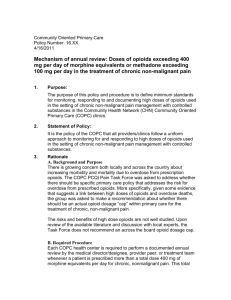
Opioid Conversions Resident Handout

OPIOID CONVERSIONS
1.
Converting Short acting Æ Long Acting (IR Æ SR) when pain is well ‐ controlled
*Use for :
¾ CHRONIC pain
¾ Pts on scheduled IR opioids – pain that recurs before the next dose
PP: ‐ Can use equianalgesic dosing when using same drug
‐ Avoid combination agents if you’re at this step
‐ Bowel regimen, bowel regimen, bowel regimen
Instructions:
1.
Calculate how many mg of opioid pt is using in 24 hrs Æ convert that amt to long ‐ acting
Opioid (SR)
2.
Add a rescue doses (IR) of same opioid if possible ‐ should be~10 ‐ 20% of total daily
opioid dose
Case1: Mr.
Smith is a 58 ‐ year old AAM with chronic bone pain from metastatic prostate CA.
He was prescribed
Percocet (5/325) in the ER 2 weeks ago and is now in your clinic for f/u.
Pain is well ‐ controlled on current meds, but tends to recur ~ 1 hr before the next dose.
He is taking 2 Percocet every 4 hrs around the clock, even at night.
10mg oxycodone 6 times/day = 60mg oxycodone in 24 hrs
Equivalent SR Oxycodone = Oxycontin 30mg q12h
Add opioid rescue dose – 10% of 60mg = 6mg 20% of 60mg = 12mg
ANSWER: Oxycontin 30mg q12h with Oxycodone 5 ‐ 10 mg q4h prn
2.
Converting Short acting Æ Long acting (IR Æ SR) at a higher dose
*Use for: Chronic pain ‐ unrelieved/ partially relieved by IR meds
Instructions:
1.
Calculate how many mg of opioid pt is using in 24 hrs Æ convert to long acting opioid
2.
Increase long acting opioid by 50%
3.
Round up or down based on what pill form is available
4.
Adjust rescue dose – [10 ‐ 20% new daily dose]
1
Case 2: Same case as above – Mr.
Smith – Pain partially relieved (9/10 Æ 6/10) with 2 percocet q4 hrs round the clock
10mg oxycodone 6 times/day = 60mg oxycodone in 24 hrs
*Increase oxycodone by 50% [(60 mg + (60mg X50%)] = 60mg + 30 mg = 90 mg oxycodone/day
Oxycontin 45mg q 12hr – Check pill availability – would give Oxycontin 40mg q12h
Rescue dose: 10% 80mg = 8 mg 20% 80mg = 16mg
ANSWER: Oxycontin 40mg q12h with Oxycodone 10 ‐ 15mg q4h prn
3.
Using rescue doses to increase sustained ‐ release opioid
PP:
‐ Can safely escalate opioid dose in pt with constant pain after pt has been taking SR preparation for 24 ‐ 48 hrs
‐ Ask pt to record all rescue doses he takes
‐ If the total amount of drug taken as a rescue dose is more than 25% of the total SR dose, increase the SR dose by the amount in the rescue doses
Case 3: Mr.
Smith returns to clinic 2 weeks later.
He is taking Oxycontin 40mg q12h and Oxycodone 10mg q4h prn.
He reports that he is consistently taking 4 oxycodone/day for breakthrough pain.
Total oxycodone /day = 80mg (SR)+ 40mg (IR) = 120 mg oxycodone/day
New Oxycontin dose 60mg q12h
Rescue dose 10% of 120mg = 12mg 20% of 120mg = 24 mg
ANSWER: Oxycontin 60mg q12h with 15 ‐ 20 mg oxycodone q4h prn
2
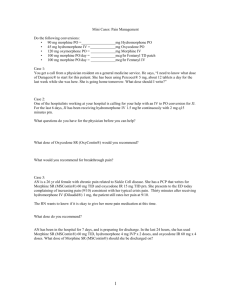
SMALL GROUPS
Ms.
X is a 60 – yo WF with chronic RA pain has failed all non ‐ opioid pain regimens.
You started her on
Morphine sulfate 15 mg IR q3h prn, which is controlling her pain and improving her function.
She takes the MS IR 8 times/day, around the clock.
You want to start her on a sustained release morphine preparation with immediate ‐ release morphine for breakthrough pain.
Ms.
Y is a 35 yo HF with a newly diagnosed soft tissue sarcoma that was resected 3 months ago.
She continues to have 8/10 pain despite taking oxycodone 20mg five times/day .
What dose of oxycontin and oxycodone IR do you want to start?
Mr.
Z is a 45 yo WM with a h/o multiple back surgeries, herniated discs, and spinal stenosis after a construction accident 6 years ago.
He is currently taking MS Contin 30mg q12h with MS IR 15mg q4h prn pain.
He reports pain is well controlled, with improved function and is back at work at a desk job.
He takes 4 MS IR tabs/day for breakthrough pain.
How would you adjust his MS Contin and MS IR?
CHANGING OPIOID AGENTS
Use for: Pt’s having intolerable side effects on one opioid; cost or delivery method may necessitate changing opioids
PP:
‐ There is incomplete cross ‐ tolerance between different opioids, but the exact amount will differ, thus, equianalgesic tables are only approximations.
‐ Depending on age, prior side effects, etc, most experts recommend starting a new opioid at ½ ‐ 2/3 of the calculated equianalgesic dose.
Instructions:
1.
Calculate the 24 hr current opioid dose
2.
Use the equianalgesic ratio to calculate new opioid dose
3.
Reduce dose by ½ ‐ 2/3 for cross tolerance – take individual patient into account
3
Mrs.
T is a 40 yo AAF with a h/o multiple myeloma whose chronic bone pain is well controlled on Oxycontin 80mg q12h with only an occasional Oxycodone 30mg q4h for breakthrough.
Her pharmacy is no longer carrying oxycontin because of recent break ‐ ins.
You want to convert her to MS Contin with MS IR for breakthrough.
Current 24 hr opioid dose = 160mg oxycodone/day
Po morphine = po oxycodone
160mg oxycodone = 160mg morphine
2/3 (160mg morphine) ~= 106 mg
New morphine dose (taking into account pill availability) = 45mg q12h MS Contin
Breakthrough dose – 10% 90mg = 9 mg, 20% 90mg = 18mg
ANSWER: 45mg MS Contin q12h with 15 mg MS IR q4h for breakthrough
Mr.
X is a 80yo WM with a h/o chronic abdominal pain after multiple abdominal surgeries for colon cancer.
His pain is well controlled on MS contin 100mg q12h with MS IR 20mg q2h prn (which he takes 5X/day).
He is admitted to the hospital with a new L MCA CVA with mild deficits.
He is having difficulty swallowing his pills and wants to try a Fentanyl patch.
What dose do you choose?
Total morphine/day = 200mg morphine (SR) + 100mg morphine (IR) = 300mg po morphine/day
25mcg/hr fentanyl patch = 1mg/hr IV morphine
25mcg/hr fentanyl patch = 75 mg po morphine/day
300mg po morphine/day X [25mcg/hr fentanyl patch] = 100mcg/hr fentanyl patch
[ 75 mg po morphine/day]
Reduce for cross tolerance ½ ( 100mcg/hr fentanyl patch) = 50mcg/hr fentanyl patch
Answer: 50 mcg/hr Fentanyl patch
Breakthrough with MS IR – can use same breakthrough dose as before (change form to liquid so pt can swallow)
Mr.
Z is a 55 yo AAM with intermittent pain in knees from OA.
He currently takes MS IR 30mg q4h prn which helps his pain.
However, he complains of “cloudy thinking” at this dose.
You try to decrease the dose, which improves the side effect, but does nothing for the pain.
You are considering opioid rotation with Dilaudid.
What is his new prescription?
4 ‐ 5 mg po morphine = 1mg po dilaudid
30mg po morphine X [1mg po dilaudid]= 6 mg po dilaudid
[5mg po morphine]
Reduce for cross ‐ tolerance 2/3 = 4mg po dilaudid
Answer: 4mg po dilaudid q4h prn
4
SMALL GROUPS:
Ms.
B is a 50 yo breast CA survivor with chronic neuropathic pain from her mastectomy.
She currently is well ‐ controlled on a 75mcg/hr fentanyl patch.
She lost her job and can no longer afford the patch.
You want to switch her to MS Contin with MS IR for breakthrough.
What dose?
Mr.
C is a 65 yo WM with severe emphysema with chronic back pain from OA and is taking Oxycontin
20mg q12h with oxycodone 5mg q4h prn (takes 4/day consistently), and is experiencing constipation despite a very good bowel regimen.
You want to rotate opioids.
What is the new prescription for MS
Contin with MS IR for breakthrough?
Methadone – don’t be afraid
PP: ‐ Methadone is a good drug ‐ cheap, effective, great for neuropathic pain
‐ Long acting, would wait 3 days before changing dose
‐ Pay attention to ratios
‐ When changing opioids, reduce by 50% for cross tolerance/ NMDA activity
Mr.
D is a 45 yo WM with a h/o prostate ca with bony mets.
He currently takes MS Contin 200mg q12h with MS IR
40mg q4h prn pain (which he takes 5 X /day).
His pain is well controlled on this medication, but he is starting to have periodic hallucinations.
You want to switch him to Methadone, what dose to you start with?
Total Morphine/day = 400mg (SR) + 200mg (IR) = 600mg morphine/day
10mg po morphine = 1mg po methadone
600mg po morphine/day X (1 mg po methadone) = 60mg po methadone/day
( 10mg po morphine)
Decrease by 50% for cross tolerance = 30mg po methadone/day = 10mg q8h
Answer: Methadone 10mg q8h
5
Mr X is a 80 yo AAM with metastatic lung CA with multiple bony lesions.
He is taking MS contin 900mg q12h with
MS IR for breakthrough.
He is extremely constipated on this dose despite an aggressive bowel regimen.
What dose of methadone would you prescribe?
900mg q12h = 1800mg po morphine/day
1800mg po morphine/day X (1 mg po methadone/day /20mg po morphine/day) = 90mg po methadone/day
Reduce by 50% for cross tolerance =45mg po methadone/day
Answer: 15mg po methadone q8h
Small Groups:
Ms.
Y is a 35 yo AAF with h/o breast CA.
She currently takes methadone 5mg q8h with morphine 30mg tabs q3h prn pain.
She comes to your clinic having run out of morphine for breakthrough pain.
Upon further questioning, she reports that her pain is manageable but only if she takes 2 morphine tabs
(60mg) every 4 hrs around the clock.
What should her new methadone dose be?
(Hint: convert her breakthrough morphine to methadone, then add that to her current dose)
Complicated /multiple opioid conversions
PP: Convert everything to morphine and go from there
Decrease for cross tolerance at the end
Ex.
Mr.
Y is a 60 yo WM who is admitted to your medicine team with cellulitis.
He has chronic pain from multiple back surgeries and is on a crazy pain regimen, that you would like to simplify.
He takes MS Contin 100mg q8h,
Percocet (5/325) 6 X/day, Dilaudid 4 mg (which he takes 4X/day), and is wearing a fentanyl patch 50mcg/hr.
What new pain regimen do you recommend?
Convert everything to morphine –
MS Contin 100mg q8h = 300mg morphine/day
Oxycodone 5mg X 6 doses= 30mg oxycodone/day = 30mg po morphine/day
Dilaudid 4mg X 4 = 16mg dilaudid/day = 80mg morphine/day
Fentanyl patch 50mcg/hr = 150mg morphine/day
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
TOTAL morphine equivalent/day = 560mg/day
Covert to methadone – 560mg morphine/day X (1mg po methadone/10mg po morphine) = 56mg methadone/day
Decrease for cross tolerance – 50% 56mg = 28mg po methadone/day
Answer: Methadone 10mg q8h + Dilaudid 8 mg po q4h prn pain
6
4.
CHANGING OPIOID ROUTE: same drug
Use for: po Æ IV : Pt who needs to be NPO; clinical situation that requires rapid titration
IV Æ po: calculating home dose of opioids/discharge planning
PP: If pt is on a long ‐ acting opioid – DO NOT just stop it if pt unable to take po,
start parenteral basal rate
Ex.
Ms.
T is a 60 yo WF with MM who is taking MS Contin 60mg q12h with an occasional MS IR for breakthrough.
She is admitted after a pathologic fracture of her humerus and is NPO for surgery.
What IV dose of morphine do you want to start her on ?
Calculate morphine in 24 hrs = 60mg q12h = 120mg po morphine/24 hrs
3mg po morphine = 1mg IV morphine
120mg po morphine X (1mg IV morphine/3mg po morphine) = 40mg IVmorphine in 24 hrs = 1.6mg/hr IV morphine
Mr.
M is a 55 yo WM on 20mg po methadone q8h for his chronic abdominal pain from a soft tissue sarcoma.
He is admitted with intractable N/V.
What do you do with his methadone?
2mg po methadone = 1mg IV methadone
Just change route – Answer: 10mg IV Methadone q8h
5.
CHANGING OPIOID ROUTE: different drug
PP: Same rules apply – use morphine to calculate equianalgesic dose; decrease new dose by ½ ‐ 2/3 for cross tolerance
Ex.
Mr.
A is a 66 yo AAM with chronic back pain from multiple surgeries.
He is on Oxycontin 120mg q12h with an occasional oxycodone for breakthrough.
He is admitted for a laminectomy.
You are the medicine consult for pre ‐ op and the surgical team wants to start a dilaudid PCA.
What basal would you recommend for when pt is NPO?
Oxycontin 120mg q12h = 240mg oxycodone/24 hrs = 240mg po morphine/24 hrs = 80mg IV morphine/24 hrs
80mg IV morphine/24 hrs X (1 mg IV dilaudid/ 5mg IV morphine) = 16mg IV dilaudid/24 hrs = 0.67
mg IV dilaudid/hr
Reduce for cross tolerance (2/3 X 0.67) = 0.4mg
IV dilaudid/hr
7
Small Groups:
Miss D is a 25 yo AAF with sickle cell anemia who comes to the ER in crisis.
She is dehydrated, complains of N/V X 2 days, and is unable to keep any food (or medication) down.
According to the pt and the Red
Book, she usually takes 90 MS IR q1hr prn for a typical crisis.
You would like to give her IV dilaudid prn.
What dose to you choose?
Ms.
P is a 54 yo WF with breast ca with progressive bony mets.
She is admitted to N4N for pain control and is placed on a dilaudid PCA to see how much opioid she requires.
After looking at the pump history, she has required 60mg IV dilaudid in the last 24 hrs.
You would like to start methadone, what dose do you choose?
8
Morphine Sulfate IR
Morphine Sulfate ER
(MS Contin)
Oxycodone IR
Oxycondone SR
(Oxycontin)
Dilaudid
(hydromorphone)
Fentanyl patch
Methadone
15 mg,
15mg,
5
10mg,
2
12
5 mg mg
,
30
30mg,
20mg,
4mg, mcg/hr, mg, mg
10mg,
8
25
60mg,
40mg,
tabs; mg
10mg/ml,
100mg,
80mg, mcg/hr,
40mg,
20mg/ml
200mg
160mg
50mcg/hr,
10mg/5ml
75 tabs
solution
mcg/hr, solution,
RATIOS morphine PO = oxycodone PO
1mg IV morphine = 3 mg PO morphine
1mg/hr IV morphine (= 72mg po morphine/day) = 25 mcg/hr Fentanyl patch
1mg IV morphine = 10 mcg IV fentanyl
100mcg fentanyl lollipop = 1mg IV morphine
5 mg po morphine = 1mg po dilaudid
5mg IV morphine = 1mg IV dilaudid
1 mg IV dilaudid = 4 ‐ 5 mg po dilaudid
10mg PO morphine = 1mg PO methadone (average)
20 mg po morphine = 1 mg po methadone (when >1000mg MS in 24 hrs)
IV = SQ (morphine and dilaudid)
100mg IV morphine = 10mg epidural morphine = 1mg intrathecal morphine
100mcg/hr
5mg/5ml
solution
9