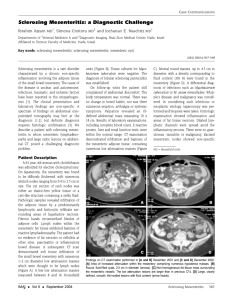
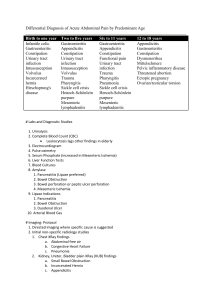
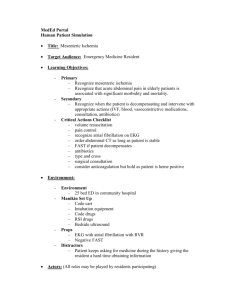
R e s i d e n t s ’ S e c t i o n • S t r u c t u r e d R ev i ew
McLaughlin et al.
Mesenteric Panniculitis and Its Mimics
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
Residents’ Section
Structured Review
Residents
inRadiology
Patrick D. McLaughlin1,2
Antonella Filippone 3
Michael M. Maher 1,2
McLaughlin PD, Filippone A, Maher MM
Keywords: mesenteric panniculitis, mesentery, retractile
mesenteritis, sclerosing mesenteritis
DOI:10.2214/AJR.12.8493
Received December 22, 2011; accepted after revision
June 6, 2012.
1
Department of Radiology, Cork University Hospital,
Wilton, Cork, Munster, Eire, Ireland. Address
correspondence to M. M. Maher (m.maher@ucc.ie). 2
Department of Radiology, University College Cork,
Cork, Ireland.
3
Department of Neurosciences and
Imaging,Section of Radiological Imaging,
“G.d’Annunzio”University, Chieti, Italy.
WEB
This is a Web exclusive article.
AJR 2013; 200:W116–W123
0361–803X/13/2002–W116
© American Roentgen Ray Society
W116 The “Misty Mesentery”: Mesenteric
Panniculitis and Its Mimics
Key Points
1. The term “misty mesentery” was coined by
Mindelzun et al. in 1996 to describe a regional increase in mesenteric fat density that
is seen frequently at abdominopelvic CT.
2.Mesenteric panniculitis (MP) is one of the
broad range of disorders that may result in the
imaging finding of a misty mesentery on CT.
3. MP cannot be diagnosed on CT without the
exclusion of many other possible causes of
a misty mesentery including disorders that
result in mesenteric edema, lymphedema,
hemorrhage, and infiltration with inflammatory or neoplastic cells.
4. Retractile mesenteritis results in irregular
fibrotic mesenteric masses that simulate
a number of neoplastic conditions of the
mesentery and peritoneum such as carcinoid tumors, desmoid tumors, and peritoneal carcinomatosis.
The term “misty mesentery” was coined
by Mindelzun et al. [1] in 1996 to describe a
regional increase in mesenteric fat density at
abdominopelvic CT. This imaging finding is
commonly encountered during review of abdominal CT scans [2]; when a misty mesentery is observed, the radiologist must consider
many pathologic entities involving the mesenteric fat and adjacent organs that may result in
the infiltration of these tissues by fluid, fibrous
tissue, or inflammatory or neoplastic cells.
Mesenteric panniculitis (MP) is one of
the broad range of disorders that may result
in the imaging finding of a misty mesentery
on CT. MP is pathologically characterized
by inflammation and variable amounts of fibrosis and fat necrosis of the mesentery. Although MP is an important potential cause
for a misty mesentery on CT, MP is a diagnosis that requires the exclusion of a range
of important diseases and ultimately may require histologic confirmation [3].
In this article, we describe the key CT findings associated with MP. We outline the imag-
ing features of MP and of a wider spectrum of
related disorders belonging to the parent group
sclerosing mesenteritis. A misty mesentery can
be seen in association with a range of pathologic entities other than MP. Imaging findings
in conditions known to mimic MP are also described in an attempt to provide the radiologist
with a basis for rational differential diagnosis.
Pathophysiology
MP belongs to a continuum of idiopathic
disorders of the mesentery and peritoneum referred to as “sclerosing mesenteritis” [4]. Pathologically, sclerosing mesenteritis can be divided
into three stages. The first stage is mesenteric
lipodystrophy in which a layer of foamy macrophages replaces the mesenteric fat [4]. The second stage is MP in which there is an infiltrate
of plasma cells, polymorphonuclear leukocytes,
and foamy macrophages [4, 5]. The final stage
is retractile mesenteritis, which is characterized
by collagen deposition, fat necrosis, and fibrosis
that leads to tissue retraction [4, 5].
The cause of sclerosing mesenteritis remains unclear, although several possible
causes have been proposed in the literature including previous abdominal surgery, abdominal trauma, autoimmunity, vasculitis, and infection [6]. Sclerosing mesenteritis has been
associated in a number of case studies with a
variety of intraabdominal and extraabdominal
malignant diseases including lymphoma, colorectal carcinoma, gastric carcinoma, renal
cell carcinoma, melanoma, myeloma, chronic
lymphocytic leukemia, and carcinoid tumors
[6]. Currently, there is no clear answer to the
question of how strongly sclerosing mesenteritis is associated with underlying malignancy.
Kipfer et al. [7] reported that 30% of patients
with sclerosing mesenteritis had an underlying
malignancy, whereas Daskalogiannaki et al.
[6] reported a higher rate of 69% of sclerosing mesenteritis patients with coexisting malignancy. Other investigators have found that
AJR:200, February 2013
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
Mesenteric Panniculitis and Its Mimics
the coexistence of malignancy and sclerosing
mesenteritis is not significantly different than
in patients undergoing routine abdominopelvic CT without findings suggesting sclerosing
mesenteritis [8]. The possibility that sclerosing mesenteritis may represent a nonspecific
paraneoplastic response has been suggested,
but available data are limited and the exact relationship between sclerosing mesenteritis and
malignancy remains unclear. There is, however, an established association between sclerosing mesenteritis and other idiopathic inflammatory disorders such as orbital pseudotumor,
retroperitoneal fibrosis, sclerosing cholangitis,
and Reidel thyroiditis [3].
Clinical Characteristics
Sclerosing mesenteritis is reported across
a large age range, typically extending from
the third to the ninth decades. Cases of
sclerosing mesenteritis in the pediatric age
range are rare but have been documented as
case reports in the literature [9]. The most
commonly reported mean age of presentation lies in the seventh decade and a male
preponderance is accepted [4, 7].
Very rarely patients with MP may present
with acute abdominal symptoms including abdominal pain, bloating, nausea, or weight loss
[5], and an abdominal mass may be palpated
in up to 50% of this subgroup [7]. In this subgroup of acutely symptomatic patients, treatment with steroids or a combination of steroids and other drugs such as tamoxifen has
been shown to be beneficial [10]. An increasing proportion of asymptomatic patients continue to be identified when undergoing modern cross-sectional imaging; Daskalogiannaki
et al. [6] reported imaging findings consistent
with MP in 0.6% of 6620 consecutive patients
undergoing routine abdominopelvic CT.
Imaging Findings in Mesenteric
Panniculitis
MP results in a masslike area of heterogeneously increased fat attenuation on CT that
may displace local bowel loops but typically
does not displace the surrounding mesenteric vascular structures [2] (Fig. 1). Ultrasound
may show a well-defined hyperechoic mass
with small central hypoechoic areas or a heterogeneous but predominantly hyperechoic mass [11]. On MRI, a mesenteric mass is
seen with intermediate signal intensity on T1weighted images and with slightly higher signal intensity on T2-weighted images [12]. Mesenteric lymph nodes are often seen within the
region of segmental mesenteric stranding and
nodes may be enlarged to greater than 1 cm in a
small percentage of cases [13]. Approximately
90% of cases involve the small-bowel mesentery [10] and changes are more commonly centered to the left of the midline corresponding
with the jejunal mesentery [14] (Fig. 2).
Important imaging signs of MP include the
“tumoral pseudocapsule” sign (Fig. 3), which
refers to the presence of a peripheral curvilinear band of soft-tissue attenuation limiting
the heterogeneous mesenteric mass from the
surrounding normal mesentery, and the “fat
halo” sign (Fig. 4), which refers to the preservation of normal fat density in the fatty tissue surrounding the mesenteric vessels. The
thickness of the tumoral pseudocapsule band
of soft tissue is typically not greater than 3 mm
[6]. The sensitivities of the fat halo and tumoral pseudocapsule signs were reported as 75%
and 50%, respectively, in a series of 17 pathologically confirmed cases [13]. The specificity
of these signs has not yet been defined to our
knowledge, but radiologists should be aware
that the fat halo sign may also be present in
patients with mesenteric lymphoma [15, 16]
and the tumoral pseudocapsule sign may also
be found in cases of benign and malignant
mesenteric lipomatous tumors [2].
Mimics of Mesenteric Panniculitis
When a misty mesentery is observed on CT,
it is incumbent on the radiologist to consider
and, if possible, exclude alternative causes of a
regional increase in mesenteric fat density such
as edema (Fig. 5), hemorrhage, lymphedema,
inflammation (Fig. 6), and neoplasia (Fig. 7)
before suggesting a diagnosis of MP [1].
Mesenteric Edema
Mesenteric edema may be caused by systemic diseases such as hypoproteinemia or hepatic, cardiac, or renal failure or may be related
to local vascular diseases such as portal hypertension and hepatic, portal, or mesenteric vein
thrombosis. Ascites and fluid in the subcutaneous adipose tissues are not associated with MP;
when these findings are present, the radiologist
should suspect mesenteric edema due to a systemic disease rather than MP. A misty mesentery was identified in 86% of patients with hepatic cirrhosis undergoing abdominal CT [17];
a large number of those patients had evidence
of edema in other adipose compartments but
more than one third of cirrhotic patients may
have evidence of only a misty mesentery.
The pattern of mesenteric edema secondary to mesenteric vein thrombosis tends to be
focal and is typically in continuity with seg-
mental bowel wall thickening, which may indicate the presence of small-bowel ischemia.
Mesenteric Inflammation
Pancreatitis is the most common process associated with inflammation of the small-bowel
mesentery but virtually all other inflammatory diseases of the gastrointestinal tract including cholecystitis, appendicitis, diverticulitis,
inflammatory bowel disease, and infective peritonitis may also result in inflammatory changes
in the adjacent mesentery [3]. Tuberculous peritonitis should be suspected when the following
signs are observed in association with a misty
mesentery [18]: lymphadenopathy with central
hypodensity due to caseous necrosis; nodularity of the mesenteric fat; smooth thickening of
the peritoneum typically with pronounced enhancement; and high-density ascites, which is
proposed to be caused by high protein content.
Mesenteric Hemorrhage
Acute hemorrhage into the small-bowel mesentery typically displays high CT attenuation
values in the range of 40–60 HU. A history of
trauma, anticoagulation therapy, blood dyscrasia, or mesenteric ischemia may be present.
Mesenteric Lymphedema
Primary mesenteric lymphedema, or small
intestinal lymphangiectasia, is a rare disorder
first described in 1961 by Waldmann et al. [19].
Mesenteric lymphedema is associated with
diffuse nodular thickening of the small-bowel
wall resulting from dilated lymphatic channels
within the small-bowel villi. The changes may
be segmental, ascites is usually present, and
small-bowel thickening may assume a stratified appearance due to mucosal or submucosa
edema [20]. Paraaortic and mesenteric lymph
nodes are not usually visible, which may allow differentiation of mesenteric lymphedema from other conditions, such as lymphoma,
Whipple disease, celiac disease, and tuberculosis, all of which can produce diffuse small intestinal wall thickening [21].
Mesenteric Neoplasia
Perhaps the most challenging differential diagnosis to exclude when a misty mesentery is
encountered is early-stage Hodgkin and nonHodgkin lymphoma; lymphoma is the most
common tumor involving the mesentery. Late
stage disease usually presents little diagnostic
difficulty because of the typically bulky mesenteric lymphadenopathy, but early stage disease
can produce mildly enlarged nodes; a misty
mesentery; and, as previously stated, even the
AJR:200, February 2013W117
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
McLaughlin et al.
fat halo sign [15, 16]. Any additional lymphadenopathy seen outside the mesenteric region,
particularly in the retroperitoneum, should immediately raise suspicion for early stage lymphoma [2]. Radiologists should recognize that
treatment response after chemotherapy may
also result in high-density changes in the mesenteric fat that can be indistinguishable from
MP [8] despite an improvement in or even resolution of the mesenteric lymphadenopathy.
Primary mesenteric neoplasms, such as neurofibromas, lipomas, and mesenteric liposarcomas, can mimic MP and may also display a
curvilinear rim of soft tissue surrounding their
peripheral margins mimicking the previously
described tumoral pseudocapsule sign [2]. An
imaging finding that can help in distinguishing
these rare neoplasms from MP and other benign pathologic processes is visible mass effect
on adjacent mesenteric vessels [8]. Mass effect
is not a feature of MP, and in such cases, imaging-guided percutaneous biopsy or laparoscopy and biopsy should be considered.
Imaging Findings in Retractile
Mesenteritis
Retractile mesenteritis represents the more
chronic and fulminant subgroup of sclerosing
mesenteritis [4]. Its imaging characteristics differ greatly from those of the MP subgroup and
are typified by the presence of one or more irregular fibrotic soft-tissue mesenteric masses
(Fig. 8). Calcification may be seen within the
soft-tissue mass, most likely reflecting a sequela
of fat necrosis, and there may be encasement
of the adjacent bowel loops and vascular structures, leading to signs of obstruction and occasionally to hollow visceral ischemia [13, 22].
on CT, but the primary carcinoid tumor, most
commonly involving the ileum, may not be
detectable on CT. Small-bowel investigations
such as CT enterography, CT enteroclysis, or
double-balloon and capsule endoscopy are frequently required to detect the small primary tumors [3]. Desmoid tumors constitute a benign
proliferation of fibrous tissue and are seen in
association with familial colorectal polyposis,
otherwise known as Gardner syndrome, most
commonly after laparotomy or in the postpartum patient [2]. Most mesenteric desmoid tumors are isoattenuating relative to muscle.
Mesenteric vessels are usually displaced but
not encased by the mass [2].
When retractile mesenteritis involves the
omentum or peripancreatic region, it may
simulate widespread carcinomatosis; infection; or, rarely, pancreatic malignancy [23].
Conclusion
Radiologists should be aware that sclerosing
mesenteritis has two imaging phenotypes—
namely, MP and retractile mesenteritis. MP results in a segmental increase in mesenteric fat
density termed the “misty mesentery”; however, this imaging finding is nonspecific and MP
cannot be diagnosed on CT without the exclusion of a range of important differential diagnoses that can mimic MP on imaging studies,
including causes of mesenteric edema, lymphedema, hemorrhage, or infiltration. Retractile
mesenteritis results in irregular fibrotic mesenteric masses and therefore simulates neoplastic conditions of the mesentery and peritoneum
such as carcinoid tumors, desmoid tumors, and
peritoneal carcinomatosis.
References
Mimics of Retractile Mesenteritis
The imaging features of retractile mesenteritis overlap with numerous malignant conditions
of the mesentery and peritoneum such as carcinoid tumors, desmoid tumors, and peritoneal
carcinomatosis [2]. Because of the overlapping
imaging findings in these conditions, retractile
mesenteritis is also a diagnosis of exclusion and
typically requires extensive histologic sampling
and often resection to exclude neoplasia [3].
Gastrointestinal carcinoid tumors typically appear as a solid mass located in the mesentery with imaging features of a surrounding
desmoplastic reaction resulting in stellate linear stranding of the adjacent mesenteric tissues
[2] (Fig. 9). Calcifications are visible in up to
70% of these lesions and they are often indistinguishable from retractile mesenteritis on CT.
The mesenteric mass is often easily identified
W118
1.Mindelzun RE, Jeffrey RB Jr, Lane MJ, Silverman PM. The misty mesentery on CT: differential
diagnosis. AJR 1996; 167:61–65
2.Filippone A, Cianci R, Di Fabio F, Storto ML.
Misty mesentery: a pictorial review of multidetector-row CT findings. Radiol Med 2011; 116:351–365
3.Horton KM, Lawler LP, Fishman EK. CT findings
in sclerosing mesenteritis (panniculitis): spectrum
of disease. RadioGraphics 2003; 23:1561–1567
4.Emory TS, Monihan JM, Carr NJ, Sobin LH.
Sclerosing mesenteritis, mesenteric panniculitis
and mesenteric lipodystrophy: a single entity? Am
J Surg Pathol 1997; 21:392–398
5.Vlachos K, Archontovasilis F, Falidas E, Mathioulakis S, Konstandoudakis S, Villias C. Sclerosing
mesenteritis: diverse clinical presentations and
dissimilar treatment options—a case series and
review of the literature. Int Arch Med 2011; 4:17
6.Daskalogiannaki M, Voloudaki A, Prassopoulos
P, et al. CT evaluation of mesenteric panniculitis:
prevalence and associated diseases. AJR 2000;
174:427–431
7.Kipfer RE, Moertel CG, Dahlin DC. Mesenteric
lipodystrophy. Ann Intern Med 1974; 80:582–588
8.
van Breda Vriesman AC, Schuttevaer HM,
Coerkamp EG, Puylaert JB. Mesenteric panniculitis: US and CT features. Eur Radiol 2004;
14:2242–2248
9.Sampert C, Lowichik A, Rollins M, Inman C,
Bohnsack J, Pohl JF. Sclerosing mesenteritis in a
child with celiac disease. J Pediatr Gastroenterol
Nutr 2011; 53:688–690
10.Akram S, Pardi DS, Schaffner JA, Smyrk TC. Sclerosing mesenteritis: clinical features, treatment, and
outcome in ninety-two patients. Clin Gastroenterol
Hepatol 2007; 5:589–596; quiz, 523–524
11.Catalano O, Cusati B. Sonographic detection of
mesenteric panniculitis: case report and literature
review. J Clin Ultrasound 1997; 25:141–144
12.Kakitsubata Y, Umemura Y, Kakitsubata S, et al.
CT and MRI manifestations of intraabdominal
panniculitis. J Clin Imaging 1993; 17:186–188
13.Sabate J, Torrubia S, Maideu J. Sclerosing mesenteritis: imaging findings in 17 patients. AJR 1999;
172:625–629
14.Seo BK, Ha HK, Kim AY, et al. Segmental misty
mesentery: analysis of CT features and primary
causes. Radiology 2003; 226:86–94
15.Yenarkarn P, Thoeni RF, Hanks D. Case 107:
lymphoma of the mesentery. Radiology 2007;
242:628–631
16.Zissin R, Metser U, Hain D, Even-Sapir E. Mesenteric panniculitis in oncologic patients: PET-CT
findings. Br J Radiol 2006; 79:37–43
17.Chopra S, Dodd GD, Chintapalli KN, Esola CC,
Ghiatas AA. Mesenteric, omental, and retroperitoneal edema in cirrhosis: frequency and spectrum
of CT findings. Radiology 1999; 211:737–742
18.Akhan O, Pringot J. Imaging of abdominal
tuberculosis. Eur Radiol 2002; 12:312–323
19.Waldmann TA, Steinfeld JL, Dutcher TF, Davidson J, Gordon R Jr. The role of the gastrointestinal
system in “idiopathic hypoproteinemia.” Gastroenterology 1961; 41:197–207
20.Simpson AJ, Amer H. The radiology corner: segmental lymphangiectasia of the small bowel. Am J
Gastroenterol 1979; 72:95–100
21.Horton KM, Corl FM, Fishman EK. CT of nonneoplastic diseases of the small bowel: spectrum of
disease. J Comput Assist Tomogr 1999; 23:417–428
22.Hassan T, Balsitis M, Rawlings D, Shah AA. Sclerosing mesenteritis presenting with complete
small bowel obstruction, abdominal mass and hydronephrosis. Ir J Med Sci 2012; 181:393–395
23. Scudiere JR, Shi C, Hruban RH, et al. Sclerosing mesenteritis involving the pancreas: a mimicker of pancreatic cancer. Am J Surg Pathol 2010; 34:447–453
AJR:200, February 2013
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
Mesenteric Panniculitis and Its Mimics
A
B
Fig. 1—47-year-old man with masslike region of heterogeneously increased fat attenuation consistent with mesenteric panniculitis.
A and B, Axial contrast-enhanced CT images show fatty mass (arrow) displacing local bowel loops but not displacing surrounding mesenteric vascular structures.
Bilateral extra renal pelves are also incidentally shown.
A
B
C
D
Fig. 2—75-year-old man with mesenteric panniculitis.
A and B, Axial contrast-enhanced CT images show involvement of jejunal mesentery (arrow) that initially is located on left side of abdomen.
C and D, Axial contrast-enhanced CT images acquired at later date show involvement of jejunal mesentery (arrow) persists but has moved in interim to right side of abdomen.
AJR:200, February 2013W119
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
McLaughlin et al.
A
B
Fig. 3—60-year-old man with mesenteric panniculitis.
A and B, Axial contrast-enhanced CT images show peripheral curvilinear band of soft-tissue attenuation (arrows), limiting heterogeneous mesenteric mass from
surrounding normal mesentery. This finding is referred to as “tumoral pseudocapsule” sign.
Fig. 4—63-year-old man with mesenteric
panniculitis. Axial contrast-enhanced CT image
shows preservation of normal fat density in tissues
surrounding mesenteric vessels (arrows), thereby
creating “fat halo” sign.
A
B
Fig. 5—58-year-old man with acute superior mesenteric venous thrombosis.
A and B, Axial CT images show filling defect (arrow, A) in superior mesenteric vein with associated regional increase in mesenteric fat density as result of edema. There
also is moderate volume of ascites (arrowheads).
W120
AJR:200, February 2013
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
Mesenteric Panniculitis and Its Mimics
A
B
Fig. 6—Mesenteric inflammation as mimic of mesenteric panniculitis (MP).
A and B, Axial (A) and coronal (B) contrast-enhanced CT images of 43-year-old
man with acute pancreatitis show local increase in mesenteric fat density and
mild adenopathy (arrow, A) secondary to inflammation. Pancreas appears normal
on CT but presence of ascites (arrowheads, B) and retroperitoneal fluid is strongly
suggestive of diagnosis other than MP.
C, Axial contrast-enhanced CT image of 28-year-old woman with acute appendicitis
(arrow) shows local increase in mesenteric fat density secondary to inflammation.
C
AJR:200, February 2013W121
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
McLaughlin et al.
A
B
C
D
Fig. 7—78-year-old man with non-Hodgkin lymphoma.
A and B, Axial (A) and coronal (B) contrast-enhanced CT images acquired at initial diagnosis show multiple pathologically enlarged mesenteric lymph nodes (arrow).
C and D, Axial (C) and coronal (D) contrast-enhanced CT images acquired after successful treatment with chemotherapy show previously enlarged mesenteric
lymph nodes are now smaller; however, residual heterogeneously increased mesenteric fat attenuation (arrowhead) after therapy mimics appearance of mesenteric
panniculitis.
W122
AJR:200, February 2013
Downloaded from www.ajronline.org by 198.108.143.18 on 08/15/14 from IP address 198.108.143.18. Copyright ARRS. For personal use only; all rights reserved
Mesenteric Panniculitis and Its Mimics
A
B
Fig. 8—43-year-old woman with retractile mesenteritis.
A, Axial contrast-enhanced CT image shows irregular, poorly circumscribed mesenteric soft-tissue mass (arrow), which is inseparable from terminal ileum, and punctate
foci of calcification likely representing internal fat necrosis.
B, Coronal contrast-enhanced CT image shows irregular, poorly circumscribed mesenteric soft-tissue mass (arrow).
A
B
Fig. 9—58-year-old man with carcinoid tumor of distal ileum.
A, Axial contrast-enhanced CT image shows solid mesenteric mass with internal calcification (arrow) closely resembling appearance of retractile mesenteritis.
B, Coronal contrast-enhanced CT image shows solid mesenteric mass (arrow) closely resembling appearance of retractile mesenteritis.
AJR:200, February 2013W123
![Paper_Prof_Wang_final1[1]](http://s3.studylib.net/store/data/005836194_1-85fb8d8882c087decd1a6d9c9fdc99c0-300x300.png)