with methotrexate, admitted for severe RLQ pain, and subsequent ruptured ectopic pregnancy. Patient underwent operative laparoscopy and right salpingectomy. LABS: HCG: 3523 (day 1) Æ 1964 (day 3) Æ 1400 (day 4) Patient Case #2 Transvaginal Ultrasound I: day 1 No evidence of intrauterine gestational sac. Adjacent to right ovary, complex echogenic area thought to be empty sac (E). E E Transvaginal Ultrasound II: day 3 Slight interval increase in size of right ectopic pregnancy (E). PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Patient Case #2 Transvaginal Ultrasound III: day 4 --> RUPTURED ECTOPIC Adjacent to right ovary, heterogeneously echoic structure (ectopic (ectopic pregnancy - RE) increased in size. Large amount of new free fluid. RE PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Patient Case #2 FF FF – free fluid in pelvis. PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Patient Case #3 HPI: 32-year-old G8P2 at unknown GA with lower abdominal pain and vaginal bleeding, and amenorrhea x1 year. Positive pregnancy test previously but no IUP on recent ultrasound. EXAM: VITALS: T 97.6 HR 76 RR 18 BP 104/68 ABDOMEN: Diffusely tender to palpation suprapubically, no R/G. PELVIC: Blood at cervical os. Mild cervical motion tenderness, left adnexal tenderness. LABS: HCG: 2413 Æ 1794 (drop in last 3 days). Patient Case #3 Transabdominal & Transvaginal Ultrasound: Large adnexal mass and moderate amount of complex free fluid within within the pelvis. No evidence of IUP, possible pseudosac. U B U FF B – bladder U - uterus CF – cul-de-sac free fluid PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Patient Case #3 Patient underwent left salpingectomy via laparotomy. A B A: Complex, heterogeneous left adnexal mass with internal echoes on on left adnexa. B: Small oval structure with anechoic center within the uterine fundus fundus without characteristic intrauterine gestational sac (no true dedidual reaction) Æ Pseudosac. PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Patient Case #4 HPI: 22-year-old G1P0 at 8w1d by LMP presenting with 4-weeks of ongoing EXAM: light vaginal bleeding and severe lower abdominal pain. guarding, + rebound. PELVIC: Deferred. LABS: VITALS: T 98.4 HR 101 RR 18 BP 142/79 ABDOMEN: Rigid, tender to palpation in lower quadrants b/l, +involuntary HCG: 488 Transabdominal Ultrasound: No IUP visible. Large heterogeneous mass without definite color flow posterior to uterus (11.6 x 7.4 x 11 cm). Moderate free fluid in abdomen/pelvis, extending into Morrison’s pouch and spleen, low level echoes concerning for blood. Patient Case #4 U U: uterus. M: heterogenous mass. RK: Kidney. L: Liver. Arrow: Morrison’s pouch, hepato-renal space. L M RK Patient underwent laparotomy and right salpingectomy. PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Ectopic pregnancy locations Ectopic pregnancy results if the blastocyst implants anywhere outside of the uterine cavity. The vast majority of ectopic pregnancies occur in: Ampulla Ectopic Pregnancy --- 75% - 90% Isthmic Ectopic Pregnancy --- 5% - 15% Heterotopic pregnancy (one embryo in the uterus and one ectopic embryo): 1/7000 (incidence in heterotopic pregnancies has increased due to assisted reproductive technologies – 1%). http://www.ectopicpregnancyfoundation.org/ectopicpregnancyplacementdiagram.htm Predisposing factors **Any factor that interferes with the normal fallopian tube function** Previous tubal surgery. Previous ectopic pregnancy. In-utero diethylstilbestrol exposure. Previous gynecologic infections (PID). Treatment of infertility. Current cigarette smoking. Previous intrauterine device use. Ectopic pregnancy facts Ectopic pregnancies make up 1.9% of all reported pregnancies (0.5% of all pregnancies in 1970 to 2% in 1992). Incidence increasing due to increase in pelvic inflammatory disease and ART. 10-15% of all maternal deaths are due to ectopic pregnancies. Infertility occurs in 10-15% of women who have had an ectopic pregnancy. Management of Ectopic Pregnancy MEDICAL (MTX) EXPECTANT MANAGEMENT 1. Small tubal diameter (<3.5cm). 2. No fetal cardiac activity. 1. Low & declining hCG levels. 3. hCG concentration <5000mIU/mL. Æ Serial hCG measurements! SURGICAL 1. Ruptured ectopic/ hemodynamically unstable. 2. Contraindications to medical therapy. 3. Lack of timely access to medical institution. 4. Failed medical therapy. Take-home points Ectopic pregnancy should always be considered in women of reproductive age presenting with abdominal pain. The classic triad of ectopic pregnancy includes abdominal pain, vaginal bleeding, and amenorrhea. Transvaginal ultrasound is the modality of choice when diagnosing an ectopic pregnancy. With hCG level>1500mIU/mL and no IUP identified on transvaginal ultrasound, this is high-risk for ectopic pregnancy. Transvaginal ultrasound is diagnostic if a true gestational sac, yolk sac, embryo, or cardiac activity is found inside or outside of the uterus. Ectopic pregnancy is the leading cause of pregnancy related death in 1st trimester of pregnancy. References Bhatt, Shweta; Hamad Ghazale, Vikram S. Dogra. Sonographic evaluation of ectopic pregnancy. Radiologic clinics of North America. 45 (2007) 549-560. Derchi, Lorenzo E. et al. Ultrasound in gynecology. Eur Radiol. (2001) 11:2137-2155. Doubilet, Peter M. & Carol B. Benson. Emergency Obstetrical Ultrasonography. Seminars in Roentgenelogy, Vol XXXIII, No 4(Oct), 1998: pp 339-343. Lozeau, M.D., M.S., Anne-Marie & Beth Potter, M.D. Diagnosis and Management of Ectopic pregnancy. American Family Physician. Volume 72, No 9; Nov. 2005. Nelson AL, DeUgarte CM, Gambone JC. Ectopic pregnancy. In: Hacker NF, Moore JG, Gambone JC. Essentials of obstetrics and gynecology, 4th ed. Philadelphia: Saunders, 2004: 325-333. Novelline, Robert A. Ultrasound imaging & Ectopic pregnancy. Squire’s Fundamentals of Radiology. Sixth edition. Pgs. 34-35 & 430-431. Toy, MD, Eugene C., Benton Baker, MD, MSC, Patti Jayne Ross, MD, Larry C. Gilstrap, MD. Case Files: Obstetrics & Gynecology. Pgs. 63-69, 211-218, 329-333. Yudin, MD, Mark H. MSc, FRCSC, & Harold C. Wiesenfeld, MDCM. Current Diagnosis & Treatment of Sexually Transmitted Diseases. Chapter 5: Lower Abdominal Pain in Women. Images References 1. http://www.aafp.org/afp/20051101/1707.pdf 2. http://www.stjohnsmercy.org/ healthinfo/test/gyn/TP124.asp# 3. http://www.aafp.org/afp/20051101/1707.html 4. http://infertility.health-info.org/reproductive-anatomy-physiology/reproductive-anatomy-physiology-home.html 5. http://radiology.rsnajnls.org/cgi/content/full/210/2/579/F2 6. http://www.ectopicpregnancyfoundation.org/ectopicpregnancyplacementdiagram.htm 7. Cases: PACS, BIDMC. Courtesy of BIDMC-ultrasound recorded case files. Acknowledgements Dr. James Kang Dr. Jay Pahade Dr. Rola Shaheen