GYN Update Family Medicine Refresher Course Jennifer McCaul
advertisement

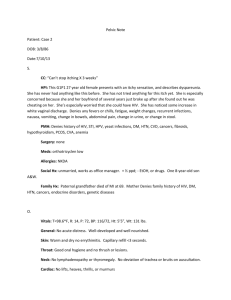
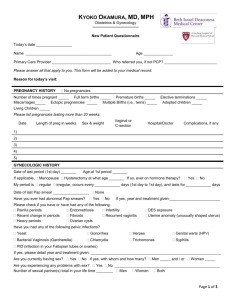
GYN Update Family Medicine Refresher Course Jennifer McCaul, MD February 7, 2014 If you think you are confused you should try being our patients…… — Dispel confusion regarding the “new” guidelines for : — Screening pap smears (out since 2012) — Yet, many of our colleagues are neither aware of nor following. — Management and follow-up of abnormal pap smears (released in 2013) — Provide talking points to help dispel your patients’ confusion regarding these guidelines — Review and walk through case studies that apply to your patients — Give some easy algorithms for office staff to follow — Technology Updates — It is unusual to see consensus from so many organizations in a guideline From 2009 to 2011 a steering group from the ASCCP, ACS and ASCP met to develop 6 working groups to review evidence and release new guidelines § The working groups included members from the above organizations and many others § Working groups reviewed evidence in studies from 1995-2011 • Topic s included: § • • • • • • Intervals Women 30+ HPV vaccine HPV testing without pap When to stop screening What to do when HPV/cytology are discordant — New understanding of the natural history course of HPV disease — Evidence of the side effects of overzealous management of precursor lesions — Efforts to individualize screening and management to age, risk factors and history When it comes to cervical cancer screening, one size does not fit all • For years we have made the well woman exam and pelvic exam synonymous with the pap smear- It is time to educate patients to the contrary — The Pelvic Exam-In 3 Parts — External Inspection — Speculum exam of Vagina/Cervix — Bimanual exam of vagina/uterus/cervix/adnexa — External Exam– Should not be skipped in the young patient-HSV/HPV/ Abuse – Could be offered to the older woman who no longer needs a pap but can not see her own perineumatrophy, lichen sclerosus — Internal/Speculum Internal exam not needed to prescribe OCPs o Adolescents can be screened for STIs with Urine nucleic acid amplification o If pap smear is not indicated, that does not mean the visit is not. o — Rarely indicated under age 21 unless acute complaint — Bimanual exam has questionable sensitivity and value but may be helpful — Indications include: ◦ ◦ ◦ ◦ ◦ ◦ Menstrual disorder Discharge Infertility Pelvic pain Perimenopausal with AUB Changes in bowel or bladder function ◦ Vaginal bulging/prolapse CDC.gov — Due to the slow progression of cervical disease, being rarely or never screened is the most important risk factor for development of cancer. — CDC populations studies find that those most likely to be rarely or never screened are: Lower SES — Minorities — Foreign born — No primary health care provider — Practical application of the guidelines For the purposes of this lecture: Cytology and Pap smear are interchangeable terms. HPV positive means High Risk HPV positive because we should NEVER be testing for low risk anyway , right???? Sidenote: An assumption made in the development of the guidelines is that conventional pap smears and liquid based preparations perform similarly — NEVER before age 21 (D) — USUALLY not after 65 (D) (see below) — 21-65 Cytology every 3 years (A) — OR: 30-65 with nl testing — Co-test with HPV/cytology every 5 years if both negative.(A) — <30 never screen w HPV (D) — HPV type only if ASCUS — NOT after Hysterectomy if no history of CIN2,CIN3 or cervical cancer — Screening more often than every 3 years was found to give little additional benefit but resulted in large increases in harm (in any patient group) — Harms considered were: — — — — — Anxiety Stigma of STI Pain and bleeding from Pap procedure Pregnancy complications LEEP- can have side effects of — Increased preterm birth (OR 1.7) — Increased LBW (OR 1.8) — Increased PPROM (OR 2.7) — Risk increases with depth and number of LEEPs — Why the increase in intervals….? — An Example: Lifetime risk of Colposcopy — Screening every 3 years — 760 colpos/1000 women — Screening every 2 years — 1080 colpos/1000 women — Screening every 1 year — 2000 colpos/1000 women….. — That is 2 colpos in the average woman’s lifetime…… — O Joy! — If s/p hysterectomy for cervical malignancy or has history of CIN2, CIN3 or cervical cancer, the patient should be screened for 20 years after definitive treatment (BUT no more often than on schedule appropriate to their age) even if it extends the period of testing beyond 65 years of age. — Patients with DES exposure, HIV+ or immunocompromise need more aggressive or longer screening due to increased risk. — — — — — — — Early onset of sexual activity does not change screening recommendations HPV vaccination does not change screening recommendations Contraceptive use does not change screening recommendations Pregnancy does not change screening recommendations (but may affect management) Fibroids and ovarian cysts do not affect screening recommendations New sexual partners later in life do not affect screening recommendations Hormone replacement therapy does not affect screening recommendations — Why are we not doing routine HPV testing in 21-29 yo? Because prevalence of HPV is up to 20% — The incidence of cervical cancer is <5/100,000 — Most infections are cleared spontaneously — — Why are we cotesting q5y in women 30-64 yo? Can achieve detection of CIN3 equal to cytology by itself done every 1-3 yrs — Enhances detection of adenocarcinoma/AIS — Acceptable to just do cytology if resources are lacking for HPV typing — Very high negative predictive value — Why are we stopping at 65 with adequate negative screening and no hx CIN2+ in last 20 years? — And WHAT is adequate negative screening, anyway? — — 3 consecutive negative paps — 2 consecutive negative HPVs CIN2+ is rare after 65 — SO….. Your 90 year old mother should NEVER have a pap smear!!!! — http://journals.lww.com/jlgtd/PublishingImages/ASCCP%20Guide lines.pdf#zoom=80 Are not so easy to distill down and will be dealt with individually — May not fully apply to you if you send your patients out for colposcopy — — But may matter greatly when they are returned to you after colpo/biopsy/LEEP for further management — Require colposcopy less often so may result in more primary care management — AKA: The dreaded “you put your patient through the pap smear but did not get a good enough sample” — If HPV status unknown or negative then repeat cytology in 2-4 months. — If HPV positive then colpo immediately or repeat cytology in 2-4 months — Negative for — 21-29- routine screen Intraepithelial Lesion or Malignancy but no endocervical sample or transformation zone found. — Managed based on age and HPV status — >30 but negative HPV- routine screen — >30 with HPV unknown Add HPV typing (pref) — Repeat cytology 3 years — — >30 with HPV + — Repeat cytology with HPV in 1 year — Can repeat both in 1 year — If either abnl then needs colposcopy — Ok to type for HPV 16/18 If positive needs to go straight to colpo — If negative then repeat cotesting in 1 year — — HPV typing is preferred If positive then send to colposcopy — If negative then repeat cotesting in 3 years — — Repeat cytology in 1 year is acceptable If normal return to routine screening — If > asc then colposcopy — — Repeat cytology in 12 mos preferred If LSIL or less then repeat cytology 12 mos again — If negative X2 then can return to regular screening — If >LSIL then colpo — — Reflex HPV typing is acceptable for ASCUS only (NOT LSIL) If negative can resume normal screening — If positive then Colpo — — Managed based on HPV typing — — Positive HPV typing — COLPO — No HPV typing — COLPO — — At Colposcopy Negative HPV typing — Repeat cotesting at 1 year — If both negative then repeat at 3 years Endocervical sampling is recommended if not pregnant or if colpo is unsatisfactory — Colpo is preferred If <CIN2 then follow up post partum — If CIN2 or CIN3 then manage per ASCCP guidelines — — Deferring Colpo until >6 wks post partum is acceptable management NO endocervical sampling should be obtained at colposcopy during pregnancy — Management is different in that immediate LEEP is not acceptable. — Serial Colpos with cytology are indicated every 6 months over two year period. — Immediate LEEP is acceptable. — Colpo with endocervical biopsy is acceptable — Results are managed per ASCCP guidelines — Atypical Endometrial Cells Endometrial and — Endocervical sampling — — Colpo if negative — All other subcategories Colposcopy for all — AND Endometrial Sampling — — If >35 or at risk for endometrial neoplasia http://www.asccp.org/Portals/9/docs/Algorithms%207.30.13.pdf How do I use all this to treat my patients? — My patient Mary Blair, age 35 who is co-screened with pap and HPV per guidelines — Pap normal with positive high risk HPV — What would you do? — Repeat both at 12 mos — Colpo if either is still positive Jane Black is 38 and screened with pap only • Pap shows ASCUS • What would you do? • HPV typing • If Negative • Repeat cytology 12 mos • If Positive • Colposcopy • Repeat cytology 1 yr acceptable — LSIL and ASCUS are — The younger patient 22 year old female has ASCUS on her first pap, and on discussion she reveals her sister who is 24, just had a LSIL papWhy do you manage them the same? managed the same in 2124 yo women- HOW? — Repeat Cytologypreferred — Negative/LSIL/ASC-US — Repeat cytology 12 mos — ASC-H, HSIL, AGC — Colpo — Could also reflex to HPV for ASCUS ONLY — Negative returns to routine screening HPV negative — Colposcopy — — If ASC or greater then — IF HPV is Positive— At Colposcopy— Endocervical sampling if not pregnant and no lesion identified on colpo. Preferred to repeat cotesting in 1yrColpo — Acceptable to do colpo — What if their 38 yo Aunt was LSIL and was Pregnant? — Colposcopy preferred but acceptable to defer until postpartum — If colpo is chosen: NO endocervical sampling at time of colpo — If CIN 1 or less — Postpartum f/u — If CIN2 or CIN3 — Manage per guidelines You get a pap back that shows negative cytology but mentions there is not sufficient endocervical or transformation zone cells…….What do you need to know? Age and HPV status — 21-29 yo-----Who cares? Routine screening — >30 – HPV neg-----Routine screening — >30- HPV pos----cyto and HPV in 1 yr — >30-HPV unknown---— HPV testing (preferred), then follow above — Repeat cytology in 3 years (acceptable) “Excuse me, I seem to have misplaced my transformation zone, have you seen it anywhere?” — You bring in June White, your 54 year old super morbidly obese patient for her screening pap and HPV typing. It takes 3 people to help do the exam and you are still not entirely sure you got the cervix. — Pap shows UNSATISFACTORY SAMPLE What should you do? — Find out HPV status — HPV- Positive-----Colpo or repeat in 2-4 mos — HPV-Negative-----Repeat pap 2-4 mos — HPV- unknown-----Repeat pap 2-4 mos — If your repeat cyto is negative and HPV- then return to routine screening — IF your repeat is cyto is negative and HPV+ then repeat cotesting in 1 year — Pap shows AGC, so now what do you want to know? — Specific type — If Atypical endometrial cells — Endometrial and endocervical sampling — IF any other glandular atypia — Colpo and endometrial sampling with endocervical sampling — Safe bet is to refer these to colpo management if you are not doing your own colpos. — Pap shows ASC-H- So Now what? — Colpo — Colpo — Colpo — Regardless of HPV status — Management of colpo results per ASCCP guidelines What would you do differently? — COLPO is still the next step But undesireable to LEEP — Can do cyto with colpo q6 mos for 2 years — — IF HSIL persists for 24 mos- excision needed — If 2 consecutive neg cyto and nothing on colpo — Can return to routine — If HSIL persists for 12 mos can bx and treat per guidelines if CIN 2, CIN3 For a straightforward handout that will help you explain the new guidelines to your patients use this link: — http://www.acog.org/~/m edia/For%20Patients/pfs 004.pdf — For an even simpler patient explanation of when paps are indicated you can use this handout: — http://www.choosingwi sely.org/doctor-patientlists/pap-tests/ Feel free to print and distribute this algorithm for use with office staff or for quick reference — ASCCP app is available for iphone, ipad and Android — $9.99 — Can easily calculate individual patient based recommendations — Easy view of all guidelines Cytology for those who do not colpo — Histology for those who do colpo themselves — — www.cdc.gov — www.asccp.org — www.acog.org — www.choosingwisely.org — Burd, EM. Clin Microbiol rev 2005: 16 1-17. — Kulasingam S et al. 2011. AHRQ publication no. 11-05157-ef-1. — Massad, L. Journal of Lower Genital Tract Disease, vol 17, number 5, 2013. — Saslow, D. Journal of Lower Genital Tract Disease, vol 16 number 3, 2012. — Stout, NK. Arch Inter Med 2008: 168-181.