Gluconeogenesis

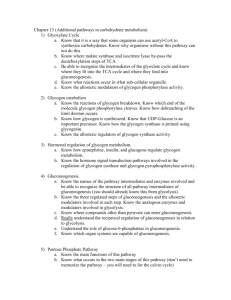
GOALS FOR LECTURE 10:
Describe the biological purpose of gluconeogenesis. Summarize the physiological states where gluconeogenesis would occur.
Identify the biochemical reactions that are identical between glycolysis and gluconeogenesis, and those that are distinct. Rationalize why the distinct reactions must be different between the two pathways.
Describe the involvement of the mitochondria and the endoplasmic reticulum in gluconeogenesis.
Describe the allosteric effectors that regulate key enzymes in gluconeogenesis. Contrast the allosteric regulation of gluconeogenesis with the allosteric regulation of enzymes in glycolysis. Rationalize the roles of these effectors based on cellular energy needs.
Recommended reading:
TOPIC
Gluconeogenesis
STRYER, 4th edition DEVLIN, 5th edition
Ch. 16, 450-460 Ch. 14, 629-643
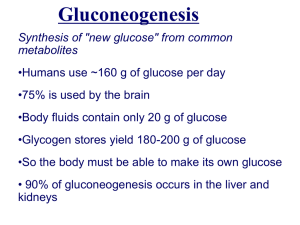
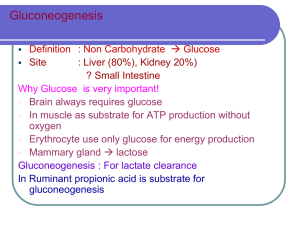
Gluconeogenesis
The energy requirement of the brain is derived almost entirely from glucose. Since nerve cells store very little glycogen, the brain and certain other tissues including cornea and red blood cells depend on a constant supply of glucose in the blood. One of the important functions of the liver is to maintain the blood glucose level. Degradation of liver glycogen is the primary source of blood glucose in the early fasting state. However, when glycogen stores are depleted, the liver is able to synthesize glucose from lactate, via gluconeogenesis. In the Cori cycle, depicted below, gluconeogenesis in the liver supports anaerobic glycolysis in red blood cells.
10.1
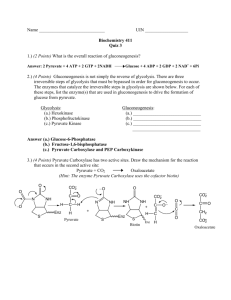
Gluconeogenesis uses many of the same reactions as glycolysis, but running in reverse. Among the glycolytic reactions, recall that all are readily reversed with the exception of the reactions catalyzed by hexokinase/glucokinase, phosphofructokinase, and pyruvate kinase. Previously, we have seen that these reactions are regulated. In gluconeogenesis, they are bypassed.
Pyruvate kinase is bypassed in two steps
Conversion of pyruvate to phosphoenolpyruvate occurs by a combination of two reactions, and requires hydrolysis of two ATP to ADP. In the first reaction, pyruvate is converted to oxaloacetate by pyruvate carboxlyase, which uses biotin as a cofactor.
This reaction takes place in the mitochondrial matrix and is also used to generate oxaloacetate as an intermediate in the TCA cycle, as will be discussed later. This reaction depends on an ATP-dependent carboxylation of biotin.
10.2
To be used for gluconeogenesis, the oxaloacetate must be transferred back into the cytoplasm. However, mitochondria lack an efficient transporter for oxaloacetate. Therefore, oxaloacetate is reduced to malate, by malate dehydrogenase which converts one molecule of NADH to NAD + . Malate is then transported out and reoxidized to oxaloacetate, regenerating NADH from NAD + in the cytoplasm.
Phosphoenolpyruvate carboxykinase simultaneously decarboxylates and phosphorylates oxaloacetate to generate phosphoenolpyruvate. GTP is used as the phosphoryl donor. Decarboxylation drives this reaction, which would otherwise be endergonic.
10.3
Glucokinase and phosphofructokinase are bypassed by phosphatases
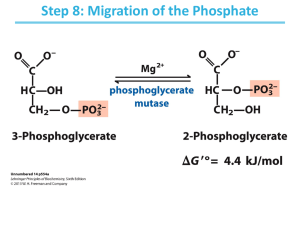
Phosphoenolpyruvate is converted to fructose-1,6-bisphosphate by a simple reversal of glycolytic steps 9, 8, 7, 6, 5 and 4, which all operate near equilibrium. Fructose-
1, 6-bisphosphate is dephosphorylated by fructose-1,6-bisphosphatase, releasing free phosphate, and bypassing phosphofructokinase. Fructose-6-phosphate is converted to glucose-6-phosphate by a phosphoglucose isomerase. Glucose-6-phosphate is converted to glucose by glucose-6-phosphatase, bypassing glucokinase.
Glucose-6-phosphatase is found in the lumen of the endoplasmic reticulum rather than in the cytoplasm. Thus, for the final step of gluconeogenesis, G6P must be transported into the ER, the phosphate is cleaved off, and then glucose and phosphate are transported back out. Deficiencies in either glucose-6-phosphatase or any of the three transporters result in von Gierke’s disease, with symptoms of hypoglycemia, lacticacidemia and ketoacidosis after mild fasting.
Note that these two phosphatase reactions do not reverse the reciprocal kinase reactions, because ATP is not regenerated.
The stoichiometry for gluconeogenesis from pyruvate is:
2 pyruvate + 4 ATP + 2 GTP + 2 NADH + 6 H
2
O Õ glucose + 4 ADP + 2 GDP + 6 P i
+ 2 NAD + + 2 H +
By contrast, the stoichiometry for conversion of glucose to pyruvate by glycolysis is: glucose + 2 ADP + 2 P i
+ 2NAD + Õ 2 pyruvate + 2 ATP + 2 NADH + 2 H
2
O
In cycling from glucose to pyruvate to glucose in the Cori cycle, four high-energy phosphate bonds are hydrolyzed. This expenditure of energy is required to turn an energetically unfaovable process (the reversal of glycolysis,
∆
G o ’ = +20 kcal/mol) into a favorable one (gluconeogenesis,
∆
G o ’ = -9 kcal/mol). The extra cost of nucleotide hydrolysis is borne by the liver, another example of its altruism toward other tissues.
10.4
Summary of gluconeogenesis, contrasted with glycolysis
10.5
Alternate substrates for gluconeogenesis
Any precursor which can be converted to pyruvate can ultimately be converted to glucose by gluconeogenesis. These precursors include all amino acids except for leucine and lysine and propionate.
Ethanol consumption and gluconeogenesis
Ethanol is metabolized primarily in the liver, by alcohol dehydrogenase.
CH
3
CH
2
OH + NAD + CH
3
CHO + NADH + H +
This reaction elevates the ratio between NADH and NAD + in liver cytosol. High
NADH levels block the conversion of cytoplasmic malate to oxaloacetate, preventing gluconeogenesis. Similarly, glyceraldehyde-3-phosphate dehydrogenase is forced to run backward by high [NADH], so glycolysis is also inhibited. Conversion of lactate to pyruvate by lactate dehydrogenase is also inhibited by high [NADH]. Consequently, consumption of large amounts of ethanol can result in hypoglycemia and mild lactic acidosis.
Severe hypoglycemia can cause irreversible damage to the central nervous system, which in its early stages might be mistaken for simple intoxication.
10.6
Regulation of gluconeogenesis
The enzymes of glycolysis and gluconeogenesis in the liver are reciprocally regulated so that either glucose is converted to pyruvate or pyruvate is converted to glucose. Fructose-2,6-bisphosphate, which we have already seen serves to activate phosphofructokinase, is an inhibitor of fructose-1,6-bisphosphatase. Because of this reciprocal effect, only one of the two enzymes is active at any given time.
The liver also contains glucokinase inhibitor protein, which is activated by fructose-6phosphate. When bound to F6P, glucokinase inhibitor protein sequesters and inactivates glucokinase, shutting down the first step in glycolysis. There is no equivalent inhibitory protein for hexokinase, so accumulation of F6P shuts down glycolysis and enables activation of gluconeogenesis only in the liver. Allosteric regulation of gluconeogenesis and glycolysis is summarized below:
10.7
Hormonal control of gluconeogenesis
As with glycolysis, glucagon-dependent protein phosphorylation also regulates enzyme activities in gluconeogenesis. Recall that F-2,6-BP levels are regulated by glucagon, with high glucagon (low blood sugar) favoring conversion of F-2,6-BP back into
F6P
In addition, glucagon activates lipases is adipose tissue, promoting release of fatty acids into the bloodstream. These fatty acids are broken down in the mitochondria of liver, resulting in high concentrations of acetyl CoA. Acetyl CoA acts as an allosteric activator of pyruvate carboxylase.
Both insulin and glucagon regulate the transcription of bypass enzymes: insulin inhibits transcription of phosphoenolpyruvate carboxykinase, and glucagon activates its transcription.
10.8