Chem*3560 Structure and Function in Biochemistry Winter 2002
advertisement

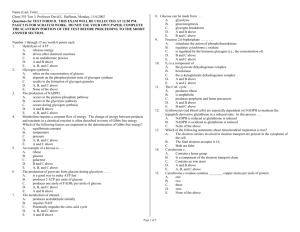
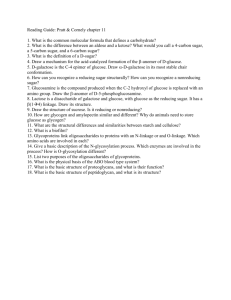
Chem*3560 Structure and Function in Biochemistry Winter 2002 Lecturers: Dr. A. Mellors, Rm 331 MacNaughton Bldg. West Wing, Phone (519) 824-4120 Ext. 3792; Fax (519) 766-1499 E-mail amellors@uoguelph.ca Office hours: Mon., Wed., Fri. 9:30 - 10:30 a.m. Other times by appointment, please. Lectures: Section 01: Mon., Wed., Fri, 12:30 PM- 1:20 PM. Room: Chemistry and Microbiology 200. Section 02: Mon., Wed., Fri, 3:30PM - 4.20 PM. Room: MacNaughton 105. Section: Sections are assigned by the registrar and students are requested to attend only the section to which they are assigned. Course Synopsis: This is a systems-oriented course where biochemical structure, function and some metabolism are presented in an integrated fashion. Textbooks: Required: "Biochemistry" by Lubert Stryer, Fourth Edition, published by W.H. Freeman, Sufficient copies are available at the Campus Bookstore. Warning:a completely revised Fifth Edition by Stryer and other authors is about to be published (Dec. 2001). This Fifth edition will NOT be used for the Winter 2002 semester and will probably not be used in future years. Several copies of the 4th and previous editions are on reserve (2 hour loan) at the Library Reserve Desk. The text Lehninger: Principles of Biochemistry (Lehninger, Cox and Nelson) is not very suitable for this course as it lacks coverage of certain topics. Sample midterms and a final exam are also available at the Reserve Desk. Computer Simulations For assistance with metabolic pathways, used in the second half of the course, students are encouraged to try the computer simulations available in the Chemistry-Biochemistry Computer Room, Chem-Micro Building Room B44. The relevant exercises are : Gluconeogenesis and the pentose-phosphate pathway: Glycogen synthesis and degradation: Fatty acid oxidation and synthesis. Web pages: Pages that worked at the start of the semester: http://www.chembio.uoguelph.ca/educmat/chm356/chm356.htm For hemoglobin structure and function, useful Web sites are: http://globin.cse.psu.edu/globin/html/huisman/variants/contents.html http://www.cryst.bbk.ac.uk/PPS2/course/section12/index.html http://www.umass.edu/microbio/chime/hemoglob/2frmcont.htm http://ntri.tamuk.edu/homepage-ntri/lectures/protein/protein.html http://grserv.med.jhmi.edu/~raj/javanim.html You can test your general knowledge of protein structure and function by doing the multiple choice problems shown at: http://bob.usuf2.usuhs.mil/biochem/exams/bytopic/proteins-f/node1.html Sickle cell disease: http://www-rics.bwh.harvard.edu/sickle/menu_sickle.html Southern blotting and restriction fragment length polymorphism: http://www.biology.washington.edu/fingerprint/problems.html http://vector.cshl.org/shockwave/southern.html Thalassemia: http://sickle.bwh.harvard.edu/thalover.html Allosteric behaviour of aspartate transcarbamoylase: http://bioinfo.mbb.yale.edu/MolMovDB/cgi-bin/morph.cgi?ID=atcase Prions and mad cow disease: http://www.airtime.co.uk/bse/welcome.htm http://www.diseaseworld.com/ http://www.sciam.com/0195issue/prion.html Blood clotting and fibrinolysis : http://www.chembio.uoguelph.ca/educmat/chm356/clot/index.htm http://brie.medlabscience.med.ualberta.ca/mlsci/235/clotcascade.html Hemophilias : http://vector.cshl.org/ygyh/mason/ygyh.html?section=whatisit&syndrome=hemo Glycolysis and glycogenolysis controls: http://www.jonmaber.demon.co.uk/ http://web.indstate.edu:80/thcme/mwking/glycogen.html#intro The sodium pump: http://www.cbc.med.umn.edu/~mwd/cell_www/chapter2/Na-Kpump.html http://www.bio.davidson.edu/biology/courses/Molbio/26aa/alphabeta.html An animated cartoon of the Na+/K+-ATP-ase is shown at: http://199.17.138.73/berg/ANIMTNS/Na-Kpump.htm Reference Material: Other textbooks are available at the Library Reserve Desk. Grade Assessment: Midterm Examination 40% Final Examination 60% Both exams are required. If the mid-term is not taken then the final exam will be 100% of the grade. Examination Schedule: Midterm Examination: The midterm will be written on Tuesday February 26th at 5:30 p.m. to 7:00 p.m.) in class-rooms to be announced. Persons with a scheduled academic conflict should inform the instructor by e-mail (amellors@uoguelph.ca), stating the conflicting course, by February 15th , and may be granted an alternative exam which will be held prior to the regular mid-term on Monday February 25th at 5:30 p.m. to 7:00 p.m. Final Examination: As scheduled by the registrar on the first day of the final exam period, Tuesday, April 9th , 11.30 a.m. -1.30 p.m. (No exceptions). The final exam is cumulative. Students who score a significantly higher grade on the Final Exam, compared with the Midterm, may receive a higher weighting of the Final Exam, at the discretion of the instructor. A significantly higher grade is one that is 25 percentage points higher. Re-grading: Midterm papers may be returned to the instructor for correction of grading errors, only within one week of the return of the paper to the student, and only if the paper was written in ink. No additions in ink must be made after return of the paper, and the instructor will photocopy some or all of the papers at the time of grading. The instructor may refuse to re-grade a paper at his discretion. Exam aids: No materials may be brought to the exam except for three pencils, three pens and an eraser. No calculator, pencil cases, purses, bags, Kleenex boxes or other containers may be present. All materials are subject to inspection. Drop and Add: Notification is not needed for dropping the course before the DROP deadline (40th class day). Program approval is only needed for drops and adds if your category is ASpecial@ or AProvisional@. Course Evaluation: As part of the faculty evaluation process in the Department of Chemistry and Biochemistry, students are reminded that written comments on the teaching performance of the lecturer may be sent to the Chair, Department of Chemistry and Biochemistry, at any time. Such letters must be signed; a copy, will be made available to the instructor after submission of final grades. Chem*3560 Schedule of topics. Note: This schedule is tentative and may be modified during the term. Chapter references are to Stryer. Stryer Lehninger et al. th 4 Edition References in italics are to similar coverage where available in Lehninger, Cox and Nelson. PART A: PROTEIN STRUCTURE AND ENZYME REGULATION: Chapter 7 Oxygen-transporting proteins Hemoglobin and myoglobin: structures 147-157 Cooperativity: inter-subunit communication in hemoglobin. 157-168 Hemoglobin S and the consequences of mutation. 168-177 Chapter 8 Introduction to enzymes Review enzyme kinetics. Allosteric enzymes. Sigmoidal kinetics. Chapter 10 Control of enzymatic activity Control by allosteric effectors: ATCase: a regulatory enzyme 237-244 R and T states: concerted model and the sequential model. 166-168 Control by proteolytic cleavage: Zymogen activation. Serine proteases of digestion: chymotrypsin. 247-249 Blood clotting: a zymogen amplification cascade 252-255 Fibrinogen and formation of the fibrin clot. Thrombin and prothrombin. Vitamin K. Hemophilia. 255-260 203-206 210-211 206-219 219-221 278-281 No coverage 216 286-287 No coverage No coverage No coverage PART B: REGULATION AND INTEGRATION OF METABOLISM: Chapter 18: Pentose phosphate pathway and gluconeogenesis Pentose phosphate pathway.Sources of NADPH for biosynthesis 559-565 Review gluconeogenesis. Regulation of carbohydrate metabolism. Control by covalent modification (phosphorylation): 244-247 Phosphofructokinase and fructose-1,6-bisphosphatase. 493-495 Role of fructose-2,6-bisphosphate. 569-576 Substrate cycles. Net direction of glycolysis/gluconeogenesis. Chapter 19: Glycogen metabolism Glycogen synthase and phosphorylase; 581-598 protein phosphorylation cascade. Chapter 20: Fatty acid metabolism Reaction sequence. 614-622 Fatty acid synthase. Contrast with ß-oxidation. Chapter references are to Stryer. Stryer 4th Edition 557-559 281-283 732-733 No coverage 730-731 282-286 770-777 Lehninger et al. References in italics are to similar coverage where available in Lehninger, Cox and Nelson. Chapter 26: Integration of metabolism Integration of metabolic pathways. Hormones: Insulin, glucagon, epinephrine. 763-773 773-782 485-489 869-884 268-278 267, 280 389-398 311-313 309-317 415-421 291-306 421-430 PART C: MEMBRANES Chapter 12: Introduction to biological membranes The fluid mosaic model of membrane structure. Glycolipids and glycoproteins. Chapter 37: Membrane Transport Na+-K+ ATPase Chapter 39: Excitable membranes and sensory systems Channels and the action potential The instructor reserves the right to change any of the above, in accordance with University of Guelph regulations. Chem*3560 LECTURE SUMMARY: Lecture 1: Structure and function of the oxygen binding proteins, myoglobin and hemoglobin. Heme; protoporphyrin IX; Myoglobin; Hemoglobin, the O2 carrier in blood Lecture 2: The Globins. Myoglobin; Hemoglobin; The 3-dimensional structures; What determines folding?; Comparing amino acid sequences of globins; Helical segments; Connecting loops; Hemoglobin-A, Adult; Hemoglobin F; Fetal; Embryonic hemoglobin Lecture 3 and review , assignment 1: O2 Binding by Myoglobin and Hemoglobin.Absorbance; oxyhemoglobin; O2 affinity of myoglobin versus hemoglobins Lecture 4: Cooperative oxygen binding by hemoglobin. Hyperbolic binding; sigmoidal binding; Hill Equation; The cooperative binding model; The sequential model of; The concerted or symmetry model Lecture 5: Monod, Allosteric cooperative binding of O2 and the structure of hemoglobin. Wyman and Changeux model (MWC); X-ray crystallography studies of hemoglobin Lecture 6 and review assignment 2: Oxygen binding proteins. Lecture 7: Other factors controlling O2 binding by hemoglobin. Effect of pH and CO2; 2,3-bisphosphoglycerate Lecture 8: Hemoglobin genetics and Molecular diseases. Sickle cell anemia; molecular disease; malarial parasite; sequence of the mutant DNA; Thalassemias; The globin genes in humans Lecture 9 and review assignment 3: Allosteric control of enzymes. Aspartate transcarbamoylase. Lecture 10: Structural studies of ATCase. Lecture 11: The allosteric mechanism of ATCase: more experimental evidence. Lecture 12 and review assignment 4: Allosteric Cooperativity. Regulation by covalent modification of enzymes by phosphorylation and dephosphorylation Lecture 13: Regulation by proteolysis; Proteolytic activation; Digestive enzymes; Zymogens; Chymotrypsin, Proteases; Blood clotting; Prothrombin; Thrombin. Lecture 14: Blood clotting.Fibrin; fibrinogen; Intrinsic pathway; Extrinsic pathway; activation cascade; Factor VIIIa; Factor Va; Hemophilia; Vitamin K; γ-carboxyglutamate Lecture 15 and review assignment 5: Blood clotting. Fibrinolysis, plasminogen; tissue plasminogen activator Lecture 16: Regulation of protein function and metabolic control. Lecture 17: Review of glucose metabolism, glycolysis and pentose phosphate pathway. Lecture 18 and review assignment 6: Pentose phosphate pathway balance sheet and experimental tests. Lecture 19: Midterm review. Lecture 20: Control of glycolysis and gluconeogenesis at the phosphofructokinase-1 step. Lecture 21 and midterm post-mortem: Final steps of gluconeogenesis; fructose-1,6-bisphosphatase; Fructose-2,6-bisphosphate. Lecture 22: Glycogen synthesis and glycogenolysis. Glycogen phosphorylase; glycogen synthase; UDP-glucose pyrophosphorylase Lecture 23: Fatty acid synthesis. Fat metabolism; Fatty acid synthesis, Acetyl CoA carboxylase. Lecture 24 and review assignment 7: Fatty acid biosynthesis (continued). Fatty acid biosynthesis cycle; phosphopantotheine; Coenzyme A; ACP. Lecture 25: Products of Lipid metabolism: Triacylglycerols; Phosphatidate; phospholipids; Micelle; Bilayers; Adipose cells; hormone sensitive lipase; Insulin Lecture 26: Integration of metabolism - Who does what. Liver, Brain; Muscle; Kidney; Adipose Tissue. Lecture 27 and review assignment 8: Metabolic crossroads. Lecture 28: Lecture 29: Membranes and Transport: Integral membrane proteins; Peripheral membrane proteins; receptors; structural components; proteins responsible for transporting substrates Glycoproteins and glycolipids, Blood groups, antigens and antibodies Lecture 30 and review assignment 9: Membranes and transport: Basis of protein mediated transport; uniport; antiport; symport; simple diffusion; facilitated diffusion; active transport; electrogenic transport; ion-pumping ATPase Lecture 31: Membranes and Transport: Ion-pumping ATPases; Na+/K+ ATPase; ion gradients; membrane potentials; Nernst equation. Lecture 32: Electrical activity in membranes: selectivity. Nerve action; voltage gates; ion selective; ion Lecture 33 and review assignment 10: Na+ channel; K+ channels; Tetrodotoxin; Digitoxin Lecture 34 and review: Review of Membrane Function. Lecture 35: Semester review. Check-list of Chemical Formulae and Required Structures: Nature of covalent bond; non-covalent bond; salt linkages (electrostatic bonds); hydrogen bond. Oxygen, carbon dioxide, carbon monoxide, cyanide anion. Pyrrole, tetrapyrrole, methene bridge. Histidine, lysine, glutamate, glutamine, apartate, asparagine, serine, cysteine. 2,3 bisphosphoglycerate, carbamate. Carbamoylphosphate, N-carbamoylaspartate, N-phosphonoacetyl-L-aspartate (PALA) and transition state for ATCase. Reagents: p-hydroxymercuribenzoate (p-HMB) and di-isopropylfluorophosphate (DIFP). Oxidative phase of the pentose phosphate pathway (to ribulose 5 phosphate). Glucose (Glc), and its phosphates; UDP-Glc; Fructose (Fru) and its phosphates. Cyclic 3'-5' adenosine monophosphate (cAMP). Fatty acid synthase pathway, triacylglycerol, phosphatidylcholine. N-acetylglucosamine (GlcNAc); N-acetylgalactosamine (GalNAc); ceramide (N-acyl-sphingosine). Check-list of Metabolic Controls and Mechanisms: Myoglobin and hemoglobin, functions in oxygen binding. Effects of BPG, H+, CO2 on oxygen binding. Bohr effect and its causes. Sickle cell anemia, thalassemia, Southern blotting method for determining defects. Control of enzyme activity, ATCase, allosteric regulation by Asp, CTP, ATP. ATCase structural studies, use of PALA. Michaelis-Menten binding (hyperbolic) versus non-hyperbolic (allosteric, co-operative, sigmoidal). Concerted versus symmetric mechanisms of allosteric behaviour. Zymogens and blood clotting; serine proteases in clotting. Seven serine proteases: thrombin, VIIa, IXa, Xa, XIa, XIIa and kallikrein. Thrombin action on fibrinogen; also on factors V, VII, VIII, and XIII. Fibrinogen -> soft clot -> hard clot, transamidation. Extrinsic (tissue factor) cascade and intrinsic (surface contact) cascade. Hemophilias A and B; anticoagulants, antithrombin III. Fibrinolysis, plasminogen and tPA. Calcium ion and phospholipid roles in clotting. Pentose phosphate pathway, its location, controls, and regulation by NADP+. Tests for P.P.P. and a balanced equation for glucose oxidation. Glycolysis and glycogenolysis. (Glycogen to 3-phosphoglyceraldehyde). Phosphofructokinase-1 and its control; Fru-1,6 bisphosphate 1-phosphatase. Allosteric regulation by Fru 2,6 bisphosphate and the bifunctional enzyme. Covalent regulation of the bifunctional enzyme. Cyclic AMP dependent protein kinases; protein phosphorylation cascades; Glucagon, epinephrine, insulin, modes of action. Protein phosphatases. Glycogen breakdown and synthesis; controls of glycogen phosphorylase and glycogen synthase. Liver versus muscle, differences in glycogen and glucose metabolism. Fat synthesis, acetyl CoA carboxylase; fatty acid synthase in mammals. Integration of metabolism, cross-road compounds, tissue specialization. Fasting and starvation, mobilization of glycogen and fats. Membrane structure and function. Ionic gradients and membrane potentials; Nernst equation. Glycolipids and sphinglipids. Glycoproteins, antigens, ABO (ABH) blood groups. Na+/K+ ATPase and the sodium pump. Na+ channel, K+ channel, and voltage gating. The action potential. Acetylcholine receptor and ligand gating. Chem*3560 Assignment 1 1 How many Angstrom units (D) are there in a metre? 2 Why is heme (Fe II-protoporphyrin IX) not used to transport or store oxygen? 3 Which molecules probably evolved first: respiratory cytochromes; chlorophylls; hemoglobins? 4 What is a pyrrole? 5 Why are the amino acids of myoglobins and hemoglobins labelled after the regions (domains, helices) and not numbered in sequence as for other proteins? 6 What is the function of the E7 His of myoglobins and hemoglobins? 7 What is a methene bridge? 8 What chemical differences does the ferrous iron show when it is in myoglobin or hemoglobin as Fe(II)-heme, compared to FeSO4. 9 Answer Yes or No to the questions in the following table: Fe(II) heme Myoglobin Hemoglobin Contains protein? Water-soluble? Binds O2 reversibly? Reduced CO binding? Co-operative or allosteric O2 binding? 10 What would be the physiological effect of replacing Hb4 within erythrocytes (R.B.C.) with myoglobin? 11. If carbon monoxide binds to the Fe(II) of hemoglobin 200 times better than oxygen binds, what percentage of carbon monoxide in air is equal in binding power to that of 20% oxygen in air? Chem*3560 #2 1 What are the structural differences between myoglobin (Mb) and hemoglobin (Hb)? 2 What are structural similarities between Mb and Hb? 3 What are the functional differences between Mb and Hb? 4 Which of the following does not describe the binding of O2 by Hb: (a) Sigmoidal (b) Cooperative (c) Hyperbolic (d) Allosteric. 5 Why is n in the Hill equation never larger than the number of oxygen binding sites for hemoglobin? 6 Oxygen concentration in the lung is much lower than in the air. Why? 7 Define P50 as used in the Hill equation. 8 Why is P50 similar to the Km for an enzyme reaction? 9 Why is blood bank blood thrown out after a few weeks of storage? 10 "R" state Hb is identical to: (a) Oxyhemoglobin (b) Deoxyhemoglobin (c) the Hb conformation with high O2 affinity (d) the Hb conformation with low O2 affinity (e) the Hb conformation that binds BPG 11 Decreased affinity of Hb for O2 is given: (a) at higher pH (c) at higher [H+] (d) at lower [BPG] (b) at lower [CO2] 12 Fetal Hb, Hb F, has a reduced capacity to bind BPG. What effect will this have on the affinity of Hb F for oxygen, and what physiological advantage will this achieve? 13 What structural differences does high resolution X ray diffraction reveal for oxyHb compared to deoxyHb? Chem*3560 #3 1 What is the easiest way to determine if a solution of hemoglobin is oxygenated or not? 2 Why is cyanide CN- poisonous, and why is nitrite NO2 - which forms methemoglobin, used to treat victims of cyanide poisoning? 3 Why is sickle cell anemia more commonly found in West Africans than in the U.S. black population whose ancestors came from West Africa? 4 What makes thalassemias different from the anemias caused by genetic variants of Hb structure? 5 Where might you expect to find the highest proportion of thalassemias among the population?(A) Guelph, Ontario (B) Anchorage, Alaska (C) Moscow, Russia (D) Edinburgh, Scotland (E) Beijing, China 6 DNA analysis is preferred as a method of testing fetuses for the sickle cell condition. Why not test for HbS directly? 7 In "Southern blotting", the specific radioactive probe used is: (A) a small DNA fragment (B) an antibody (C) messenger RNA (D) a small peptide (E) transfer RNA 8 Why is DNA in the region of the sickle cell gene (βs) cleaved only twice by the restriction endonuclease enzyme that cleaves the normal β-globin gene region three times? 9 Butyrate CH3.CH2.CH2.COO promotes transcription of the γ globin gene. Why does this help to - alleviate sickle cell anemia? 10 Would butyrate therapy help all thalassemia patients? Chem*3560 #4 1 Draw the activation energy barrier curve for an endergonic reaction. Which point corresponds to the "transition state" and what is the effect of a catalyst on the shape of the curve? 2 What methods reveal that aspartate transcarbamoylase has quaternary structure? 3 What is the effect of p-hydroxymercuribenzoate on the enzyme activity of ATCase? 4 β-Mercaptoethanol (2-thioethanol) is used in biochemistry as : (A) positive allosteric modulator (B) negative allosteric modulator (C) oxidizing agent (D) reducing agent (E) denaturing agent 5 Why is PALA (N-phosphoacetyl-L-aspartate) used to study binding to the active site of aspartate transcarbamoylase (ATCase), instead of N-carbamoyl phosphate and L-aspartate? 6 What effect does PALA have on ATCase activity? 7 Complete the table: ATCase subunit(s) c6r6 c3 r2 c r Catalytic activity? + or Heterotropic allosteric behaviour? Binding to CTP or ATP? Binds substrates fully? 8 Large particles usually sediment in the ultracentrifuge faster than small particles. Why does ATCase plus PALA sediment more slowly than ATCase alone? 9 Classify the following pairs of proteins and their ligands as (a) positive or negative; (b) homotropic or heterotropic: (1) Hemoglobin A:O2 (2) Hemoglobin A:BPG (3) Hemoglobin A:CO2 (4) ATCase:ATP (5) ATCase: carbamoylphosphate and L-aspartate 10 The concerted or symmetric model (M-W-C model) for allosteric effects only explains positive homotropic effects and not negative homotropic effects. Why? 11 For the normal binding of Hb A tetramer to 4 O2, is the concerted (symmetric) model or the sequential model the best explanation of allosteric behaviour? 12 Protein structures in texts are often represented as below. What secondary or tertiary structural features can you deduce from the diagram? 13 Two proposed conformations for a single protein are shown below. In conformation I, this protein is a harmless normal component of cells. In conformation 2, it is an infectious lethal agent of disease, called a prion. How could a single protein be a cause of infectious disease transmitted from one individual to another? How could a protein reproduce itself? Clue: think of co-operativity between protein subunits, as in hemoglobin or ATCase. A full answer is found in AScientific American@ January 1995, pages 48 - 57, and on the web pages http://www.airtime.co.uk/bse/welcome.htm http://www.diseaseworld.com/ http://www.sciam.com/0195issue/prion.html Chem*3560 #5 1 How could you tell if a patient with a blood clotting deficiency has a defect in the "extrinsic pathway" or in the "intrinsic pathway". 2 Aspirin reduces the clotting rate and increases the "bleeding time" of a patient, by reducing the number and activity of platelets. Why should this slow the rate of clotting? ( Give 3 reasons ). 3 What kind of chemical bonding occurs when fibrin clots? 4 Why is a blood clot red in colour? 5 What laundry advice would you offer to a mass-murderer who wishes to get blood stains out of her sheets? 6 Why does fibrinogen not polymerize whereas fibrin does? 7 Prothrombin binds to cell surfaces through Ca2+, but thrombin does not. Why? 8 Why does dicoumarol in "sweet clover" cause hemorrhagic disease in cattle? 9 In hemorrhagic disease in cattle, transcription and translation of the prothrombin gene is the same as in normal cattle, yet prothrombin does not bind to calcium as does the normal prothrombin. Why? 10 In what ways does thrombin resemble trypsin or chymotrypsin? 11 Why is the tissue-type plasminogen activator (tPA) often injected into patients immediately after they have suffered a coronary artery blockage of the heart or a "stroke" (clot in the brain)? 12 Classic hemophilia (type A) is a deficiency of factor________ and hemophilia type B is a deficiency of factor ___________. 13 What are the common biochemical features in proteolysis by the seven serine proteases of the blood clotting cascade? Chem*3560 #6 1. Define the terms glycolysis; glycogenolysis; gluconeogenesis. 2. You have isolated an animal tissue of unknown metabolism, which use glucose as its energy source. How do you test the route of glucose breakdown in this tissue? Give three tests. 4. Why should mammalian liver, which carries out 90% of glucose breakdown by the aerobic glycolytic route, at the same time carry out the pentose phosphate pathway for glucose oxidation? 5. Why should mammalian liver, at the same time as carrying out glycolytic and pentose phosphate path breakdown of glucose, also be capable of the synthesis of glucose? 6. Which of the following sugar phosphates would you expect to show mutarotation, that interconversion in water between α and β anomers? Fru-2,6-bisphosphate; Fru-1,6-bisphosphate; Fru-6-phosphate; Ribulose-5-phosphate. is, 7. The phosphofructokinase enzyme and the fructose 1,6 bisphosphate-1 phosphatase catalyze the same reaction in opposite directions. (A) What are the essential differences in the two reactions? (B) What would be the result of both reactions acting simultaneously? (C) What physiological benefit could be derived from (B)? (D) What physiological harm (pathology) could arise from (B)? 8. When fructose 6 phosphate accumulates in glycolytic tissues such as liver, a small amount is converted to fructose 2,6 bisphosphate. What effect will this synthesis have on the breakdown and synthesis of Fru-6-phosphate? 9. If a major function of the pentose phosphate pathway is to supply reducing power for biosynthetic reductions, what molecule would you expect to be the major controlling factor in this pathway? (A) NADP+; (B) NAD+ ; (C) ATP ; (D) NADH 10. Which of the following ratios is maintained HIGH in a tissue which breaks down glucose? (A) NADH/NAD+ ; (B) NADPH/NADP+ ; (C) AMP/ADP ; (D) ADP/ATP 11. How does a tissue like liver, which produces both NADH and NADPH, manage to maintain a low ratio ( reduced / oxidized) for one and a high ratio for the other? 1. Chem*3560 #7 If you assume that caffeine acts only by affecting cyclic AMP levels, what effect would you predict for caffeine on the level in liver of: (A) Glycolysis (B) Glycogenolysis (C) Gluconeogenesis (D) Fru 2,6 bisphosphate 2. The enzyme Glc 6-phosphatase, which hydrolyzes Glc 6-phosphate to yield free Glc and Pi is found in liver but not in muscle. Why? 3. Protein kinases are enzymes that transfer phosphate groups from ATP to side chains on protein amino acid residues: (A) Thr (threonine) (B) Ser (serine) (C) Tyr (tyrosine) (D) Cys (cysteine) 4. In bacteria, cyclic AMP is made in response to (A) excess glucose in medium (B) low glucose in medium (C) glucagon in medium 5. In intestinal (gut) tissue, a toxin made by the cholera bacterium binds to a G protein associated with hormone receptor and adenylate cyclase, and results in the massive secretion of salts and water into the gut (diarrhea). What does this suggest about the control of water secretion? 6. Cystic fibrosis is the most common genetic defect in Caucasians. It causes dry mucus to accumulate in the lungs, due to the lack of water and chloride ion secretion across mucus membranes. It is due to a defect in chloride ion transport from the cell to the exterior, and so less chloride ion and water enter the gut and lungs. What benefit could this defect confer on heterozygotes, which would lead to the conservation of this deadly genetic disease? 7. The pancreatic hormone insulin has the opposite effect on blood glucose to that of glucagon. Would you expect insulin to be secreted mainly (A) before a meal (B) after a meal (C) during fasting or starvation? 8. Why is a branched glucose polymer (glycogen) a much better storage form of glucose than a linear glucose polymer such as amylopectin which is part of starch? 9. There are numerous genetic diseases that result in the lack of muscle enzymes for glycogen breakdown, including defective phosphorylase, branching enzyme, debranching enzyme etc. What symptoms might you predict for these diseases? 10 The bifunctional or tandem enzyme ( phosphofructokinase 2/ FBP-2-phosphatase); and glycogen phosphorylase; and glycogen synthase, are all (A) activated by serine phosphorylation (B) inactivated by serine phosphorylation (C) directly regulated by the same protein kinase (D) controlled through cAMP-dependent serine kinase cascades. 11. What processes lead to the lowering of phosphorylase activity in liver or muscle cells? What conscious actions can you take to lower this activity in muscle and liver? Chem*3560 #8 1. Muscle glycogen phosphorylase has sites on the enzyme for the binding of: (A) ATP (B) AMP (C) Pyridoxal phosphate (D) Glycogen (E) Glucagon 2. Protein phosphatase 1, an enzyme that dephosphorylates glycogen phosphorylase, hydrolyzes the serine phosphate residue on: (A) phosphorylase b T-form (B) phosphorylase a T-form (C) phosphorylase b R-form (D) phosphorylase a R-form. 3. Phosphorylase kinase in muscle is activated by (A) phosphatase action (B) calcium ion (C) cAMPdependent protein kinase (D) glucose. 4. Fill in the following table for the effects of high and low blood glucose on the levels of enzymes and metabolites ( High or Low) in liver: Blood Glucose Cyclic AMP Glycogen phosphorylase Glycogen Synthase Protein phosphatase I Low High 5. Fill in the following table to show how fatty acid synthesis contrasts with β-oxidation of fatty acids, in mammals: β-Oxidn. Cell location Electron carrier Thioester involved Units +/- Mitochondria NAD+ 6 NADH Acyl-CoA Acetyl removed Fatty Acid Synthase 6. What would you consider to be the major differences between the organization of β-oxidation enzymes, and fatty acid synthase in the mammalian liver? 7. What B vitamins (or cofactors, or prosthetic groups) would you expect to be vital for the synthesis of fat in mammals? 8. What factors regulate acetyl-CoA carboxylase activity in mammals? Chem*3560 #9 1. The build-up of the TCA cycle intermediate, citrate, will: (A) Inhibit acetyl-CoA carboxylase (B) Stimulate glycolysis (C) Inhibit glycolysis (D) Stimulate synthesis of malonyl CoA. 2. In the liver, the compound at the junction of glycolysis, gluconeogenesis, pentose phosphate pathway, glycogen synthesis and glucose uptake/secretion is: (A) Glucose 1-phosphate (B) Glucose-6-phosphate (C) UDP-glucose (D) Fructose-6-phosphate (E) 6-phosphogluconate. 3. A common starting point for the synthesis of fatty acids, sterols, ketone bodies and citrate is: (A) Malonyl CoA (B) 3 hydroxy 3 methyl glutaryl CoA (C) Acetoacetyl CoA (D) Acetyl CoA (E) Malonate. 4. In prolonged starvation, the principal fuel for the brain is provided by: (A) Ketone bodies (B) Amino acids (C) Glucose (D) Glycogen (E) Triacylglycerols. 5. In early starvation, a major source of energy for the synthesis of glucose in the liver is: (A) Protein (B) Fat (C) Glycogen (D) Ketone bodies. 6. When glucagon is released into the blood, what effect might you expect on blood levels of the following: (A) Blood glucose (B) Blood fatty acid (C) Blood glycerol. 7. What chemical composition would you expect for a typical plasma membrane? (A) High lipid (B) High protein (C) No carbohydrate (D) No nucleic acid . 8. Compared with extracellular fluids, the cytosol has: (A) Low K+ (B) Low protein (C) Low Ca++ (D) Low Mg++ (E) Low phosphate. 9. Compared with intracellular fluid (cytosol), the extracellular fluids have: (A) High K+ (B) High chloride (C) High Mg++ (D) High phosphate (E) High Na+. 10. Predict which of the following lipids are amphipathic and will therefore form ordered structures in water: (A) Fatty acid, Na salt (B) Fatty acid methyl ester (C) Fatty acyl CoA (D) Fatty acid, protonated form. 11. Which of the following would you expect to pass easily across the plasma membrane lipid bilayer? (A) NaCl (B) H2O (C) Glycerol (D) 2,3 bis-phosphoglycerate (E) Glucose-6-phosphate. Chem*3560 #10 1. N-Acetyl-D-glucosamine residues are found in glycoproteins often linked to the side chains of (A) Asparagine (B) Aspartate (C) Alanine (D) Serine (E) Threonine. 2. Cerebrosides are glycolipids which contain (B) Ceramide (C) N-Acyl groups 3. Cell surface antigens of the human ABO blood groups are found (A) In human plasma (B) In human serum (C) On human lymphocytes (D) On human erythrocytes (R.B.C.) (E) Only on human glycoproteins. 4. The Rhesus antigen on the surface of Rhesus-positive fetal RBC can cause antibody production in the maternal serum of Rhesus-negative mothers, which leads to hemagglutination in the blood of new born infants (blue babies). Why are such mothers given intra-venous anti-Rhesus antibodies at all births? (A) To titrate antigen (B) To agglutinate the baby's RBC (C) To make anti-antibody antibodies 5. The digitalis (foxglove) component, digitonin, will stop the heart by irreversibly binding to the Na+/K+ ATPase. However, a smaller amount of digitonin will strengthen the heart muscle contraction, by increasing the Ca++ content of heart muscle cells. What does this tell you about the mechanism for controlling Ca++ inside these cells? (A) There is a Na+/Ca++ symport (B) There is a Na+/Ca++ antiport (C) A Ca++-ATP-ase is needed for Ca++ export. 6. A clumsy murderer might make use of digitalis to poison her victim. A clever murderer would achieve the same deadly effect by intravenously injecting: (A) CaCl2 (B) NaCl (C) KCl. 7. Arsenate As043- and vanadate V043- both are poisons and useful inhibitors in biochemistry. They both act through their chemical similarity to (A) ATP (B) ADP (C) AMP (D) Phosphate (A) Sphingomyelin (D) Choline (E) Phosphate.