History: 65-year-old female with right lower extremity melanoma
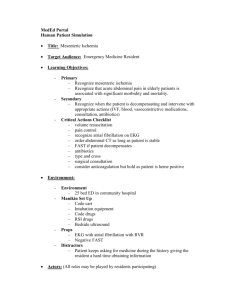
advertisement

Ryan B. O'Malley, MD
Assistant Professor, Body Imaging
Department of Radiology, University of Washington School of Medicine,
1959 NE Pacific St, Seattle, WA 98195.
History: 65-year-old female with right lower extremity melanoma
What is the most likely diagnosis?
a) Mesenteric hemorrhage
b) Mesenteric panniculitis
c) Lymphoma
d) SMV thrombosis with mesenteric edema
1
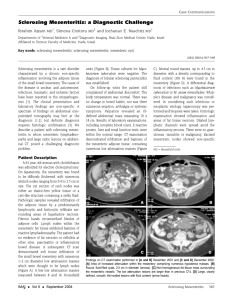
Findings:
Mesenteric fat stranding (“misty
mesentery”) surrounding non-enlarged LN
Preserved fat halo around the vasculature
Tumoral pseudocapsule
Benign idiopathic inflammatory process
involving the mesenteric fat
Commonly incidentally detected in
patients being imaged for other reasons
(including malignancy)
Autopsy series reported up to 1%
Does not progress or evolve into
malignancy
Subtype of sclerosing mesenteritis –
spectrum based on the predominant
imaging findings and tissue type
Mesenteric panniculitis – ill-defined
inflammation without discrete soft tissue
or mass
Histology: Heterogeneous chronic
inflammatory infiltrate
Mesenteric lipodystrophy – fat necrosis
Histology: Lipid-laden macrophages
Retractile mesenteritis – fibrotic soft
tissue mass with retraction and distortion
Histology: Collagen deposition
Abdominal manifestation of IgG4-related
sclerosing disease
RPF
IPT
AIP
Sclerosing cholangitis
2
Imaging:
“Misty mesentery” – nonspecific
term describing increased
attenuation within the mesenteric
fat
Fluid
Fibrosis
Neoplastic infiltration
Fat-ring sign preserved fat halo
surrounding the mesenteric
vasculature
Tumoral pseudocapsule border
outlining the affected mesentery
Lymphoma
DDx:
Lymphoma (after treatment, may be
identical to mesenteric panniculitis)
Edema (e.g. thrombosis, CHF,
pancreatitis)
Hemorrhage
Carcinomatosis
{separate slide with images of
each?}
History: 53-year-old female with fatigue
What is the most likely diagnosis?
a) Lymphoma
b) Sclerosing mesenteritis
c) Carcinoid
d) Metastatic GI stromal tumor
3
History: 53-year-old female with fatigue
Findings:
Clusters of mesenteric and
retroperitoneal LN
Confluent soft tissue encasing
mesenteric vasculature with lost fat halo
Most common malignancy
affecting the mesentery
Primarily spreads via lymphatics
Most common malignant
retroperitoneal tumor
Mesenteric LAD more common in
NHL than HD
~50% of NHL has enlarged
mesenteric LN at presentation
compared to 5% for HD
Coexistent retroperitoneal LAD
helps suggest the diagnosis
4
Imaging:
Can present with LN with a wide range of
size and morphology
Characteristically confluent soft tissue
surrounding and encasing vessels (especially
SMA and SMV) with lost fat halo, but no
narrowing
Sandwich sign – confluent soft tissue on both
sides of mesenteric vessels and perivascular fat
Following response to therapy, may only
see infiltration of the mesenteric fat +/Ca++
FDG PET is most accurate modality, 90-95%
sensitive
DDx:
Sclerosing mesenteritis
Misty mesentery and Ca+ usually only seen in
treated lymphoma)
PTLD
Can also see sandwich sign
Metastatic disease
Typically localized rather than diffuse
Infectious/inflammatory adenopathy (e.g.
TB, Whipple disease)
LN may be rim-enhancing with central necrosis
History: 44-year-old man with enlarging palpable L testicular mass
Which of the following is considered regional LN
in the setting of testicular CA?
a)
b)
c)
d)
Paraaortic
Common iliac
Internal iliac
Inguinal
5
History: 44-year-old man with enlarging palpable R testicular mass
Findings:
Confluent retroperitoneal LN at the level of the
renal veins
No pelvic LN
Right testicular mass
Metastases from testicular CA most
commonly occur in paraaortic region
Lymphatics follow gonadal vessels to
level of the renal hilae
Typically ipsilateral to the primary tumor
May spread inferiorly toward the aortic
bifurcation
Frequently skip the pelvic LN (unless
there has been prior inguinal or scrotal
surgery; e.g. post-orchiectomy)
Always consider testicular CA in DDx
for male patients with retroperitoneal
LN
Testicular germ cell tumors (95% of
testicular CA)
Seminoma (60%)
LN usually soft tissue attenuation
Nonseminomatous
LN usually more cystic
Stage II
Pure seminoma + regional LN
Staged based on maximum diameter of
Paño B et al. RadioGraphics. 2011 Jan-Feb;31(1):135-60.
involved LN
Stage IIA: ≤2 cm RT
Stage IIB: >2 and ≤5 cm RT or chemo
Stage IIC: >5 cm chemo (cisplatin-
based)
6
DDx – retroperitoneal soft
tissue mass(es):
Lymphoma
Metastatic LN
Most commonly pelvic source
(e.g. ovary, testis, prostate,
uterus)
Mesenchymal tumor
Leiomyosarcoma
Liposarcoma
Retroperitoneal fibrosis
Hematoma
Paño B et al. RadioGraphics. 2011 Jan-Feb;31(1):135-60.
History: 60-year-old female with intermittent left flank pain
Which of the following is an
abdominal manifestation of IgG4related sclerosing disease?
a)
b)
c)
d)
Primary biliary cirrhosis
Whipple syndrome
Castleman’s disease
Retroperitoneal fibrosis
7
History: 60-year-old female with intermittent left flank pain
Findings:
Infiltrative retroperitoneal soft tissue
encasing aorta and IVC, tethering
toward the spine
Left renal obstruction with delayed
nephrogram and medial deviation of
the left ureter
Confluent peri-pancreatic soft tissue
Inflammatory and fibrotic plaquelike
retroperitoneal mass or soft tissue,
which encases aorta, IVC, and ureters
Presents in middle age (40-60 y/o),
men 2-3x more common than women
Non-specific presentation – flank or
back pain, fever, fatigue, decreased
urination, malaise
Majority (>70%) are idiopathic, exact
mechanism uncertain
Increasingly recognized as systemic
inflammatory condition
Abdominal component of IgG4-related
sclerosing disease along with other
fibroinflammatory conditions
Some suggest an immune response to
leaking antigens from atheromatous
plaque within the aorta
Secondary causes
Ergot derivatives (e.g. mehysergide) are
most common
Coexistent malignancy in up to 8%,
possible a desmoplastic reaction to
underlying retroperitoneal metastases
8
Imaging:
Infiltrative retroperitoneal
soft tissue, most commonly
along the aorta and common
iliac arteries (centered at the
aortic bifurcation)
Can be more extensive
Anteriorly pancreas and
duodenum
Craniocaudally mediastinum
or pelvis
Bilateral or unilateral ureteral
encasement results in medial
deviation and obstruction
Enhancement and T2 SI
reflects the degree of
inflammation
Acute phase – avid
enhancement, T2 SI
Chronic/fibrotic – little to no
enhancement, low SI on T1 and
T2
DDx:
Lymphoma
Metastatic disease (e.g. colon,
prostate, testicular)
Hematoma
Postirradiation
Imaging cannot reliably
distinguish benign from
malignant RPF!
Benign/idiopathic RPF is
classically plaquelike and
tethers the aorta and IVC
toward the spine, reflecting
underlying fibrosis
Malignancy tends to be bulkier
and lobulated, displacing aorta
and IVC anteriorly and ureters
laterally
Poor sensitivity and specificity
of these (and other) features
and many exceptions exist
Biopsy may be required (often
surgical)
9
Management
Treat underlying cause and/or
remove causative agent
Some drug-induced causes also
respond to immunosuppresion
Glucocorticoids (usually
prednisone) – high-dose
initially, followed by taper and
maintenance therapy
If renal impairment, PCN and
ureteral stent
History: 54-year-old female with increasing abdominal girth over 1 year
What is the most likely diagnosis?
a)
b)
c)
d)
Dermoid
Angiomyolipoma
Myelolipoma
Liposarcoma
10
History: 54-year-old female with increasing abdominal girth over 1 year
Findings:
Large retroperitoneal mass containing fat, soft
tissue nodules, and septations
Mass effect upon, but separate from,
retroperitoneal structures
Coarse Ca++
Most common primary retroperitoneal
malignant tumor
80% of all retroperitoneal tumors are
malignant (lymphoma most common,
followed by sarcoma)
>90% of retroperitoneal sarcomas are
liposarcoma or leiomyosarcoma
2nd most common adult soft tissue
sarcoma (after MFH)
Malignant from inception almost never
arise from lipomas
No fat-containing retroperitoneal lesion
should be dismissed as a lipoma
retroperitoneal lipomas are exceedingly
rare, more likely represents lipomalike
area of a well-differentiated
liposarcoma
Grow slowly and are very large at
detection
Results in longer time to diagnosis
more likely to dedifferentiate
15% of well-differentiated liposarcomas
dedifferentiate (median 8 years)
5 histologic types
Well-differentiated
Myxoid
Dedifferentiated
Pleomorphic
NOS
11
Imaging:
Large heterogeneous mass with
varying components of fat,
fibrous strands, & soft tissue
Mixed (most common) – fat (< -20
HU) and non-lipomatous
components (soft tissue, fluid)
Solid (myxoid tissue) – T2
hyperintensity with enhancement
Pseudocystic (-20-20 HU) – mimics
fluid collection
Displaces retroperitoneal
structures
Identify kidneys and adrenals
separately to distinguish from
AML or myelolipoma
Regional LN involvement is rare
Mets most commonly lung and
liver
Well-differentiated
Predominantly fat and fibrous
septations
Myxoid
Craig WD et al. RadioGraphics. 2009 Jan-Feb;29(1):261-90
Uniform low attenuation with
increased SI on T2W
Dedifferentiated
Discrete nodular soft tissue > 1
cm
Discrete soft tissue components
are the hallmark of
dedifferentiation
12
Craig WD et al. RadioGraphics. 2009 Jan-Feb;29(1):261-90
DDx:
AML
Large internal vessels, renal
notch, hemorrhage
History of tuberous sclerosis
Myelolipoma
Most (90%) arise from adrenal,
but extra-adrenal type can mimic
sarcoma
Hematoma
May be secondary to AAA
rupture or tumor (e.g. RCC, ACC,
AML)
Management:
Surgical resection
Very difficult to obtain clear
margins
Frequently recurs and
becomes more aggressive
Recurrence most commonly as
soft tissue rather than fat
13
History: 60-year-old male with weight loss and facial flushing
Fused CT and OctreoScan
In what percentage of patients does carcinoid
syndrome occur?
a)
b)
c)
d)
>90%
50%
30%
<10%
History: 60-year-old male with weight loss and facial flushing
Fused CT and OctreoScan
Findings:
Spiculated mesenteric mass in the RLQ with
encasement of vasculature and tethering of
small bowel loops
Mesenteric mass and liver lesions have uptake
on OcreoScan
14
Uncommon neuroendocrine tumor
arising from the endocrine system
outside the pancreas and thyroid
~2% of all GI tract tumors
Most common malignant
neoplasm of the small bowel
Most commonly distal ileum
Primary tumor is a small (< 3.5
cm) submucosal mass that is
usually occult by imaging
40-80% spread to mesentery
(directly or via lymphatics)
Typically the first or only imaging
manifestation (unless there are
hepatic metastases)
Imaging findings are a result of
extramural spread and resultant
desmoplastic reaction in the
mesenteric fat retraction and
tethering
Imaging:
Enhancing calcified, soft tissue mass with
spiculation of the mesenteric fat, tethering
of adjacent bowel and vasculature
Metastatic disease becomes more common
with larger tumors (> 1 cm)
Regional LN
Liver (usually hypervascular)
5-year survival 79% for <5 lesions vs. 47% for ≥5
Peritoneum
Carcinoid syndrome (<10%)
Refers to a constellation of symptoms – flushing,
diarrhea, wheezing, right heart failure
90% have metastatic disease, most commonly
patients with liver metastases tumor products
(e.g. histamine, serotonin) released into systemic
circulation
Majority originate in midgut (jejunum, ileum,
cecum), bronchial in 10%, rarely distal colon and
rectum
111In pentetreotide helps distinguish from
other etiologies and predict response to
octreotide therapy (80% have somatostatin
receptors)
DDx:
Desmoid
Hematoma
Retractile mesenteritis
Treated lymphoma
{more detail for these? Separate slide?}
15
Management:
Localized, non-metastatic resection
Extent depends on origin and size
Post-treatment surveillance often
continues for up to 10 years due to late
recurrence
Carcinoid syndrome
Somatostatin analogs (e.g. ocreotide) –
bind to somatostatin receptors and block
release of active tumor products
Hepatic resection
Considered for select patients with
localized disease, preserved liver
function, and no extrahepatic disease
Symptomatic relief in most patients,
disease-free survival in up to 20%
Liver-directed therapy
Bland or chemoembolization, ablation,
and 90Y have been shown to improve
symptoms in unresectable cases
Prophylactic octreotide required to
prevent carcinoid crisis
History: 29-year-old female status post total proctocolectomy with abd pain
Which of the following describes Gardner
syndrome?
Ectopic gallstone with gastric outlet obstruction
RCC, pancreatic cysts, hemangioblastoma,
pheochromocytoma
c) Lung cysts and RCC
d) Colorectal polyps, skull osteomas, desmoid
tumors, epidermoid cysts
a)
b)
16
History: 29-year-old female status post total proctocolectomy with abd pain
Findings:
Infiltrative mesenteric soft tissue in RLQ
Tethering and spiculation of surrounding
structures
AKA aggressive or deep fibromatosis
Fibromatoses – benign, but locally
aggressive proliferation of fibrous or
connective tissue
Superficial – smaller, slow-growing,
rarely involve deeper structures
Deep – larger, more aggressive, grow
rapidly, infiltrate surrounding
structures
Abdominal wall – classically young
women during pregnancy or within 1 year
postpartum
Intraabdominal – mesenteric,
retroperitoneal, and pelvic
Can be familial or sporadic
Mesenteric desmoids are associated
with patients with FAP (Gardner
syndrome) 18-20% of patients with
Gardner syndrome develop desmoids
75% develop in patients with prior
abdominal surgery
17
Variable imaging appearance, frequently
non-specific
Masslike or ill-defined (and both forms
can coexist in same patient)
Infiltrative types may encase bowel loops and
vasculature
Masslike types tend to displace rather than
encase
Spiculated with radiating strands of soft
tissue and retraction of surrounding
structures
Similar attenuation/SI to muscle, but can
become necrotic when large
Usually low SI on T1; If myxoid high SI
on T2
Imaging primarily used to plan surgical
resection
Size and number of lesions
Local extent – vasculature, bowel, solid
organs
DDx:
Carcinoid
Sclerosing mesenteritis
Metastasis
Lymphoma
History: 64-year-old male with LLE numbness, new hemorrhagic brain lesions
What is the most likely diagnosis?
a)
b)
c)
d)
Desmoid
Metastatic melanoma
Metastatic colorectal cancer
GIST
18
History: 64-year-old male with LLE numbness, new hemorrhagic brain lesions
Findings:
Dominant lobulated sigmoid mass with
eccentric wall thickening
Multiple round, circumscribed
mesenteric masses
Numerous tiny subcutaneous nodules
Skin cancer arising from melanocytes
Most in sun-exposed areas, but can
develop elsewhere
Mucosal melanoma 1% of all melanoma
Primarily head & neck, anorectal,
vulvovaginal
Worse prognosis than cutaneous primary
LN disease starts regionally and
progresses contiguously through the
lymphatic chain
Can metastasize hematogeneously to any
organ
More common in advanced regional
disease
Distant metastases can occur even
without regional LN spread
60% of metastatic melanoma have
abd/pelvis mets
Most common sites of metastases:
Regional LN (75%)
Lung (70%)
Subcutaneous/soft tissues (67%) – in
transit, between primary and regional LN
Liver (58%) – most common visceral site
CNS (49-73%)
GI tract (40%)
Spleen (5%)
19
Small bowel and mesentery are most common site of
GI metastases
GI tract
Can present anywhere in the GI tract, but usually
multiple
Small bowel more common (75%) than colon (25%)
Intramural, serosal, or polypoid intraluminal masses
Target appearance with central necrosis or ulceration
Aneurysmal SB dilation
Eccentric wall thickening
Mesentery and LN
Mesentery and omentum usually both involved
Lobulated, confluent, or infiltrative patterns (overlap
with lymphoma, carcinoid, and desmoid)
Rarely result in desmoplastic response (contrast to
carcinoid)
Peritoneal or omental carcinomatosis
LN may bleed
Abdominal LN in 30%
PET/CT (with diagnostic CT) most accurate for
staging and assessing for recurrence
Sensitivity 98%, specificity 94%
Detects unsuspected metastases in 15%
Demonstrates blind spots better than CT alone
Management
Metastatectomy – isolated or limited metastatic disease
Immunotherapy (e.g. IL-2, ipilimumab, anti-PD1 monoclonal Abs)
Ipilimumab preferred for most patients, produces durable response in 20%
IL-2 in selected patients can be curative, but severe associated toxicities
Anti-PD1 monoclonal Abs 2nd line after PD with ipilimumab
Radiation therapy
Mostly for brain metastases
Palliative for symptomatic localized disease
20
History: 47-year-old male, fall from 27 feet
What is the most likely diagnosis?
a)
b)
c)
d)
Desmoid
Mesenteric hematoma
Carcinoid
Sclerosing mesenteritis
History: 47-year-old male, fall from 27 feet
Findings:
High attenuation mesenteric fluid
collection displacing adjacent bowel loops
Active extravasation centrally
Pelvic fractures
21
Bowel and mesenteric injuries
found in ~5% of laparotomies for
blunt trauma
CT is the test of choice with
sensitivity 69-95% and specificity
94-100%
Mesenteric hematoma should
prompt search for associated bowel
injury
Imaging:
Ill-defined mesenteric fat stranding
May reflect isolated mesenteric injury
or bowel injury
Highest sensitivity, but nonspecific
Hematoma
Specific to mesenteric injury, but does
not always require surgery
Irregularity of mesenteric
vasculature
Usually indicates underlying vascular
injury
Extravasation of IV contrast –
reportedly 100% specific for
significant mesenteric injury
Usually indicates need for laparotomy
History: 49-year-old dock worker with increased abdominal girth
What is the most likely diagnosis?
a)
b)
c)
d)
Malignant peritoneal mesothelioma
Pseudomyxoma peritonei
TB peritonitis
Mesenteric hemorrhage
22
History: 49-year-old dock worker with increased abdominal girth
Findings:
Diffuse infiltrative soft tissue throughout the
peritoneal cavity
Scalloping of the liver surface
Small amount of ascites
No enlarged LN
Rare aggressive neoplasm
arising from mesothelial cells
lining serosal surface of
peritoneal cavity, spreads
rapidly throughout the abdomen
and pelvis
Peritoneum is 2nd most
common site of mesothelioma
(after pleura), accounting for
10-15% cases annually
Most have h/o asbestos
exposure, but the link is less
strong than for pleural
mesothelioma
Incidence rises sharply at
higher levels of exposure
20-40 year latency
23
Imaging:
Most commonly, diffuse infiltrative
peritoneal soft tissue, including
scalloping of liver or diaphragmatic
surface
Ascites frequently present (60-100%), but
rarely large volume
Pleural Ca++ (50%), thickening, and/or
effusion
Less commonly presents as a dominant
mass with peritoneal nodularity
Distant metastases are rare (consider
alternate diagnosis)
DDx:
TB peritonitis
High attenuation ascites, LN, peritoneal
thickening
Exposure history
Carcinomatosis
Cannot be reliably distinguished by imaging
Lymphomatosis
Usually with LN
Pseudomyxoma peritonei
Serous carcinoma of the peritoneum
Primary arising from ovarian epithelial rests
Management
No consensus, poor prognosis
Median survival historically < 1
year, but up to 5 years at
certain centers
If good performance status
and no extraperitoneal
disease cytoreductive
surgery + hyperthermic
intraoperative peritoneal
perfusion with chemotherapy
(HIPEC)
Systemic chemotherapy for
patients who cannot tolerate
surgery + HIPEC or have
extraperitoneal disease
24
History: 66-year-old female with abdominal bloating and fatigue
What is the most likely diagnosis?
a)
b)
c)
d)
Pseudomyxoma peritonei
Malignant peritoneal mesothelioma
Simple ascites
Perforated appendicitis
History: 66-year-old female with abdominal bloating and fatigue
Findings:
Dilated tubular structure in the RLQ with
punctate Ca++
Mucinous implants displacing bowel loops,
scalloping liver surface
Cystic left ovarian lesion
25
Clinical entity with accumulation of gelatinous
ascites and mucinous implants along peritoneal
surfaces secondary to mucinous epithelial
neoplasia
Histologically bland or low-grade mucinous
epithelium on the peritoneal surface
Most common presenting symptom is increased
abdominal girth
Terminology is confusing and variable, but the
current consensus is that PMP should be used to
describe peritoneal spread in association with
appendiceal mucinous neoplasm
AKA disseminated peritoneal adenomucinosis
(DPAM)
Allows more uniform pathologic and prognostic
classification
Appendiceal tumor obstructs lumen ruptures
with tumor cells disseminated throughout
peritoneal cavity
Appendiceal neoplasm itself is histologically lowgrade, but can result in appendiceal rupture and
peritoneal dissemination, resulting in a more
aggressive clinical scenario
~20% of mucinous tumors of the appendix results
in PMP
Found incidentally in 2/10,000 laparotomies
Disseminated mucin-producing appendiceal
adenocarcinoma (peritoneal mucinous
carcinomatosis) is an aggressive subset with
mucinous epithelium demonstrating features of
carcinoma
Ovarian mucinous tumors are presumed to be
metastatic (present in 44%)
Rare metastases to LN or liver parenchyma
Imaging findings:
Loculated/mucinous ascites
accumulates throughout the
peritoneal cavity in
characteristic locations
(corresponding to areas of fluid
reabsorption and dependent
accumulation)
Greater omentum
Right subphrenic space
Pouch of Douglas
Right retrohepatic space
Liver and spleen surface
Left para-colic gutter
Ligament of Treitz
Centrally displaced bowel loops
Scalloping of liver and spleen
surface
Mucinous appendiceal +/-
ovarian tumors
May have curvilinear Ca++ in wall
or lumen
Left ovary
26
TB Peritonitis
Peritoneal carcinomatosis
DDx:
– Peritoneal carcinomatosis
Burrill et al. RadioGraphics 2007 27:5, 1255-1273
– Peritonitis (e.g. TB, bacterial)
– Peritoneal mesothelioma
Pseudomyxoma peritonei
Malignant peritoneal mesothelioma
Management
Palliative, intended to manage symptoms by reducing accumulation
of mucus
Repeated surgical debulking
Most aggressive approach with curative intent – complete
cytoreduction followed by intraperitoneal heated chemotherapy
Best results at select expert centers with extensive experience (Sugarbaker)
27
![Paper_Prof_Wang_final1[1]](http://s3.studylib.net/store/data/005836194_1-85fb8d8882c087decd1a6d9c9fdc99c0-300x300.png)