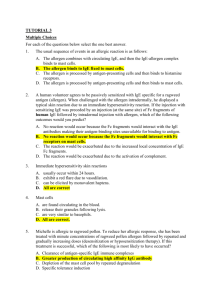
IMMUNE EFFECTOR MECHANISMS
advertisement

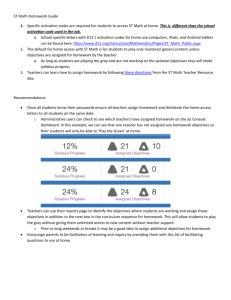
IMMUNE EFFECTOR MECHANISMS Antibody-Mediated Reactions Immunology - the Double-Edged Sword Immunoprotection Immunopathology Both involve the same immune mechanisms! The balancing act between hyporeactivity and hyperreactivity Infections and Tumors Health Immunopathology Classification of Immune Mechanisms Handout Gell and General Properties Coombs (1963) Antibody-Mediated Inactivation or Activation Cytotoxic or Cytolytic Immune Complex Atopic or Anaphylactic -Type II Type III Type I Toxin, virus inactivation Opsonization, ADCC, C’-mediated lysis Ag-Ab complex formation in tissue IgE mediated allergic reactions Cell-Mediated T-cell Cytotoxic Delayed Hypersensitivity -Type IV CD8+ T cell-mediated cell lysis CD4+ T cell-mediated activation of macrophages Either Granulomatous Reactions -- Chronic reaction to poorly degradable antigens Lecture: Ab mediated Reactions 1 2 3 4 6 5 Granulomatous Persistent antigen Lymphocytes and Macrophages Space occupying lesion Lecture: Cell mediated Reactions 7 Induction of Different Forms of Immunity • • • • Type of agent or antigen. Route of infection/exposure. Activation of Th1 vs. Th2 cells. Location/cell type involved in antigen presentation. • Cytokines expressed by antigen presenting cells and T cells. • Genetic factors. • Non-genetic factors. (e.g. age and nutritional status) 1. Inactivation or Neutralization Reactions Definition - binding of antibody to an epitope resulting in inactivation, neutralization or abnormal activation Mechanisms – Ab binding to a protein (e.g. toxin) can inhibit binding to substrate or alter conformation, resulting in loss of activity Ab binding to virus can block receptors, alter viral structure, or opsonize virus Autoimmune Abs against hormone or neurotransmitter receptors can either block or activate the receptor Toxin Viral protein Host protein Direct Blockade of active site; or Alteration of structure, function Inactivation or Neutralization Reactions: Medical Aspects (Examples) • Protective • Toxin inactivation (e.g. C. diphtheriae and C. tetani toxins) • Virus neutralization (polio, influenza, measles, mumps, rubella) • Immunopathologic • Myasthenia gravis: autoimmune Ab to ACh receptors, blocks interaction • Graves disease: Ab to TSH receptor activate thyroid cells (hyperthyroidism) Clinical Vignettes – Inactivation Reactions (Geha and Notarangelo, “Case Studies in Immunology”) Case 40 Myasthenia Gravis binding of anti-AchR antibodies results in skeletal muscle weakness (blocks activation) Three effects Anti-AchR antibodies block Ach binding Ach receptors internalized and degraded Synaptic clefts decrease in complexity • Aristotle Onassis • (Jackie Kennedy Onassis’ husband) had this disease. Graves Disease: Autoantibody to cell surface receptors leading to activation reaction Normal thyroid activation Autoantibody activation Graves Disease: Autoimmunity to cell surface receptors Opthamolopathy Factoid: George and Barbara Bush AND their dog Millie all had Graves disease while he was President. 2. Cytotoxic Reactions (Type II Hypersensitivity) Definition - Ab binding to cell surfaces resulting in opsonization, complement activation, or ADCC Mechanisms Activation of classical complement pathway, MAC formation Opsonization by IgG or C3b, enhanced phagocytosis Antibody-Dependent Cellular Cytotoxicity (ADCC) involving null lymphocytes or macrophages (IgE mediated binding of eosinophils to helminths) (complement dependent examples) Cytotoxic Reactions: Medical Aspects (Examples)) Protective Ab and complement-mediated killing and opsonization of pyogenic bacteria (e.g. Staph and Strep) – Ab and complement-mediated killing and opsonization of protozoa, including Plasmodium and Trypanosoma – ADCC against virus-infected cells, tumor cells, protozoa, and helminths – Immunopathologic Transfusion reactions - lysis of transfused RBCs – Rh reactions - hemolytic disease of newborns – Hemolytic anemia- autoantibodies lyse, opsonize RBCs – Goodpasture's syndrome - anti-basement membrane Abs – Transplant rejection - recipient Abs cause hyperacute rejection – Immunopathologic – Transfusion reactions - lysis of transfused RBCs – Rh reactions - hemolytic disease of newborns – Hemolytic anemiaautoantibodies lyse, opsonize RBCs – Transplant rejection recipient Abs cause hyperacute rejection Blood Groups Hemolytic anemia- autoantibodies lyse, opsonize RBCs Case 46. Geha and Notarangelo Infections can cause individuals to develop transient serum antibodies to RBC antigens. Hyperacute Rejection – Kidney Preformed antibodies available to rapidly destroy transplanted tissue 3. Immune Complex Reactions (Type III Hypersensitivity) Definition - deposition of AgAb complexes, leading to attraction of PMNs, inflammation Mechanisms – Soluble or insoluble (large) complexes form between Ag and IgG or IgM and are deposited in tissue – Immune complexes fix complement (releasing C3a, C5a), resulting in mast cell degranulation and attraction of neutrophils – Inflammatory response can aid in clearing bacteria – Complement activation, release of neutrophil lysosomal contents can cause tissue damage Occurring in Tissue and influx of PMNs, monocytes • hemorrhagic appearance (purpura) • Neutrophilic infiltrate around vascular beds • Requires 2 to 6 hours to occur Immune Complex Reactions: Medical Aspects (Examples) Protective – Contribute to acute inflammatory responses, protection against bacterial infections Immunopathologic – Serum sickness (‘foreign’ protein or drug-induced) – Systemic lupus erythematosus (SLE) and other autoimmune diseases – Rheumatic fever – Glomerulonephritis - neutrophil infiltration, 'lumpybumpy' basement membrane deposits (Geha and Notarangelo, “Case Studies in Immunology”) Case 52 Drug-Induced Serum Sickness – antibodies against penicillin cause vasculitis, hemorrhage Case 37 - Systemic Lupus Erythematosus 16 yo Nicole Chawner developed a ‘butterfly’ rash over her cheeks after prolonged exposure to the sun. Also experienced joint pain and had enlarged lymph nodes. She had anti-DNA antibodies and decreased complement C3 levels. Treatment: prednisone and naproxen. Geha and Notarangelo, Case Studies in Immunology 4. Anaphylactic or Atopic Reactions (Type I Hypersensitivity) Definition - IgE-mediated activation of mast cells and other cell types and its effects. Mechanisms – IgE is produced and binds to Fc receptors on mast cells, basophils, and eosinophils – Ag crosslinking of bound IgE results in mast cell degranulation and synthesis of leukotrienes & prostaglandins – Histamine release causes increased vascular permeability, vasodilation, and bronchoconstriction – ECF-A and NCF attract eosinophils, neutrophils – Leukotrienes and eosinophil factors cause long-term effects Anaphylactic or Atopic Reactions: Medical Aspects (Examples) Protective – Helminth infections: expulsion of worms from GI tract, eosinophil-mediated killing of worms in tissues Immunopathologic – Hay fever – Asthma – Cutaneous anaphylaxis – Food allergies – Systemic anaphylaxis Mast Cells Connective Tissue (Skin) Mucosal (Gut) http://tu-dresden.de/die_tu_dresden/fakultaeten/medizinische_fakultaet/inst/imm/bilder/mast_cells http://www.vetmed.vt.edu/education/curriculum/vm8054/Labs/Lab5/Lab5.htm Mast cells – found in tissue (EM, color enhanced) Basophils – found in blood Protective Response to Parasitic Worms Problem – IgE made in response to “everyday” antigenic stimuli. These stimuli thus become “allergens”. Sequence of Events Sensitization Phase – Individual exposed to antigen. – B cells produce IgE to allergen. – Activation Phase – Mast Cells (and Basophils ) recognize Ab-Ag and trigger activation of cell. Mast cell triggered to release granules and inflammatory mediators. – Usually due to cross-linking of Fc receptors with antigen. – Effector Phase – Preformed mediators released. – Newly synthesized mediators made and released. – Late Phase – Continued tissue damage. – Sensitization Phase IgE-Mediated Reactions Effector Phase with released mediators Clinical Presentations of Type I Hypersensitive Reactions Anaphylactic Reaction to a Bee Sting Roitt 19.2 Clinical Vignettes – Anaphylactic Reactions (Geha and Rosen, “Case Studies in Immunology”) Case 50 Allergic Asthma –14 yo Frank Morgan has rhinitis and persistent wheezing Case 49 Acute Systemic Anaphylaxis – toddler John Mason has a near-fatal allergic reaction after repeated exposure to cookies containing peanut butter Lecture: Ab mediated Rxns 1 2 3 4 6 5 Granulomatous Persistent antigen Lymphocytes and Macrophages Space occupying lesion Lecture: Cell mediated Rxns 7 Late Phase Reaction with released mediators (constant stimulation leads to pathology; occurs in ASTHMA)