The Use and Interpretation of Quantitative Terminology in Reporting
advertisement

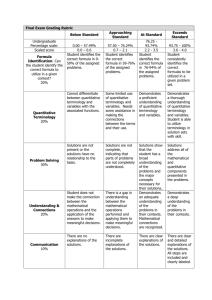
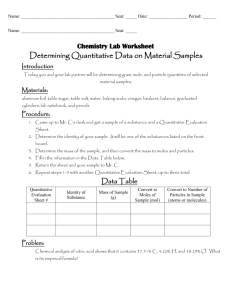
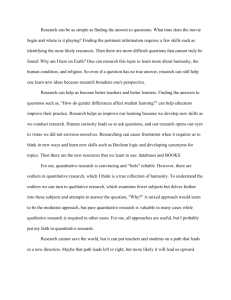
ISLH Laboratory Hematology 7:85-88 © 2001 Carden Jennings Publishing Co., Ltd. Official Publication The Use and Interpretation of Quantitative Terminology in Reporting of Red Blood Cell Morphology LAWRENCE HOOKEY, DAVID DEXTER, DAVID H. LEE Departments of Medicine and Pathology, Queen’s University, Kingston, Ontario, Canada ABSTRACT INTRODUCTION Despite advances in diagnostic technology in the hematology laboratory, the evaluation of peripheral blood films for abnormal red blood cell (RBC) morphology remains a manual task. The terminology used by laboratory technologists to describe the frequency of morphologically abnormal RBCs in peripheral blood films has rarely been studied. We conducted a study to determine the variability in the use of these quantitative descriptors and to determine how physicians interpret these terms. Thirty-one hematology laboratory technologists from 6 hospitals were asked to quantitate abnormal RBCs in a series of peripheral blood films using their usual terminology. Interpretation of these quantitative terms by the attending physicians and residents from an Internal Medicine teaching program was also assessed. We found a wide variation in the use of quantitative descriptors between technologists and between centers. Physicians’ interpretations of these terms varied, with some terms having a narrow, consistent interpretation and others having a broader range of interpretations. We suggest that the precision of communication between the hematology laboratory staff and clinicians can be improved by tailoring the use of quantitative terminology to avoid terms that have a broad range of interpretations by physicians. Lab. Hematol. 2001;7:85-88. Despite advances in diagnostic laboratory technology, the assessment of peripheral blood films for red blood cell (RBC) morphologic abnormalities remains a manual task that is inherently subjective. The frequency of morphologically abnormal RBCs (such as target cells or schistocytes) in a blood film can have significant implications on diagnosis and clinical management; therefore, quantitative descriptors (such as rare or occasional) are frequently included in morphology reports. Accurate communication of the frequency of abnormal RBCs is entirely dependent on the wording used in morphology reports; however, this aspect of laboratory practice has not been studied or evaluated in quality assurance programs. We conducted a study to determine the variability in the quantitative terminology used by laboratory technologists to describe the frequency of abnormal RBCs in a set of standard peripheral blood films. We also surveyed physicians to ascertain how they interpreted these quantitative descriptors. KEY WORDS: METHODS Assessment of Terminology Used by Laboratory Technologists Clinical laboratory technologists from one tertiary care teaching hospital in Kingston, Ontario and 5 non-teaching hospitals in southeastern Ontario were invited to participate if reviewing peripheral blood films was a routine part of their laboratory responsibilities. A standard set of 7 peripheral blood–film slides depicting target cells (2 slides), schistocytes (2 slides), teardrop cells (1 slide), acanthocytes (1 slide), and RBCs containing Howell-Jolly bodies (1 slide) were prepared with Wright’s stain [1], and viewed by all participants using Red blood cell · Morphology · Reporting · Interpretation Correspondence and reprint requests: David H. Lee, Etherington Hall, Queen’s University, 94 Stuart Street, Kingston, Ontario, Canada, K7L 3N6; (613) 533-6329; fax: (613) 533-6855 (e-mail:leedh@meds.queensu.ca). Received January 3, 2001; received in revised form April 3, 2001; accepted April 4, 2001 85 86 L. Hookey et al Quantitative descriptors used by technologists and their interpretation by physicians. The upper 7 panels depict the frequencies of terms used by technologists to describe the quantity of abnormal red blood cells in a set of 7 peripheral blood films. The lower panel depicts the physicians’ interpretation of the terms: the mean (), standard deviation (error bars), and minimum and maximum values () are shown for each term. Results of statistical comparison between physician interpretations of terms are shown in Table 2. their usual microscopes in their own laboratories. For each slide, the type of abnormal RBC to be quantitated was given, and each technologist selected the quantitative descriptor that they would normally use to report the frequency of the abnormal RBC from a list of terms. The list of terms was generated after consultation with technologists prior to the study. Technologists were observed during the study to ensure that no collaboration occurred. list. This was done using 0 to 10 ordinal scale for each term, anchored at each end by the terms none and all, respectively. Interpretation of Terminology by Physicians Residents and attending physicians in the Internal Medicine training program at Queen’s University in Kingston, Ontario were surveyed to determine how frequent they perceived a morphologic abnormality to be for each term on the Thirty-one technologists from 6 hospitals and 32 physicians from 1 hospital participated. The responses of laboratory technicians are shown in the Figure. Responses were heterogeneous for all slides. For 6 of the 7 slides, fewer than half of participants used the same term to describe the Statistical Analysis The Wilcoxon signed rank test was performed to compare paired physician responses. RESULTS Quantitative Terminology in Reporting of Red Blood Cell Morphology 87 TABLE 1. Frequency of Terminology Used by Each Center Centers No. of technologists Terminology used Rare Slight Occasional Few Mild Present Moderate Many Marked Other All 1* 2 3 4 5 6 31 11 4 4 4 5 3 10 16 28 44 1 36 50 12 4 16 4 9 20 17 1 4 16 4 1 1 0 5 5 6 0 0 10 2 0 0 5 0 0 6 0 0 14 0 1 2 1 0 3 10 0 1 7 4 1 1 0 0 0 0 0 30 0 0 0 5 0 2 0 5 0 1 3 2 1 7 *Tertiary care center. frequency of the abnormality. Certain terms were used more frequently by certain centers (Table 1). The term rare was used mainly in centers 1 and 3. Slight was used primarily in centers 1 and 2. Occasional was used primarily in center 1 and present was used almost exclusively in center 5. The physicians’ interpretations of the terms used by the technologists are arranged in ascending order (Figure, lower panel). When pairs of terms were compared, the differences in interpretation between most terms were found to be statistically significant (Table 2), but the magnitudes of the differences between some terms is small. There was heterogeneity in the scatter of responses to the terms (Figure, lower panel). For example, the term rare had little variation in perceived meaning: all responses were clustered at the low end of the scale. In contrast, the term present had a broader meaning to physicians, with responses distributed over a wider range. DISCUSSION In this study, we observed heterogeneity in the quantitative terms used by laboratory technologists to report the fre- quency of RBC morphologic abnormalities. This variation was present between centers and between technologists. Furthermore, many of the different quantitative terms used to describe the same blood film are interpreted differently by physicians. To our knowledge, these aspects of hematology morphology reporting have not been studied previously. The current study focused on the responses of technologists and physicians, rather than on the variables that contributed to these responses. Likely, the choice of terminology by technologists is dependent on several variables including (1) the perceived frequency of the abnormality by the technologist, (2) the perceived meaning of the various terms by the technologist, and (3) laboratory policy and local practices. Similarly, the interpretation of these terms by physicians is likely influenced by (1) the physician’s concept of the terminology, (2) their familiarity with abnormal RBC morphology and its reporting, and (3) previous exposure to the terminology. The latter 2 influences are probably dependent on the specialty and experience of the physician and may also depend on existing regional reporting practices to which the physician is accustomed. Although the physicians surveyed TABLE 2. Wilcoxon Signed Rank Test P Values for Comparison of Physicians’ Interpretations of Quantitative Terms Slight Present Moderate Few Mild Marked Occasional Many Rare Slight Present Moderate Few Mild Marked Occasional Many Rare — <.001 <.001 <.001 .001 <.001 .001 <.001 <.001 <.001 — .039 .003 .012 <.001 .002 <.001 <.001 <.001 .039 — <.001 <.001 <.001 <.001 <.001 <.001 <.001 .003 <.001 — .174 <.001 .197 <.001 <.001 .001 .012 <.001 .174 — <.001 .013 <.001 <.001 <.001 <.001 <.001 <.001 <.001 — <.001 <.001 <.001 .001 .002 <.001 .197 .013 <.001 — <.001 <.001 <.001 <.001 <.001 <.001 <.001 <.001 <.001 — <.001 <.001 <.001 <.001 <.001 <.001 <.001 <.001 <.001 — 88 L. Hookey et al represent a single specialty rather than a general cross-section of physicians, they do make up a specialty (Internal Medicine) that is an important consumer of laboratory information. It is not known whether the observed technician and physician responses are generalizable, nor is it known whether the differences in terminology use or interpretation are of sufficient magnitude to affect clinical management. Understanding how clinicians interpret quantitative terminology may lead to improved patient care. For example, avoiding the use of terms that are vague (eg, the term present) might improve the usefulness of the morphology report. Recognition of the limitations of specific words and the inconsistent use of terminology may also be relevant for laboratory quality improvement. Hematology laboratory external quality assessment programs evaluate blood film interpretation [2,3] but quantitation of abnormal cells is infrequently evaluated, partly because of the inconsistent distribution of abnormal leukocytes in blood films. To our knowledge, the distribution of the abnormal non-nucleated RBCs examined in our study would not be expected to vary significantly from region to region within the same slide. Based on the results of our study, we do not recommend the use of the term present as a quantitative descriptor for RBC morphology reporting because of the wide variation in meaning to clinicians. To minimize the risk of being misunderstood, laboratory technologists should be encouraged to use terms that have relatively uniform interpretations and to recognize that terms used by individual technologists may have a different meaning to clinicians. Although we did not ascertain how technologists judge the same panel of terms, similar patterns of variability of interpretation likely exist within this group. How can each hematology laboratory optimize its choice of quantitative descriptors? We believe that the local clinicians who regularly use the laboratory should be surveyed as was done in our study. In this fashion local tendencies and differences can be taken into account when selecting a menu of quantitative descriptors for use in reports. Such a survey need not be cumbersome: our physician survey took approximately 1 minute to complete, and our group of 32 physicians in a tertiary care center were surveyed in 1 day. We propose that these measures and further study of quantitative descriptors in peripheral blood film reporting will improve the precision of communication between the hematology laboratory and clinicians. REFERENCES 1. Luna LG. Histopathologic Methods and Color Atlas of Special Stains and Tissue Artifacts. Gaitheresburg, Md: American Histolabs; 1992. 2. Lewis SM. The WHO International External Quality Assessment Scheme for haematology. Bull World Health Organ. 1988;66:283-290. 3. Lewis SM. Blood film evaluations as a quality control activity. Clin Lab Haematol. 1990;12(suppl 1):119-127.