Protective Immunity to SIV Challenge Elicited by Vaccination of
advertisement

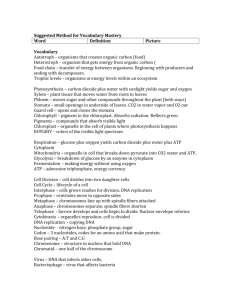
AIDS RESEARCH AND HUMAN RETROVIRUSES Volume 20, Number 4, 2004, pp. 425–434 © Mary Ann Liebert, Inc. Protective Immunity to SIV Challenge Elicited by Vaccination of Macaques with Multigenic DNA Vaccines Producing Virus-Like Particles SALLY P. MOSSMAN, 1,2,9 CHRISTOPHER C. PIERCE,1 ANDREW J. WATSON, 1 MICHAEL N. ROBERTSON,3 DAVID C. MONTEFIORI,4 LARENE KULLER,2 BARBRA A. RICHARDSON, 5 JEFFREY D. BRADSHAW, 1 ROBERT J. MUNN,6 SHIU-LOK HU,2 PHILIP D. GREENBERG,3 RAOUL E. BENVENISTE,7 and NANCY L. HAIGWOOD 1,8 ABSTRACT We utilized SIVmne infection of Macaca fascicularis to assess the efficacy of DNA vaccination alone, and as a priming agent in combination with subunit protein boosts. All SIVmne structural and regulatory genes were expressed using the human cytomegalovirus Immediate Early-1 promoter in plasmids that directed the formation of virus-like particles in vitro. Macaques (n 5 4) were immunized intradermally and intramuscularly four times over 36 weeks with 3 mg plasmid DNA. A second group (n 5 4) received two DNA priming inoculations followed by two intramuscular boosts consisting of 250 mg recombinant Env gp160 and 250 mg recombinant Gag-Pol particles in MF-59 adjuvant. These regimens elicited modest cellular immunity prior to challenge. Humoral immune responses to Env gp160 were elicited and sustained by both vaccine protocols, and as expected antibody titers were higher in the protein subunit-boosted animals. Neutralizing antibodies prior to challenge were measurable in two of four subunit-boosted macaques. The two vaccine regimens elicited comparable helper T cell responses at the time of challenge. Vaccinees and mock-immunized controls (n 5 4) were challenged intrarectally at week 38 with uncloned SIVmne. Following challenge all macaques became infected, but both vaccine regimens resulted in reduced peak virus loads (p 5 0.07) and significantly improved maintenance of peripheral CD41 T cell counts postchallenge (p 5 0.007, DNA alone and p 5 0.01, all vaccinees). There was no significant difference between the two vaccine groups in levels of plasma viremia or maintenance of CD4 1 T cell counts postchallenge. INTRODUCTION V (HIV) are needed to stem the worldwide epidemic. Despite promising results from immunizing mice with naked plasmid DNA vaccines, results in primate models have been disappointing, eliciting fully protective immune responses only to low pathogenicity challenge viruses.1,2 More recently responses induced ACCINES FOR HUMAN IMMUNODEFICIENCY VIRUS by naked DNA have been improved by the inclusion of adjuvants or cytokines3,4 or by using different methods of delivery.5,6 A number of groups have demonstrated the relative efficacy of priming responses using DNA vaccines, followed by boosting with live virus vectors.4,7–11 We were interested in comparing DNA alone with DNA plus subunit protein boosts in the SIVmne challenge model of Macaca fascicularis. Boosting with protein in an appropriate adjuvant could potentially al- 1Seattle Biomedical Research Institute, Seattle, Washington 98109. Primate Research Center, University of Washington, Seattle, Washington 98195. of Medicine, University of Washington, Seattle, Washington 98195. 4Duke University Medical Center, Durham, North Carolina 27710. 5Department of Biostatistics, University of Washington, Seattle, Washington 98195. 6Department of Pathology, University of California, Davis, California 95616. 7Laboratory of Viral Carcinogenesis, National Cancer Institute, Frederick, Maryland 21702. 8Department of Pathobiology, University of Washington, Seattle, Washington 98195. 9Current address: Corixa Corporation, Seattle, Washington 98104. 2Regional 3Department 425 426 MOSSMAN ET AL. low expansion of a CD4 and CD8 response primed by DNA. Unlike viral vectors, which are often compromised by the elicitation of antivector responses, protein has the potential for delivering multiple subsequent boosting immunizations to maintain responses over time. Primate lentivirus models for vaccine testing can have a broad range of virus loads and highly variable time to CD41 T cell decline.12,13 In the SIV mne model, the virus generally replicates to high virus loads in infected animals and leads to AIDSlike disease and CD41 T cell decline in 50–60% of macaques within 3 years postinfection. The biological clone of SIVmne, SIVmneE11S, shows reduced virus replication and slower CD41 T cell depletion relative to the parental uncloned stock.14 Priming with recombinant vaccinia viruses combined with subunit protein boosts has shown some success in providing sterilizing immunity against both intravenous and intrarectal challenge.15–17 These studies have indicated that complex multiple antigen vaccines are more effective than Envelope-only vaccines.14 Protection against intravenous challenge was observed in fewer animals than intrarectal challenge, leading to the conclusion that the mucosal barrier provides some protection, even with the very high doses of virus used to ensure full infection of all controls. The DNA vaccine described here was composed of three plasmid constructs together encoding all of the structural and regulatory genes of SIVmneE11S , without the LTRs.18 Subunit boosts consisted of Gag-Pol particles mixed with Envgp160, coformulated in MF-59 adjuvant. These antigens were produced using recombinant vaccinia virus infection of Vero cells. The choice of subunits in this experiment was governed by the desire to make direct comparisons with prior vaccinia virus priming and subunit boosting in this model. We elected to challenge the macaques with SIVmne uncloned virus stock by the intrarectal route, using the same viral stock used in prior experimental work with vaccinia prime-boost. We present evidence that both of the vaccine strategies elicited protection from SIV mne -induced CD41 T cell decline. MATERIALS AND METHODS Expression plasmids The structural and regulatory genes of SIV mneE11S , clone 8,19 were cloned into mammalian expression vectors under the control of the cytomegalovirus Immediate Early-1 promoter, as previously described.18 Three constructs were used in these experiments, pCI-env, pJW-gag-pol-env, and pcDNA3-nef. Plasmids were prepared on a large scale using Qiagen EndoFree purification kits. The DNA vaccine for macaques comprised a pool of the three vectors in equal W:W ratios in endotoxin-free saline. Animals and immunizations Twelve juvenile cynomolgous macaques (Macaca fascicularis), 1 to 2 years of age and weighing 2–4 kg, were obtained from and housed at The Washington Regional Primate Research Center. All animals were negative for SIV and simian type D retrovirus at the study onset. The DNA vaccine was administered at a dose of 3 mg DNA per animal in a volume of 1.5 ml. This dose was divided in two and given intramuscularly into the triceps and intradermally in the shoulder area. Recombinant proteins were produced using vaccinia constructs as previously described.15 Animals received a dose of 250 mg recombinant gp160 (rgp160) plus 250 mg Gag-Pol particles.14 These were coformulated in MF-59 adjuvant (Chiron Corporation) to a final volume of 1 ml per animal. The subunit boost was administered by the intramuscular route. Challenge virus SIVmne uncloned virus stock was grown in macaque PBMC and titered in vivo in M. fascicularis. Macaques were challenged with 20 macaque infectious doses (MID) by the intrarectal route. Plasma virus load determination Viral RNA in plasma was quantified using a quantitative competitive-reverse transcriptase PCR (QC-RT-PCR) assay as previously described.20 The limit of detection for this assay was 3000 copies/ml plasma. Virus isolation Cell-associated virus was detected postchallenge by coculture of peripheral blood mononuclear cells (PBMC) or lymph node (LN) cells from macaques with CEMx174 cells. Virus in supernatants from these cultures was detected by antigen capture ELISA. Cultures were maintained for 6 weeks before being discarded as negative. Nested LTR-gag PCR assay Nested set primers from the LTR/gag region of SIVmne were used to amplify proviral DNA from 2 mg total DNA extracted from PBMC or LN cells of macaques postchallenge. The first round of PCR utilized a 1 mM concentration of the following primers: 59-CCAGTGTGTGCTCCCATCTCTCCTAGTCGC and 59-GTACTTTTTCTTCCCGCCGGGTCGTAGCC. The reaction was carried out for 35 cycles, with an annealing temperature of 55°C. Of the first round reaction product 5 ml was then amplified using a 1 mM concentration of an internal set of primers: 59-CCTGACAAGACGGAGTTTCTCGCGCC and 59-CGATAATAAGAAGACCCTGGTCTG. This reaction was performed for 35 cycles with an annealing temperature of 50°C. The appropriately sized product was detected by agarose gel electrophoresis and ethidium bromide staining. Heteroduplex mobility assay PCR products were tested for heteroduplexes using standard procedures, essentially as described by Delwart et al.21 The SIV clone 8 molecular clone env gene was used as a reference sequence by which to identify sequences identical to or divergent from this clone in the V1–V2 regions. Antibody assays ELISA assays for measuring antibody titers to Envelope were performed using plates coated with rgp160 at 2 mg/ml. Bound antibodies in titrated sera were detected using goat antimonkey IgG conjugated to horseradish peroxidase (Cappel). Western blot analysis against vaccinia lysates was used to confirm that antibody reactivity detected in this ELISA was gp160 specific PROTECTION FROM SIV WITH MULTIGENIC DNA VACCINES and not due to contaminating vaccinia proteins, which may have been present in the subunit immunogens and in the protein used to coat plates. Virus neutralizing antibodies against SIVmne uncloned stock were detected in CEMx174 cells as previously described.22 T cell proliferation assay Ficoll-separated, cryopreserved PBMC were incubated in the presence of 5 mg/ml rgp160 or 10 mg/ml phytohemagglutinin in medium containing 10% heat-inactivated AB-positive human serum for 3 days at 37°C. Cells were then pulsed overnight with 0.5 mCi of aqueous [methyl-3H]thymidine. Cells were harvested the next day and counts incorporated measured on a scintillation counter. Proliferation was then expressed as the mean counts per minute of triplicate wells in antigen minus counts in medium alone (net CPM) and as a stimulation index. Cytolytic T cell assay Bulk cultures of PBMC from immunized and challenged macaques were stimulated twice in vitro with autologous adherent PBMC infected with recombinant vaccinia virus expressing Gag-Pol, Env, Nef, or LacZ, as an irrelevant control. T cells were then assayed for lytic activity against autologous B-LCL expressing SIV proteins using standard chromium release assay.23 For an assay to be significant, the specific target must be killed at least 10% and it must exceed the killing of control targets by the mean plus 3 standard deviations of three replicas for at least two different E:T ratios. Statistical analyses SPSS version 10.0 (SPSS, Inc., Chicago, IL) and S-Plus 2000 (Insightful, Inc., Seattle, WA) were used for all analyses. In all cases, values below the limit of detection of an assay were transformed to be equal to the midpoint between zero and the lower limit of detection of that assay. Differences between the experimental and control groups in median peak plasma viral load at 2 weeks postchallenge and for levels of neutralizing antibodies postchallenge were tested using the Mann–Whitney U test. Median area under the curve minus baseline values for acute levels of plasma viral RNA between weeks 0 and 6 postchallenge were calculated for vaccinees and controls as previously described.24 Values were compared for statistically sig- FIG. 1. 427 nificant differences using the Mann–Whitney U test. CD41 T cell counts were defined as ,1000 only if the CD41 T cell count at the subsequent time point was also ,1000. Differences between the experimental and control groups for time to CD41 T cell count ,1000 were assessed using Kaplan–Meier survival analysis and the log-rank test. Detection of virus-like particles in vitro pJW-gag-pol-env was cotransfected with plasmid pSV2neo expressing the neomycin resistance gene (gift of Paul Luciw, UC Davis) in COS cells using standard calcium chloride procedures. After 3 days transfected cells were selected by culturing in 400 mg/ml geneticin. Clones were expanded and examined for Gag and Env production by antigen-capture ELISA and by radioimmune precipitation assays. Positive clones were fixed in 2.5% glutaraldehyde in 0.1 M phosphate buffer and examined by electron microscopy. ELISA data estimated the yield of virus-like particles (VLPs) at 120 ng/ml culture supernatant. RESULTS Prior to inoculation into macaques, all DNA vaccine constructs used in these studies were selected for optimal expression in vitro and immunogenicity in mice, as detailed elsewhere.18 Of particular interest from these preliminary studies was the finding that the construct expressing Gag-Pol-Env was capable of producing VLPs in transfected cells in vitro. COS cells permanently transfected by the DNA construct were screened for coexpression of Gag and Env by ELISA and radioimmunoprecipitation (data not shown). The highest expressing cell line was shown to produce VLPs by electron microscopy (Fig. 1). Two groups of four cynomolgous macaques (M. fascicularis) were immunized twice with 3 mg plasmid DNA expressing multiple viral genes at weeks 0 and 8. The DNA alone group then received a further two identical immunizations at weeks 16 and 36. The second group was boosted twice with 250 mg rgp160 and 250 mg Gag-Pol particles formulated in MF-59 adjuvant. The four control animals received DNA immunizations of pCI-neo plasmid, either four times (95013 and 95027) or twice followed by two inoculations with MF-59 adjuvant alone (95042 and 95057). Electron micrograph to show virus-like particles budding from COS cells stably transfected with pJW-gag-pol-env. 428 MOSSMAN ET AL. Humoral immune responses to Env gp160 (Fig. 2) and to Gag (data not shown) were elicited by both vaccine protocols and were sustained over the course of the immunization protocol. As expected, antibody titers were higher in sera from macaques boosted with recombinant protein, where geometric mean end point titers to Env gp160 were 1/30,000 at time of challenge, compared to 1/700 in animals receiving DNA as a sole immunogen. Neutralizing antibody titers against SIVmneE11S were detected in only two animals prior to challenge, and only after the fourth immunization (Fig. 3). Both animals were in the DNA plus subunit group (95022 and 95024). Proliferative responses to rgp160 (Fig. 4) and to whole inactivated virus (data not shown) were induced equally well by both vaccine regimens. Weak responses were detected as early as postsecond immunization in three of the vaccinees (,2000 net cpm). Following the fourth immunization, at time of challenge, the number of responders (8 of 8) and the magnitude of FIG. 3. Results of in vitro homologous virus neutralizing assay on pre- and postchallenge serum from macaques. Data are expressed as titer at which 50% virus is neutralized. Titers for animals vaccinated with DNA alone are shown in (A) 95010 (diamonds), 95011 (squares), 95045 (triangles), and 95047 (circles). Titers for animals vaccinated with DNA plus subunit boost are shown in (B) 95014 (diamonds), 95018 (squares), 95022 (triangles), and 95024 (circles). Titers for control animals are shown in (C) those vaccinated with plasmid vector alone are 95013 (diamonds) and 95027 (squares), and with vector plus adjuvant boost are 95042 (triangles) and 95057 (circles). Arrow represents time of challenge, and the horizontal dotted line indicates the limit of detection of the assay. FIG. 2. Pre- and postchallenge serum antibody titers to Env gp160 by ELISA. Animals vaccinated with DNA alone are shown in (A) 95010 (diamonds), 95011 (squares) 95045 (triangles), and 95047 (circles). Animals vaccinated with DNA plus subunit boost are shown in (B) 95014 (diamonds), 95018 (squares), 95022 (triangles), and 95024 (circles). Control animals are shown in (C) those vaccinated with plasmid vector alone are 95013 (diamonds) and 95027 (squares), and with vector plus adjuvant boost are 95042 (triangles) and 95057 (circles). Arrows represent times of immunization, and the vertical line at week 38 indicates time of challenge. the responses had increased markedly, displayed as net counts incorporated and converted to stimulation indices (Fig. 4). We were unable to detect bulk SIV-specific cytolytic activity after in vitro stimulation of PBMC from any of the vaccinated animals prior to challenge, although CTL were readily detected using this protocol in infected macaques postchallenge, noted below. However, cytolytic T cell clones specific for Env and Gag-Pol were detectable in two vaccinees following two DNA immunizations.23 At 38 weeks postinitiation, 2 weeks postfinal immunization, all macaques were challenged intrarectally with 20 MID of SIVmne uncloned virus. Outcome postchallenge was monitored by assessing viral burden over time, determining viral RNA in plasma and proviral DNA in PBMC and lymph nodes, and also by evaluation of CD41 T cell counts in peripheral blood. All PROTECTION FROM SIV WITH MULTIGENIC DNA VACCINES 429 caques 95010 and 95011, immunized with DNA alone, by both assays. Consistent with the QC-RT-PCR data, virus was undetectable in animal 95010 after the acute phase of viremia (week 8 postchallenge, week 46 postinitiation). Indeed, we were unable to detect proviral DNA in the lymph node of 95010, suggesting that this macaque may have been only transiently infected. Of the DNA plus subunit immunized macaques, provirus was isolated from the PBMC only sporadically in 95022 relative to the other animals of the group, suggesting control of virus load consistent with the quantitative plasma viral RNA data. Although control animal 95013 had low levels of plasma viremia, provirus was readily isolated from PBMC at most time points tested. To determine which species of virus was transmitted, we performed heteroduplex mobility analysis (HMA) of the V1–V2 FIG. 4. Lymphoproliferative responses to rgp160 in PBMC from immunized macaques on day of challenge. Data are expressed as counts per minute of tritium incorporated, with background to medium alone subtracted (net CPM) and also as a stimulation index. animals became infected postchallenge, but protective immune responses were elicited by both vaccine regimens. Viral RNA in plasma was assessed by QC-RT PCR assay over the course of 1 year postchallenge (Fig. 5). Three of four macaques receiving DNA alone maintained low virus loads (,5 3 104 copies/ml plasma) for the duration of the experiment. Two of these macaques, 95010 and 95011, had plasma virus levels below the level of detection of the QC-RT-PCR assay at all time points, with the exception of a single time point during the acute phase of viremia for animal 95010. One of the subunit-boosted animals died at 8 months postchallenge due to causes unrelated to SIV infection. Of the remaining three macaques, 95022 alone was able to control virus long term, with plasma virus copy number being below the level of detection for the assay at all but one time point following resolution of the acute phase of infection. Macaque 95013 in the control group was also able to control levels of plasma virus postchallenge, with the remaining three animals in this group showing high acute peak virus loads and high viral set points out to 1 year postchallenge. There was a trend for a significant difference in peak viral load, measured at week 2 postchallenge, between DNA immunized animals compared to controls (p 5 0.1) and between all vaccinees compared to controls (p 5 0.07). Furthermore, analysis of acute levels of viral RNA between weeks 0 and 6 postchallenge showed a similar trend (p 5 0.1 in each case). There was no significant difference between the two vaccine groups in ability to control levels of plasma viremia postchallenge. Detection of cell-associated proviral DNA by coculture assay and by PCR up to 20 weeks postchallenge (58 weeks postinitiation) is shown in Table 1. In general, detection of virus in PBMC by culture in vitro was delayed in vaccinees relative to controls. Provirus was only sporadically detectable in ma- FIG. 5. Plasma virus load determinations postchallenge by QC-RT-PCR assay. Number of viral copies per/ml plasma for animals vaccinated with DNA alone are shown in (A) 95010 (diamonds), 95011 (squares), 95045 (triangles), and 95047 (circles). Results for animals vaccinated with DNA plus subunit boost are shown in (B) 95014 (diamonds), 95018 (squares), 95022 (triangles), and 95024 (circles). Results for control animals are shown in (C) those vaccinated with plasmid vector alone are 95013 (diamonds) and 95027 (squares), and with vector plus adjuvant boost are 95042 (triangles) and 95057 (circles). Arrow represents time of challenge, and the horizontal dashed line indicates the limit of detection of the assay. 430 MOSSMAN ET AL. TABLE 1. VIRAL COCULTURE AND PROVIRAL DNA IN PBMC AND LNMC POSTCHALLENGE a Weeks postchallenge Vaccine group DNA alone 95010 95011 95045 95047 DNA plus Subunit 95014 95018 95022 95024 Controls 95013 95027 95042 95057 1 2 3 4 6 8 12 14 LN 16 20 2/2c 2/2 1/2 2/2 2/2 2/2 2/2 2/2 2/2 2/2 2/1 2/1 2/3 2/2 2/2 1/1 2/1 2/2 2/1 1/1 1/2 2/1 1/1 1/2 2/2 2/2 2/1 2/1 2/2 1/1 1/1 1/1 2/2 1/2 2/2 1/2 2/2 2/2 2/2 1/2 2/2 2/2 2/2 2/2 2/1 1/2 2/1 2/2 1/1 1/2 2/1 2/2 1/2 1/2 1/2 2/1 1/1 1/1 1/2 1/1 1/1 1/1 1/1 1/1 1/1 1/2 2/2 2/1 1/1 1/1 2/1 1/1 1/2 1/2 2/2 1/2 1/2 1/2 2/2 1/2 2/2 2/2 1/2 2/2 1/2 1/1 1/2 1/2 1/1 2/1 1/1 1/1 2/2 1/1 1/1 1/1 2/1 1/1 1/1 1/1 1/1 2/1 1/2 1/2 2/1 2/1 1/1 1/1 1/1 1/1 1/1 1/1 1/2 2/2 1/2 1/2 1/2 1/2 2/2 2/2 a Where no result is indicated, assays were not performed due to lack of available sample. PBMC were tested for all weeks except 14, where LNMC were tested. Results are shown as “1” or “2” at each time point for provirus detection by viral coculture (left of slash)/nested LTR-gag PCR assay (right of slash). env region of proviral DNA extracted from PBMC at 6 weeks postchallenge. Amplified sequences from each animal were mixed individually with the same region from molecular clone 8 of SIVmneE11S .19 The HMA of these mixtures showed no diversification, indicating that the predominant virus in the SIVmne swarm (E11S) was transmitted to all of the animals, vaccinees and controls (data not shown). This virus shares sequence homology with the Envelope, Gag-Pol, and Nef used in the vaccine components, which were derived from the SIVmneE11S clone 8. CD41 T cell counts were monitored for 1 year postchallenge as a further indication of the ability of macaques to control the SIV challenge (Fig. 6). In the SIVmne infection and pathogenesis model in M. fascicularis, 50–60% of naive control macaques infected with either SIVmneE11S or uncloned SIVmne experienced relatively slow CD41 T cell decline and developed AIDS-like diseases within 3 years after infection; however disease progression is more rapid with the uncloned virus.14 Within the control group, only 95013 maintained normal CD41 T cell counts by the termination of the study (94 weeks), but only 95027 declined to 500 cells/ml. We utilized 1000 cells/ml as a cutoff in this study, based on published patterns of CD41 T cell decline in the model, since this level is maintained in healthy animals, and no recovery is seen once the CD4 cells drop below this level. Peripheral CD41 T cells were maintained above 1000 cells/ml blood in three of four macaques immunized with DNA alone. The fourth animal in this group, 95045, dropped below but close to this level after week 40 postchallenge (week 78 postinitiation). Of the three surviving DNA plus subunit boost macaques, only 95022 had maintained CD41 T cell counts above 1000 cells/ml blood by the end of the study at 1 year postchallenge. There was a statistically significant delay in time to CD41 T cell decline to ,1000 cells/ml blood relative to controls for the DNA immunized macaques (p 5 0.007). This statement is also true when all vaccinees were compared with controls (p 5 0.01). As expected, the CD4 data show a close inverse correlation with levels of plasma viremia. Consistent with plasma viremia data, there was no significant difference between the two vaccine groups in maintenance of CD4 counts following challenge. Postchallenge cellular immunity was assessed in four vaccinees and two control macaques using chromium release cytolytic assays (Fig. 7). Bulk PBMC were tested without freezing and stimulated with recombinant vaccinia virus-expressed SIV proteins. No CTL directed to Env or to Gag/Pol were detected in vaccinee 95018, which controlled viremia after the acute phase (data not shown). When tested by stimulation with Gag/Pol, Env, and Nef, PBMC from vaccinees with low or no detectable viral replication postchallenge had borderline positive responses to Gag/Pol (95011) and Nef (95010) at 2 months following challenge. DNA vaccinee 95045, with relatively poor virus control, had strong Nef and weaker Gag/Pol responses at 5 months postchallenge. At 2 months postchallenge, bulk CTL specific for Env (95027) and for Gag/Pol and Env (95057) were seen at low levels in controls with poor postacute control of viremia and ultimate disease progression (Fig. 7). Anti-Envelope gp160 ELISA antibodies were boosted in most macaques following exposure to challenge virus, and were maintained at steady levels over the course of the study, out to 1 year postchallenge (Fig. 2). Interestingly, animal 95011 did not exhibit an anamnestic boost in gp160 titers postchallenge, further evidence of the low levels of viral replication in this animal, even at the acute phase, where viral DNA and RNA was undetectable (Fig. 5 and Table 1). Neutralizing antibody titers developed in most macaques by 16 weeks following challenge (54 weeks postinitiation) (Fig. 3). In general, peak titers of neutralizing antibodies postchallenge were higher in vaccinees than in control animals, suggesting priming of this response by the PROTECTION FROM SIV WITH MULTIGENIC DNA VACCINES FIG. 6. CD41 T cell counts in peripheral blood of vaccinated macaques postchallenge. Number of CD41 cells per ml blood for animals vaccinated with DNA alone are shown in (A) 95010 (diamonds), 95011 (squares), 95045 (triangles), and 95047 (circles). Results for animals vaccinated with DNA plus subunit boost are shown in (B) 95014 (diamonds), 95018 (squares), 95022 (triangles), and 95024 (circles). Results for control animals are shown in (C) those vaccinated with plasmid vector alone are 95013 (diamonds) and 95027 (squares), and with vector plus adjuvant boost are 95042 (triangles) and 95057 (circles). Arrow represents time of challenge. vaccines. Indeed, there was a statistically significant trend for higher neutralization titers in DNA plus subunit immunized animals compared to controls at 16 weeks postchallenge (week 54 postinitiation, p 5 0.1) and at 44 weeks postchallenge (week 82 postinitiation, p 5 0.07). In the DNA plus subunit group animal 95022 had the highest neutralizing titer prechallenge and early postchallenge, and animals 95010 and 95047 had the highest postchallenge titers among the animals immunized with DNA alone (Fig. 3). All three of these animals controlled viral replication to some extent following challenge. DISCUSSION In this study we elected to challenge macaques by the mucosal (intrarectal) route with the uncloned stock of SIVmne. Heteroduplex mobility assay of proviral genomes from PMBC of 431 these animals postchallenge shows that the E11S variant alone was detected in the blood. This variant, present in the complex stock, appears to preferentially cross the mucosal barrier to establish infection, as has been reported previously.17 Sexual transmission of a single viral species is also seen in infection of humans with HIV-1.25,26 Thus, protection in this challenge model may have additional relevance to the development of an HIV vaccine that protects against mucosal transmission of the virus. Failure to protect from infection by this variant, despite its identity with the vaccine Envelope immunogen in all components (DNA and rgp160), suggests that improvements are needed to elicit strong neutralizing antibodies at the site of infection. Like others, we have demonstrated that naked DNA alone is not sufficient to induce the levels of protection required by an AIDS vaccine for induction of sterilizing immunity.27,28 However, the results presented here indicate that vectors engineered to express multiple viral genes, to make VLPs in infected cells, and additionally selected for optimal expression levels were able to suppress viral replication and to significantly maintain CD41 T cell counts above a threshold level following challenge in three of four animals (p 5 0.007). Peak (week 2) viral loads were lower in vaccinated macaques than in controls, trending toward significance (p 5 0.07). Median peak viral RNA levels were 3 logs lower in vaccinated animals than controls, but this was not significantly different (p 5 0.1). The reduction in viremia is less than that seen in SHIV89.6P challenge experiments reported recently.4 Whether this difference is due to the immunogenicity of the specific vaccine constructs or to differences in control of viral replication between SHIV and SIV models, or both, remains to be clarified. The SHIV89.6P model has recently been the focus of questions due to its unusual course of pathogenesis and CD41 T cell decline.29 In this study, we had the choice of two challenge stocks of SIV that had been titered in vivo and utilized extensively for vaccine studies: uncloned SIVmne and the biological clone SIV mneE11S . These models both have gradual rather than precipitous CD41 cell decline, and depletion occurs more rapidly in some of the macaques infected with the uncloned virus than in those infected with E11S.14 We chose to use the uncloned stock as a more robust challenge that would provide us a greater opportunity to measure disease onset in a shorter period of time. A drop in CD41 T cells below 1000 in this species is uniformly followed by gradual and irretrievable loss to very low levels with onset of AIDS-like disease following. Because our study was less than 2 years in duration, we used a threshold of 1000 cells/ml below which to predict disease progression in controls and in vaccinees. This level differs from that utilized in most published studies but was necessary due to the slow erosion of T cells seen in the SIVmne disease course. The mechanism of protective immunity induced by the DNA vaccines is unclear from these studies. Immunization of macaques with DNA alone induced moderately high ELISA antibody titers to gp160. It is likely that the level of antibodies achieved here is due to the production of VLPs in infected cells, enhancing presentation of antigen to the immune system. Neutralizing antibodies were measured at higher titers and were more sustained in the vaccinated groups compared with controls following challenge. Thus CD41 T cell help was effectively stimulated for the production of virus binding and neu- 432 MOSSMAN ET AL. FIG. 7. Cytolytic T cell assays of bulk PBMC from SIV-infected macaques at various time points postchallenge. PBMC were stimulated in vitro with recombinant vaccinia constructs expressing SIV antigens as noted in the individual graphs. These cultures were then tested for their ability to lyse autologous B-LCL target cells in an antigen-specific manner by chromium release at three different effector to target (E:T) ratios. Specific targets were B-LCL infected with vaccinia viruses expressing GagPol, Env, or Nef and uninfected B-LCL (Uninfected) and cells infected with vaccinia virus expressing b-galactosidase (Vacc-Lac) were used as negative controls. PBMC from 95010, 95011, 95057, and 95027 were tested 9 weeks postchallenge; PBMC from 95045 were tested 5 months postchallenge. tralizing antibodies. The presentation of the native Envelope protein by expression of authentic Env gp160 in vivo after DNA immunization likely facilitated this response. Although there was not a universal correlation between the presence of neutralizing antibodies and control of plasma viremia in individual macaques, it cannot be ruled out as a potential protective factor in certain animals. Those with the highest titers pre- and early postchallenge controlled virus to some degree, and neu- tralizing antibodies were higher in titer and sustained longer in vaccinees relative to controls. The production of particulate antigen by the gag-pol-envvector is likely to enhance the ability to induce a CD81 T cell response through phagocytosis by antigen-presentingcells and introduction of antigen into the cytosol.30 CTL responses in CD81 T cells were induced by the DNA, which would also utilize the classic class I pathway in transfected cells, but these were of PROTECTION FROM SIV WITH MULTIGENIC DNA VACCINES insufficient frequency to be detectable in bulk cultures of PBMC by chromium release assay prior to challenge. In macaques that were tested for the induction of CTL postchallenge, bulk responses to Gag/Pol, Env, and Nef were readily detected. Bulk CTL were more readily detected in those with detectable postacute viremia. However, we did not obtain postchallenge CTL data for all animals. More sensitive and quantitative methods for detection of antigen-specific CD81 T cells were not used here due to technical and sample limitations, and thus the role played by these effectors in vaccine induced protection is not clear. Surprisingly, boosting DNA-elicited responses with subunit proteins in adjuvant did not further improve outcome postchallenge. Although humoral responses were increased relative to DNA alone, antigen-specific T cell proliferation was equivalent between the two groups. The finding that DNA-subunit prime-boost vaccines failed to induce sterilizing immunity after intrarectal challenge with SIVmne uncloned virus is in contrast to results in the same model with vaccinia virus priming followed by subunit boosting.17 This observation underscores the importance of elucidating differences between live virus and DNA priming and of understanding the immunological correlates involved in protection. We believe that the boosting immunogen could be improved by using lower doses of protein for selection of T cells with higher affinities,31,32 more potent adjuvants, and/or improved methods for delivery of antigens to the MHC class I pathway for presentation to CD81 T cells. For more optimal elicitation of neutralizing antibodies, better presentation via the MHC class II pathway may be needed, and this version of Envelope expressed in and extracted from vaccinia-virus-infected cells is potentially compromised in key conformational determinants. In addition, recent data suggest that the rational design of Envelope immunogens may be required for more effective induction of neutralizing antibody responses.3 Development in these areas should improve the potential for using subunit proteins to boost and maintain immune responses primed by gene-based vaccines. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. ACKNOWLEDGMENTS This work was supported by Public Health Service Grant AI26503 from the National Institute of Allergy and Infectious Diseases. The authors thank Chiron Corporation for the generous provision of MF-59. We thank P.A. Luciw for a gift of pSV2neo and for support of electron microscopy work; N. Doria-Rose, V. Hirsch, and L. Stamatatos for critical review of the manuscript; and J. Oberembt for proofreading and formatting assistance. REFERENCES 1. Boyer JD, Ugen KE, Wang B, et al.: Protection of chimpanzees from high-dose heterologous HIV-1 challenge by DNA vaccination. Nat Med 1997;3:526–532. 2. Letvin NL, Montefiori DC, Yasutomi Y, et al.: Potent, protective anti-HIV immune responses generated by bimodal HIV envelope 15. 16. 17. 18. 19. 20. 433 DNA plus protein vaccination. Proc Natl Acad Sci USA 1997; 94:9378–9383. Barnett SW, Lu S, Srivastava I, et al.: The ability of an oligomeric human immunodeficiency virus type 1 (HIV-1) envelope antigen to elicit neutralizing antibodies against primary HIV-1 isolates is improved following partial deletion of the second hypervariable region. J Virol 2001;75:5526–5540. Shiver JW, Fu TM, Chen L, et al.: Replication-incompetent adenoviral vaccine vector elicits effective anti-immunodeficiencyvirus immunity. Nature 2002;415:331–335. Aguiar JC, Hedstrom RC, Rogers WO, et al.: Enhancement of the immune response in rabbits to a malaria DNA vaccine by immunization with a needle-free jet device. Vaccine 2001;20:275–280. O’Hagan D, Singh M, Ugozzoli M, et al.: Induction of potent immune responses by cationic microparticles with adsorbed human immunodeficiency virus DNA vaccines. J Virol 2001;75: 9037–9043. Allen TM, Vogel TU, Fuller DH, et al.: Induction of AIDS virusspecific CTL activity in fresh, unstimulated peripheral blood lymphocytes from rhesus macaques vaccinated with a DNA prime/modified vaccinia virus Ankara boost regimen. J Immunol 2000;164:4968–4978. Amara RR, Villinger F, Altman JD, et al.: Control of a mucosal challenge and prevention of AIDS by a multiprotein DNA/MVA vaccine. Science 2001;292:69–74. Estcourt MJ, Ramsay AJ, Brooks A, et al.: Prime-boost immunization generates a high frequency, high-avidity CD8(1) cytotoxic T lymphocyte population. Int Immunol 2002;14:31–37. Hanke T, Samuel RV, Blanchard TJ, et al.: Effective induction of simian immunodeficiency virus-specific cytotoxic T lymphocytes in macaques by using a multiepitope gene and DNA prime-modified vaccinia virus Ankara boost vaccination regimen. J Virol 1999;73:7524–7532. Kent SJ, Zhao A, Best SJ, et al.: Enhanced T-cell immunogenicity and protective efficacy of a human immunodeficiency virus type 1 vaccine regimen consisting of consecutive priming with DNA and boosting with recombinant fowlpox virus. J Virol 1998;72: 10180–10188. Haigwood NL: Progress and challenges in therapies for AIDS in nonhuman primate models. J Med Primatol 1999;28:154–163. Joag SV: Primate models of AIDS. Microbes Infect 2000;2: 223–229. Polacino PS, Stallard V, Klaniecki JE, et al.: Role of immune responses against the envelope and the core antigens of simian immunodeficiency virus SIVmne in protection against homologous cloned and uncloned virus challenge in Macaques. J Virol 1999; 73:8201–8215. Hu S-L, Abrams K, Barber GN, et al.: Protection of macaques against SIV infection by subunit vaccines of SIV envelope glycoprotein gp160. Science 1992;255:456–459. Hu S-L, Stallard V, Abrams K, et al.: Protection of vaccinia-primed macaques against SIVmne infection by combination immunization with recombinant vaccinia virus and SIVmne gp160. J Med Primatol 1993;22:92–99. Polacino P, Stallard V, Montefiori DC, et al.: Protection of macaques against intrarectal infection by a combination immunization regimen with recombinant simian immunodeficiency virus SIVmne gp160 vaccines. J Virol 1999;73:3134–3146. Mossman SP, Pierce CC, Robertson MN, et al.: Immunization against SIVmne in macaques using multigenic DNA vaccines. J Med Primatol 1999;28:206–213. Benveniste RE, Arthur LO, Tsai CC, et al.: Isolation of a lentivirus from a macaque with lymphoma: Comparison with HTLV-III/LAV and other lentiviruses. J Virol 1986;60:483–490. Watson A, Ranchalis J, Travis B, et al.: Plasma viremia in ma- 434 21. 22. 23. 24. 25. 26. 27. 28. MOSSMAN ET AL. caques infected with simian immunodeficiency virus: Plasma viral load early in infection predicts survival. J Virol 1997;71:284–290. Delwart EL, Shpaer EG, Louwagie J, et al.: Genetic relationships determined by a DNA heteroduplex mobility assay: Analysis of HIV-1 env genes. Science 1993;262:1257–1261. Montefiori DC, Robinson WE, Jr., Schuffman SS, et al.: Evaluation of antiviral drugs and neutralizing antibodies to human immunodeficiency virus by a rapid and sensitive microtiter infection assay. J Clin Microbiol 1988;26:231–235. Haigwood NL, Pierce CC, Robertson MN, et al.: Protection from pathogenic SIV challenge using multigenic DNA vaccines. Immunol Lett 1999;66:183–188. Journot V, Chene G, Joly P, et al.: Viral load as a primary outcome in human immunodeficiency virus trials: A review of statistical analysis methods. Control Clin Trials 2001;22:639–658. Zhu T, Mo H, Wang N, et al.: Genotypic and phenotypic characterization of HIV-1 patients with primary infection. Science 1993;261:1179–1181. Zhu T, Wang N, Carr A, et al.: Genetic characterization of human immunodeficiency virus type 1 in blood and genital secretions: Evidence for compartmentalization and selection during sexual transmission. J Virol 1996;70:3098–3107. Lu S, Arthos J, Montefiori DC, et al.: Simian immunodeficiency virus DNA vaccine trial in macaques. J Virol 1996;70:3978–3991. Robinson HL, Montefiori DC, Johnson RP, et al.: Neutralizing an- 29. 30. 31. 32. tibody-independent containment of immunodeficiency virus challenges by DNA priming and recombinant pox virus booster immunizations. Nat Med 1999;5:526–534. Feinberg MB and Moore JP: AIDS vaccine models: Challenging challenge viruses. Nat Med 2002;8:207–210. Kovacsovics-Bankowski M and Rock KL: A phagosome-to-cytosol pathway for exogenous antigens presented on MHC class I molecules. Science 1995;267:243–246. Alexander-Miller MA, Leggatt GR, and Berzofsky JA: Selective expansion of high- or low-avidity cytotoxic T lymphocytes and efficacy for adoptive immunotherapy. Proc Natl Acad Sci USA 1996;93:4102–4107. Rees W, Bender J, Teague TK, et al.: An inverse relationship between T cell receptor affinity and antigen dose during CD4(1) T cell responses in vivo and in vitro. Proc Natl Acad Sci USA 1999;96:9781–9786. Address reprint requests to: Nancy L. Haigwood Seattle Biomedical Research Institute 307 Westlake Ave. N, Suite 500 Seattle, Washington 98109-5219 E-mail: nancy.haigwood@sbri.org This article has been cited by: 1. Antonella Caputo, Riccardo Gavioli, Stefania Bellino, Olimpia Longo, Antonella Tripiciano, Vittorio Francavilla, Cecilia Sgadari, Giovanni Paniccia, Fausto Titti, Aurelio Cafaro, Flavia Ferrantelli, Paolo Monini, Fabrizio Ensoli, Barbara Ensoli. 2009. HIV-1 Tat-Based Vaccines: An Overview and Perspectives in the Field of HIV/AIDS Vaccine Development. International Reviews of Immunology 28:5, 285-334. [CrossRef] 2. Marie-Claude Boily, Laith Abu-Raddad, Kamal Desai, Benoit Masse, Steve Self, Roy Anderson. 2008. Measuring the public-health impact of candidate HIV vaccines as part of the licensing process. The Lancet Infectious Diseases 8:3, 200-207. [CrossRef] 3. Shan Lu. 2006. Combination DNA plus protein HIV vaccines. Springer Seminars in Immunopathology 28:3, 255-265. [CrossRef] 4. Laurence E. Shields, Aimee J. Sieverkropp, Jennifer Potter, Robert G. Andrews. 2006. Phenotypic and cytolytic activity ofMacaca nemestrina natural killer cells isolated from blood and expanded in vitro. American Journal of Primatology 68:8, 753-764. [CrossRef] 5. Carey Farquhar, Ruth Nduati, Nancy Haigwood, William Sutton, Dorothy Mbori-Ngacha, Barbra Richardson, Grace John-Stewart. 2005. High Maternal HIV-1 Viral Load During Pregnancy Is Associated With Reduced Placental Transfer of Measles IgG Antibody. JAIDS Journal of Acquired Immune Deficiency Syndromes 40:4, 494-497. [CrossRef] 6. Diane E Webster, Merlin C Thomas, Raelene Pickering, Andrew Whyte, Ian B Dry, Paul R Gorry, Steve L Wesselingh. 2005. Is there a role for plant-made vaccines in the prevention of HIV/AIDS?. Immunology and Cell Biology 83:3, 239-247. [CrossRef] 7. Stephen M. Smith, Mahender Singh, Kuan-Teh JeangVaccine Approaches for Protection Against HIV . [CrossRef]