Long-term Outcome of Keratolimbal Allograft with or without
advertisement

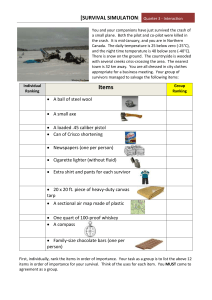
Long-term Outcome of Keratolimbal Allograft with or without Penetrating Keratoplasty for Total Limbal Stem Cell Deficiency Abraham Solomon, MD,1 Pierre Ellies, MD,1 David F. Anderson, FRCOphth,1 Amel Touhami, MD,1 Martin Grueterich, MD,1 Edgar M. Espana, MD,1 Seng-Ei Ti, MD,1 Eiki Goto, MD,1 William J. Feuer, MS,1,2 Scheffer C. G. Tseng, MD, PhD1,3 Purpose: To evaluate the long-term outcome of ocular surface reconstruction, including keratolimbal allograft (KLAL) and amniotic membrane transplantation (AMT) with or without penetrating keratoplasty (PKP), in patients with nonambulatory vision secondary to total limbal stem cell deficiency (LSCD). Design: Retrospective, noncomparative interventional case series. Participants: Thirty-nine eyes in 31 consecutive patients with total LSCD, as defined by impression cytology, who had a preoperative best-corrected visual acuity of less than 20/200 and a minimum follow-up of 12 months. Patients were divided into three groups: group 1 (16 eyes) with chemical burns, group 2 (9 eyes) with Stevens-Johnson syndrome (SJS), and group 3 (14 eyes) with other causes of LSCD, including ocular cicatricial pemphigoid, atopic keratoconjunctivitis, and aniridia. Intervention: All patients underwent KLAL and AMT by one surgeon (SCGT). If needed, PKP was performed at the same surgical setting using tissue from the same donor. Main Outcome Measures: Cumulative rates of survival of ambulatory vision (ⱖ 20/200), survival of KLAL, survival of PKP, and incidence of complications. Results: Fifty-three KLAL with AMT procedures were performed in 39 eyes, of which 23 eyes received simultaneous PKP at the time of the first KLAL. The mean follow-up was 34.0 ⫾ 21.5 months (range, 12–117.6). The mean period of ambulatory vision was 23.9 ⫾ 20.9 months (range, 0 –104). The overall survival of ambulatory vision was 53.6% at 3 years and 44.6% at 5 years. The survival of ambulatory vision was significantly worse in SJS compared with other causes (67%, 81%, and 92% for groups 1, 2, and 3, respectively; P ⫽ 0.06 for group 1 versus 2, P ⫽ 0.0008 for group 1 versus 3). KLAL performed alone resulted in higher survival of ambulatory vision at 2 years (86.1% ⫾ 9.1%) compared with KLAL with PKP (46.9% ⫾ 10.6%, P ⫽ 0.100). The survival of PKP was significantly worse in SJS compared with the other causes (20.0% ⫾ 17.9% compared with 55.6% ⫾ 11.7%, respectively, P ⫽ 0.028). After 2 years, the survival of the second KLAL was better than that of the first: 68.2% ⫾ 15.4% compared with 27.3% ⫾ 13.4%, respectively (P ⫽ 0.041). Conclusions: Ambulatory vision for a period of more than 2 years can be achieved by KLAL with or without PKP in eyes with severe ocular surface disorders caused by total LSCD. However, a progressive decline of the visual outcome and graft survival is evident with time. Performing PKP simultaneously with KLAL may be associated with a less favorable outcome. The failure of KLAL is associated with the loss of donor cells in the recipient. Augmentation of ocular surface defense is essential in securing the success of KLAL and PKP. Future modifications of the surgical procedure and of the immune suppressive protocols may improve survival of the allogeneic grafts and the final visual outcome. Ophthalmology 2002;109:1159 –1166 © 2002 by the American Academy of Ophthalmology. Originally received: June 27, 2001. Accepted: August 28, 2001. Manuscript no. 210446. 1 Department of Ophthalmology, Bascom Palmer Eye Institute, Miami, Florida. 2 Department of Biostatistics, Bascom Palmer Eye Institute, Miami, Florida. 3 Department of Cell Biology & Anatomy, University of Miami School of Medicine, Miami, Florida. Supported in part by an unrestricted grant from Research to Prevent © 2002 by the American Academy of Ophthalmology Published by Elsevier Science Inc. Blindness, Inc., New York, New York, la Banque Française des yeux, Paris, France (PE), the T.F.C. Frost Charitable Trust, London, England (DFA), and the Deutsche Forschungsgemeinschaft, Bonn, Germany (MG) (GR1814/1-1). SCGT has obtained a patent on preparation and clinical uses of the amniotic membrane. Reprint requests to Scheffer C. G. Tseng, MD, PhD, Ocular Surface Center, 8780 SW 92 Street, Suite 203, Miami, FL 33176. ISSN 0161-6420/02/$–see front matter PII S0161-6420(02)00960-0 1159 Ophthalmology Volume 109, Number 6, June 2002 Stem cells of the corneal epithelium are located at the limbus1 and are ultimately responsible for renewal and regeneration of the entire corneal epithelium under normal circumstances and during wound healing.2,3 Diseases causing either a complete loss of limbal epithelial stem cells or severe destruction of the limbal stroma result in the pathologic state of total limbal stem cell deficiency (LSCD).4 Patients with total LSCD invariably complain of pain and photophobia and have severe loss of vision caused by the invading vascularized conjunctiva. Because the life span of corneal epithelial progenitor cells from a corneal graft is limited, total LSCD cannot be treated by penetrating keratoplasty (PKP) alone, and visual rehabilitation depends on transplantation of limbal epithelial stem cells.5,6 When total LSCD involves only one eye, successful reconstruction can be achieved by transplanting autologous limbal epithelial stem cells from the fellow eye in a procedure termed “limbal conjunctival autograft.”7–11 However, when total LSCD involves both eyes, corneal surface reconstruction relies on transplantation of an allogeneic source of limbal epithelial stem cells. This can be achieved by limbal conjunctival allograft from living-related donors12,13 or keratolimbal allograft (KLAL) from cadaveric donors.12,14 –16 Because the source of limbal epithelial stem cells is allogeneic, the survival of the graft depends on systemic immunosuppression. Despite the continuous administration of systemic cyclosporin A, the success rate of KLAL declines from 75% to 80%14 –16 after 1 year to 50%17 after 3 years of follow-up. This finding strongly suggests that there are unknown clinical variables that affect the outcome of KLAL, and underscores the importance of identifying and measuring these variables in a long-term study. A major variable that may complicate the outcome analysis of KLAL is additional PKP that is needed to restore corneal transparency when LSCD is accompanied by deep corneal scarring.12,17–20 The conventional method of grouping KLAL failure and PKP failure together as a single end point analysis may not disclose the true survival of KLAL or PKP. Other important variables include the heterogeneous nature of the underlying cause, the varying degrees of LSCD severity, and different extents of dysfunctional external adnexae, which may independently affect the outcome of KLAL. In an attempt to address these potential variables, we present herein the long-term outcome of KLAL in patients with nonambulatory vision secondary to total LSCD by evaluating the survival of KLAL and PKP separately and according to the underlying ocular surface disease. Furthermore, the visual outcome is measured not by mean preoperative and final visual acuity, as previously reported,12,17–20 but by the period of ambulatory vision achieved in a manner similar to that reported by Dohlman and Terada21 for evaluating the visual outcome in the use of keratoprosthesis. The contribution of other variables relating to the dysfunctional ocular surface defenses in affecting such outcome is analyzed as well. 1160 Materials and Methods Patients This study was approved by the Medical Science Subcommittee for the Protection of Human Subjects in Research of the University of Miami School of Medicine, Miami, Florida. Each patient gave written informed consent after explanation of the nature, risks, and possible adverse consequences of the procedure. One surgeon (SCGT) performed all surgeries at one center (i.e., the Bascom Palmer Eye Institute). The entry criteria for the study were patients with total LSCD who underwent KLAL and amniotic membrane transplantation (AMT), had a best-corrected visual acuity (BCVA) of less than 20/200, and had been followed up for at least 12 months postoperatively. On the basis of these criteria, 53 KLAL procedures were performed on 39 eyes of 31 patients (21 males, 10 females) between January 1991 and January 1999. The last follow-up visits for all patients, for the purpose of data analysis, took place between January and April 2001. Diagnosis of LSCD was made clinically and was confirmed in 28 of 39 eyes by impression cytology showing goblet cells on the corneal surface, as previously reported.18,22 In the remaining 11 eyes, the diagnosis of LSCD was clinically evident as shown by late fluorescein staining, loss of limbal palisade of Vogt, superficial vascularization, signs of complete conjunctivalization, or keratinization of the cornea, and impression cytology was thus not considered necessary. These 39 eyes were further divided into three groups according to the underlying causes. Group 1 included patients with chemical burns (16 eyes), group 2 had patients with Stevens-Johnson syndrome (9 eyes), and group 3 included all other causes such as ocular cicatricial pemphigoid (2 eyes), atopic keratoconjunctivitis (3 eyes), contact lens-induced keratopathy (2 eyes), herpes simplex virus keratitis (1 eye), multiple surgeries (1 eye), aniridia (1 eye), and idiopathic causes (4 eyes). Data were gathered by retrospective review of the medical and operative records. Previous surgeries before referral to Bascom Palmer Eye Institute were also considered and included PKP, KLAL, anterior segment reconstruction, lid surgery, and glaucoma surgery. Other procedures performed during this study were recorded and included punctal occlusion, filtering surgery, lid reconstruction, and tarsorrhaphy to restore the healthy ocular surface defense. Transplantation of Limbal Epithelial Stem Cells All surgeries were performed with the patient under local anesthesia. Transplantation of allogeneic limbal epithelial stem cells by means of KLAL was performed as previously described.18 Scarred and inflamed tissue was removed by superficial keratectomy in the entire limbal and corneal surfaces. Amniotic membrane provided by Bio-Tissue (Miami, FL) was used as a graft to reduce inflammation and scarring in the underlying stroma and to prepare the stromal bed for stem cell transplantation. For all cases, a 360° corneolimbal ring graft was prepared from a remaining corneoscleral ring after a conventional 8.0-mm trephination of a cadaveric donor button stored in a modified MK medium without human leukocyte antigen matching. This donor corneolimbal ring was thinned from the endothelial aspect by dissection with sharp Westcott scissors. It was then secured to the surrounding conjunctival edge with 9-0 or 10-0 interrupted Vicryl sutures with episcleral bites and, if necessary, to the denuded corneal surface with a running 10-0 nylon suture. When PKP was needed, it would be performed first and immediately followed by KLAL at the same surgical setting using the same donor. The central corneal donor button was first secured to the host tissue with eight interrupted 10-0 nylon sutures. The donor corneolimbal rim was then transferred to the recipient eye to fit exactly with the outside border of Solomon et al 䡠 Keratolimbal Allografts for Stem Cell Deficiency the secured central corneal button. The KLAL was then secured to the surrounding conjunctival edge in the same manner as that described previously and to the donor corneal button using a second set of eight interrupted 10-0 nylon sutures, which were passed to include portions of donor corneal button, recipient peripheral cornea, and donor ring graft. Maxitrol (neomycin, polymyxin B, and dexamethasone) ointment (Alcon Laboratories, Inc., Fort Worth, TX) was applied at the end of the procedure. Postoperatively, all patients received nonpreserved 1% methylprednisolone eye drops (Bascom Palmer Eye Institute Pharmacy) every 2 hours while awake and 0.3% ofloxacin (Allergan, Irvine, CA) three times a day, of which the former was tapered to a maintenance dose over 1 month and the latter was discontinued when epithelialization was completed. Sutures were removed at 3 to 6 weeks. All patients received oral cyclosporin A at a dosage of 5 mg/kg body weight a day in divided doses starting at 1 week before or at the time of KLAL. Cyclosporin A was then tapered to 1 to 2 mg/kg in 4 to 8 weeks, so that the trough blood level was maintained at 100 to 150 ng/ml, and administered indefinitely. Renal and liver function tests were monitored at appropriate intervals. Patients with aqueous tear deficiency were treated with preservative-free Refresh Plus (Allergan, Irvine, CA) lubricants or autologous serum drops. Punctal occlusion by cauterization had been performed in both upper and lower lids if there was severe aqueous tear deficiency or a neurotrophic state as diagnosed by the Cochet-Bonnet esthesiometer (Luneau, Paris, France).23 Clinical Evaluation of Main Outcome Measures Maintenance of Ambulatory Visual Acuity. The BCVA was measured at each clinical visit. Nonambulatory vision was defined as a BCVA ⬍ 20/200, whereas ambulatory vision was defined as a BCVA ⱖ 20/200. For each eye the postoperative time period during which ambulatory vision was continuously maintained was recorded, following a method described by Dohlman and Terada21 for the postoperative evaluation in patients with keratoprosthesis. When the BCVA deteriorated to the level below the cut-off point of 20/200, the eye was considered as a failure for the purpose of survival analysis. Survival of KLAL. Survival of transplanted limbal epithelial stem cells was defined by the duration of maintaining a normal corneal epithelial phenotype after surgery. Failure of the KLAL and subsequent recurrent LSCD was defined as the appearance of diffuse late fluorescein staining, conjunctivalization, vascularization of the cornea through the limbus, or persistent epithelial defects with diffuse persistent irregular epithelium after correction of lid malposition, trichiasis, symblepharon, and dry eye. In addition to slit-lamp examination, impression cytology was performed when necessary to confirm the presence of conjunctival goblet cells on the corneal surface. Failure of KLAL was also diagnosed when there were clear signs of rejection (congestion of the perilimbal and limbal blood vessels and swelling of the tissue, as previously described),14 but was also diagnosed in cases in which rejection could not be detected. Survival of the Central Corneal Graft (PKP). Survival of corneal allograft was defined conventionally by maintenance of a clear and compact corneal tissue that allowed a clear view of underlying iris detail. Corneal allograft failure was diagnosed by classic signs of endothelial or epithelial rejection lines and subepithelial infiltrates, keratic precipitates, stromal edema, and corneal opacification. Complications All postoperative complications were carefully recorded. Raised intraocular pressure was considered a complication when glau- coma had not been diagnosed before surgery. Corneal epithelial defects were considered to be persistent when they were observed for more than 2 weeks. Persistent epithelial defects were treated by artificial tear supplementation, punctual occlusion, autologous serum drops, lid reconstruction, amniotic membrane transplantation, and tarsorrhaphy. When persistent epithelial defects remained despite these treatments, they were considered a complication. Statistical Analysis The data were analyzed with the assistance of the Biostatistics Department at Bascom Palmer Eye Institute. Kaplan-Meier survival analysis was performed to evaluate three outcome measures: the cumulative incidence of maintaining ambulatory vision, KLAL survival, and PKP survival. The effect of several clinical parameters (such as cause, concomitant PKP, first versus second procedure, preoperative procedures, lid surgery during the follow-up period, symblepharon, and postoperative secondary glaucoma) on the survival of the three outcome measures was evaluated by univariate survival analysis and by Cox proportional hazards survival regression. The log-rank test was used to compare univariate survival curves. SPSS version 7.5 (SPSS Inc., Chicago, IL) was used for data analysis. Results Fifty-three KLAL procedures were performed on 39 eyes of 31 patients. The mean age of the patients was 40.1 ⫾ 14.6 years. The mean follow-up period was 34.0 ⫾ 21.5 months (range, 12–117.6). Twenty-eight of 39 eyes (74.4%) underwent one KLAL transplantation, 9 eyes had two KLAL procedures, one eye had 3, and another eye had 4 KLAL procedures (Table 1). Twenty-four eyes underwent a total of 45 PKP procedures. The first PKP procedure was performed simultaneously with a KLAL procedure, using the same donor. Twelve of 24 eyes (50.0%) underwent one PKP, and 11 eyes had 2 to 4 PKPs. Table 1 shows the number of surgical procedures according to the cause of LSCD. Survival of Ambulatory Vision The overall mean period of ambulatory vision was 23.9 ⫾ 20.9 months (range, 0 –104 months). Eyes that sustained chemical burns (group 1) had ambulatory vision for a mean period of 32.4 ⫾ 27.9 months, whereas eyes with Stevens-Johnson syndrome (SJS) and other causes (groups 2 and 3) had considerably shorter mean ambulatory vision periods of 15.2 ⫾ 12.4 months and 19.9 ⫾ 11.5 months, respectively (Fig 1A). The mean period of ambulatory vision for eyes with SJS was significantly shorter than that for eyes with chemical burns (P ⫽ 0.046). Survival analysis of the overall change of ambulatory vision with time showed a progressive decline of the cumulative proportion of eyes enjoying BCVA of 20/200 or better (Fig 1B). After 1 year of follow-up, 76.6% ⫾ 6.8% of eyes had ambulatory vision. This proportion further declined to 53.6% ⫾ 9.9% at 3 years, and to 44.6% ⫾ 11.6% at 5 years. The cause of limbal deficiency was found to have a significant effect on the final visual outcome. SJS had the lowest cumulative proportion of eyes with ambulatory vision after 2 years of follow-up compared with the other two groups (Fig 1C): 29.6% ⫾ 16.4% (SJS) compared with 62.5% ⫾ 1.2% (chemical burn, P ⫽ 0.067) and 92.3% ⫾ 7.4% (others, P ⫽ 0.00008). Performing PKP concomitantly with KLAL, during the first KLAL procedure, was found to decrease the visual outcome compared with performing KLAL alone (Fig 1D). Only 46.9% ⫾ 1161 Ophthalmology Volume 109, Number 6, June 2002 Table 1. Number of Eyes and of Surgical Procedures (Keratolimbal Allograft and Penetrating Keratoplasty) According to the Three Etiology Groups Procedures Total eyes with KLAL Eyes with 1 KLAL Eyes with 2 KLAL Eyes with 3 KLAL Eyes with 4 KLAL Total KLAL procedures Total eyes with additional PKP Eyes with 1 PKP Eyes with 2 PKP Eyes with 3 PKP Eyes with 4 PKP Total PKP procedures Group 1: Chemical Burns 16 11 4 1 23 15 8 3 1 3 29 Group 2: StevensJohnson Syndrome Group 3: Other Causes 9 7 1 1 14 10 4 12 5 2 1 2 18 4 2 2 10 6 Total 39 28 9 1 1 53 24 12 6 3 3 45 KLAL ⫽ keratolimbal allograft; PKP ⫽ penetrating keratoplasty. 10.6% of eyes that had undergone KLAL and PKP had ambulatory vision at 2 years compared with 86.1% ⫾ 9.1% for eyes that had KLAL alone (P ⫽ 0.10). However, after 3 years, no difference in ambulatory vision survival was noted between eyes that had simultaneous KLAL and PKP (43.1% ⫾ 30.8%) and eyes that had KLAL alone (39.1% ⫾ 11.4%). Cox proportional hazard survival regression analysis revealed that the most significant variables associated with reduced survival of the ambulatory vision were SJS (P ⫽ 0.047), younger age (P ⫽ 0.041), and performing PKP simultaneously with KLAL (P ⫽ 0.058). Other variables such as preoperative glaucoma, the number of previous surgical procedures, the presence of symblepharon, or lid surgery performed during the follow-up period did not have an effect on the visual outcome in the multivariate regression analysis. Survival of KLAL A progressive attrition in the survival of KLAL was noted during more than 5 years of follow-up (Fig 2A). The survival of KLAL was 76.9% ⫾ 6.7% at 1 year, 47.4% ⫾ 11.7% at 3 years, and only 23.7% ⫾ 17.7% at 5 years. This trend seemed to parallel the decline of ambulatory vision over the follow-up period. No differences in KLAL survival were noted between the three groups (Fig 2B). Univariate analysis did not demonstrate any effect for the number of previous procedures, previous glaucoma, presence of symblepharon, or lid surgery on KLAL survival. Although not significantly different, performing PKP with KLAL at the same session was associated with a markedly reduced KLAL survival after 2 years (Fig 2C, 81.2% ⫾ 9.8% when KLAL was performed alone compared with 58.9% ⫾ 10.6% when KLAL was performed with PKP, a decrease of 27.5%; P ⫽ 0.17). In 11 eyes, a second KLAL was performed after failure of the first KLAL. Comparison of the survival curves of the second with the first KLAL in these 11 eyes demonstrated a significantly higher survival for the second graft (Fig 2D). The survival of the second KLAL after 2 years was 68.2% ⫾ 15.4% compared with 27.3% ⫾ 13.4% for the first KLAL (P ⫽ 0.041). Survival of PKP An overall progressive decline in central corneal graft survival was observed from 47.8% ⫾ 10.4% after the first year to 13.7% ⫾ 1162 8.4% after 3 years (Fig 3A). As in KLAL, eyes with SJS had a significantly shorter survival compared with the other two groups (Fig 3B). After 1 year, the cumulative survival of eyes with SJS was 20.0% ⫾ 17.9% compared with 55.6% ⫾ 11.7% for the other two groups, whereas after 2 years of follow-up, none of the SJS central grafts had survived compared with 42.3% ⫾ 12.1% in the other groups (P ⫽ 0.028). Univariate survival analysis demonstrated a significant effect for the need to perform a lid surgery during the follow-up period. In eyes that required lid surgery to correct entropion, lid margin keratinization, or exposure, a significantly shorter survival of the central corneal graft was demonstrated compared with eyes in which no such surgery was needed (P ⫽ 0.034) (Fig 3C). Other parameters such as previous surgical procedures, previous glaucoma, and presence of symblepharon were not found to have an effect on central corneal graft survival. In addition, no difference was found between the survival of the first PKP compared with the second PKP in the 12 eyes that had undergone more than one PKP (Fig 3D). Complications Ten of 39 eyes (25.6%) developed elevated intraocular pressure after surgery. Eight of these 10 eyes (80.0%) had undergone one to three PKPs, which is a known risk factor for developing an elevated pressure. Nine of the 10 eyes required a glaucoma filtering procedure (a Baerveldt implant) to control the intraocular pressure. Fourteen eyes (35.9%) developed persistent epithelial defects. All defects except one healed by punctual occlusion (8 eyes), lid surgeries (10 eyes), and an amniotic membrane transplantation as a patch (9 eyes). The only one eye with refractory persistent epithelial defect as a complication had SJS with severe dry eye. Three eyes developed microbial keratitis. Two corneal grafts were severely infected by Candida species, which led to a central corneal graft failure and to a repeat penetrating keratoplasty. Both of these two infected grafts were also associated with secondary severe tractional retinal detachment. One eye infection had coagulase negative Staphylococcus in a loose suture, which was successfully treated with topical 0.3% ofloxacin. One eye with successful corneal surface reconstruction developed postoperative cystoid macular edema. Three eyes with severe chemical burns developed tractional retinal detachment as a result Figure 1. Analysis of the survival of ambulatory vision. A, Mean time periods of maintaining ambulatory vision in the three etiology groups. B, Kaplan-Meier survival curve of ambulatory vision in all 39 eyes. A progressive decline is evident with time. C, Survival of ambulatory vision according to different causes. Eyes with Stevens-Johnson syndrome had a significantly lower survival of ambulatory vision compared with the other two groups. D, Survival of ambulatory vision according to the inclusion of penetrating keratoplasty (PKP) with the first keratolimbal allograft (KLAL). Performing KLAL with PKP was associated with reduced survival of ambulatory vision during the first 2 years. Tables show cumulative percentages ⫾ standard deviation of eyes that maintained ambulatory vision. Figure 2. Analysis of variables affecting the survival of keratolimbal allograft (KLAL). A, Kaplan-Meier survival curve of KLAL in all 39 eyes. A progressive decline is evident with time. B, No differences were found between the effects of different causes on KLAL survival. C, Survival of KLAL according to the inclusion of penetrating keratoplasty (PKP) with the first KLAL. Performing KLAL with PKP was associated with a marked, although not significant, reduction in KLAL survival. D, Survival of the second KLAL was found to be significantly better than that of the first KLAL. Tables show cumulative percentages ⫾ standard deviation of eyes that had KLAL survival. Ophthalmology Volume 109, Number 6, June 2002 of deep penetration of the chemical into the posterior pole, leading to vitreitis and proliferative vitreoretinopathy. Discussion Reconstruction of the ocular surface in eyes with severe LSCD remains one of the most challenging problems in ophthalmology. It takes a set of preoperative measures to prepare the ocular surface defense mechanisms for surgery, requires demanding surgical procedures of KLAL and AMT with or without PKP, and involves a prolonged postoperative management that includes immunosuppression and continuous care for the maintenance of the ocular surface health (for reviews see references 2, 3, 5, and 12). Because this field is still evolving, little is known about the long-term outcome of these patients. Except for the recent study by Tsubota et al,17 there have been only a few reports on a relatively small number of patients with limited followup.13,14,16,19,20,24 In this study we present the long-term outcome of eyes with total LSCD, for whom a mean follow-up of 34 months was available, extending in some cases to 5 years. Using three objective measures to characterize the functional and anatomic outcome, namely the period of ambulatory vision, KLAL survival, and PKP survival, we demonstrated an overall trend of progressive decline of vision and attrition of these two allografts. Survival analysis demonstrated that 53.6% and 44.6% of eyes maintained visual acuity equal to or better than 20/200 after 3 and 5 years, respectively. The cumulative percentage of graft survival 3 years after surgery was 47.4% for KLAL and 13.7% for PKP. Of the three outcome measures, the main factor that might determine the final outcome of these eyes is probably KLAL survival, because failure of the transplanted limbal stem cells to survive will invariably result in invasion of conjunctival epithelium and blood vessels into the central corneal graft, thereby impairing its clarity. The prognosis for a successful KLAL may thus be strongly influenced by preoperative conditions such as tear function and functional external ocular adnexae. Postoperatively, attrition of KLAL survival is probably related to persistent inflammation, severe dry eye, or asymptomatic and progressive rejection of the KLAL. Shimazaki et al25 have recently reported that tear function affected surgical outcome of KLAL and amniotic membrane transplantation in patients with SJS. Previous reports with a shorter follow-up of 1 or 2 years revealed more favorable results of 70% to 80% success,12,15,16,18,24 a finding that was also noted in our data for the first 2 years of follow-up. Rao et al26 have also recently noticed gradual peripheral vascularization in seven of nine eyes, graft rejection in three eyes, and ambulatory vision in only two eyes after a short follow-up of 17 months. In Holland’s series,12 Figure 3. Analysis of variables affecting the survival of penetrating keratoplasty (PKP). A, Kaplan-Meier survival curve of 24 eyes that had PKP with the first keratolimbal allograft (KLAL) procedure. A progressive decline is evident with time. B, Stevens-Johnson syndrome had a signif- 1164 Š icantly lower PKP survival compared with the other causes. C, eyes that required lid surgery had a better PKP survival compared with eyes in which lid surgery was not performed. D, No differences were found between the survival of the first and the second PKP. Solomon et al 䡠 Keratolimbal Allografts for Stem Cell Deficiency 72% of eyes had a stable ocular surface, and 60% had a significant improvement in visual acuity. In our previous report,18 we observed corneal graft rejection in 9 of 14 (64%) eyes and limbal allograft rejection in 3 of 21 eyes (14%). The fact that the success rate declines with time, a finding consistent with that reported by Tsubota et al,17 further underscores the importance of long-term follow-up in the investigation of a graft survival. Recent laboratory data provide conflicting evidence concerning the survival of transplanted limbal epithelial stem cells in patients receiving KLAL. Using primers that detect variable nucleotide tandem repeats, the genotype of surface epithelial cells from recipients of KLAL was compared with that of scleral samples from remnant donor eyes.27 The authors noted that in none of the eyes examined were donor cells recovered from the recipient’s surface 3 to 5 years after KLAL. A recent immunohistologic study of specimens from corneas after KLAL rejection could not demonstrate any epithelium with a corneal phenotype.28 In a rabbit study of KLAL, none of the recipient corneas regained a normal corneal surface within the first 5 months after surgery.29 On the contrary, Shimazaki et al30 detected donor-derived epithelial cells in the paracentral cornea of eyes after KLAL using fluorescein in situ hybridization probes and restriction fragment length polymorphism analysis. We suspect that the failure of KLAL is associated with the loss of donor cells in the recipient. Further studies comparing the genotyping of donor and recipient epithelial cells in KLAL transplanted eyes at different time points after the surgery are needed to evaluate the true survival of donor-derived cells with time. In this study, eyes with SJS were found to have the least favorable visual outcome (29.6% survival of ambulatory vision at 2 years) and the lowest survival of the central corneal graft (no surviving grafts at 2 years). SJS is characterized by persistent inflammation coupled with progressive fibrosis, leading to tear film abnormalities and lid malposition, all of which contribute to progressive attrition of corneal epithelial cells and progressive exhaustion of the stem cell population. By use of a similar surgical approach, a successful outcome of ocular surface reconstruction was recorded in 13 of 29 (44.8%) eyes in adult patients with SJS25 and in 2 of 4 children.20 However, the success in these series was determined by sustained coverage of the corneal surface by the corneal epithelium, whereas only 9 of 29 (31.0%) eyes achieved a postoperative visual acuity equal to or better than 20/200.25 When PKP was performed at the same session with KLAL, we noted a marked reduction in the ambulatory vision during the first 2 postoperative years, along with a marked reduction in KLAL survival. Moreover, a progressive decline of PKP survival with time was evident, to the point at which none of the grafts survived after 5 years follow-up. Likewise, Shimazaki et al31 reported that 16 of 45 (35.6%) eyes receiving simultaneous PKP and KLAL developed an endothelial rejection of the central corneal graft and that, subsequently, 10 of these 16 eyes developed endothelial decompensation. The poor prognosis of central corneal graft survival may be partially explained by the increased exposure of the host immune system to the donor corneal antigens through the recognition of limbal allograft antigens, which come from the same donor as the central corneal graft. Moreover, the addition of PKP at the same setting might have increased the wound healing response and inflammation, which are deleterious to stem cell health. For these reasons, some physicians have advocated waiting for at least 3 months after KLAL before performing PKP.32 We have since modified our surgical strategy and adopted a two-step approach by performing KLAL first, followed by a PKP 3 to 6 months later. Interestingly, the second KLAL survival rate was 2.5fold greater than that of the first KLAL. Although no data are yet available on the longevity of repeat KLAL, our observation contradicts the conventional knowledge on the survival of corneal regrafts, in which the survival of repeated PKP significantly decreases with the increasing number of regrafting procedures.33 We speculate that postoperative measures to improve the ocular surface defense may have facilitated a better prognosis for the second KLAL. Furthermore, both the surgeon’s learning curve in KLAL and performing the second KLAL without a simultaneous PKP may have also increased the survival of second KLAL. Systemic cyclosporin A was used for immunosuppression throughout the study period. Systemic immunosuppression is probably needed for an indefinite time when the transplanted tissue is allogeneic. Because the rate of graft survival seemed to be unacceptably low, we have decided to modify our protocol to include systemic corticosteroids and mycophenolate mofetil (CellCept, Hoffmann La Roche, Nutley, NJ), starting 1 month before surgery and tapering down the corticosteroids during the first postoperative months while adjusting cyclosporin A and mycophenolate dosages to a level that can be tolerated by the patient. Although long-term data are not available, our preliminary impression is that this modified protocol might improve the overall success, because the graft tissues and the eyes seem to be more quiescent. Ocular surface reconstruction for severe diseases such as SJS, ocular cicatricial pemphigoid, and chemical burns continues to be one of the most challenging fields in ophthalmology. Our study provides new information regarding the long-term survival of vision and transplanted tissue in this set of complicated cases. On the basis of the results of this study, we have considerably modified our surgical technique and postoperative management. We no longer perform PKP at the same session with KLAL, and prefer to wait at least 3 months or until the surface inflammation is diminished. We use the amniotic membrane in all of our KLAL procedures, first as a graft on which the corneoscleral rim is sutured and then as a patch over the surface at the end of the procedure. We emphasize the need for indefinite immunosuppression in all of our patients after allogeneic transplants while meticulously monitoring any possible side effects. Because the overall success rate of such ocular surface reconstruction remains low, we continue our search for other strategies. Performing KLAL with tissue from human leukocyte antigen-matched live related donors may improve the longevity of KLAL.13,26 The ability to expand the limbal epithelial stem cells in an ex-vivo environment 1165 Ophthalmology Volume 109, Number 6, June 2002 on the amniotic membrane as a carrier34 –36 may prove to be an alternative to the current KLAL procedure. Tissue engineering that includes an artificial stroma made from synthetic polymers, with or without epithelial and endothelial cells, may prove to be another future avenue for surface reconstruction.37 Keratoprosthesis is yet another alternative for patients in whom the ocular surface is severely keratinized and dry, and the chances for graft failure are high.21 Some or all of these alternatives may be available in the future for patients with ocular surface diseases, and we may be able to choose or tailor the appropriate treatment for each of our patients according to the underlying disease and the severity of deficiency in ocular surface defense and LSCD. References 1. Schermer A, Galvin S, Sun TT. Differentiation-related expression of a major 64K corneal keratin in vivo and in culture suggests limbal location of corneal epithelial stem cells. J Cell Biol 1986;103:49 – 62. 2. Tseng SCG. Regulation and clinical implications of corneal epithelial stem cells. Mol Biol Rep 1996;23:47–58. 3. Tseng SCG, Sun TT. Stem cells: ocular surface maintenance. In: Brightbill FS, ed. Corneal Surgery: Theory, Technique, and Tissue. St. Louis: Mosby, 1999; chap. 2. 4. Puangsricharern V, Tseng SCG. Cytologic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology 1995;102:1476 – 85. 5. Holland EJ, Schwartz GS. The evolution of epithelial transplantation for severe ocular surface disease and a proposed classification system. Cornea 1996;15:549 –56. 6. Tseng SCG. Conjunctival grafting for corneal diseases. In: Tasman W, Jaeger EA, eds. Duane’s Clinical Ophthalmology. Philadelphia: JB Lippincott, 1994; chap. 34. 7. Kenyon KR, Tseng SCG. Limbal autograft transplantation for ocular surface disorders. Ophthalmology 1989;96:709 –23. 8. Jenkins C, Tuft S, Liu C, Buckley R. Limbal transplantation in the management of chronic contact-lens–associated epitheliopathy. Eye 1993;7:629 –33. 9. Morgan S, Murray A. Limbal autotransplantation in the acute and chronic phases of severe chemical injuries. Eye 1996;10:349 –54. 10. Moldovan SM, Borderie V, Baudrimont M, Laroche L. Treatment of unilateral limbal stem cell deficiency syndrome by limbal autograft. J Fr Ophtalmol 1999;22:302–9. 11. Rao SK, Rajagopal R, Sitalakshmi G, Padmanabhan P. Limbal autografting: comparison of results in the acute and chronic phases of ocular surface burns. Cornea 1999;18:164 –71. 12. Holland EJ. Epithelial transplantation for the management of severe ocular surface disease. Trans Am Ophthalmol Soc 1996;94:677–743. 13. Daya SM, Ilari L. Living related conjunctival limbal allograft for the treatment of stem cell deficiency. Ophthalmology 2001;108:126 – 34. 14. Tsai RJF, Tseng SCG. Human allograft limbal transplantation for corneal surface reconstruction. Cornea 1994;13:389 – 400. 15. Tan DTH, Ficker LA, Buckley RJ. Limbal transplantation. Ophthalmology 1996;103:29 –36. 16. Tsubota K, Toda I, Saito H, et al. Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology 1995;102:1486 –96. 17. Tsubota K, Satake Y, Kaido M, et al. Treatment of severe ocular surface disorders with corneal epithelial stem-cell transplantation. N Engl J Med 1999;340:1697–703. 1166 18. Tseng SCG, Prabhasawat P, Barton K, et al. Amniotic membrane transplantation with or without limbal allografts for corneal surface reconstruction in patients with limbal stem cell deficiency. Arch Ophthalmol 1998;116:431– 41. 19. Theng JTS, Tan DTH. Combined penetrating keratoplasty and limbal allograft transplantation for severe corneal burns. Ophthalmic Surg Lasers 1997;28:765– 68. 20. Tsubota K, Shimazaki J. Surgical treatment of children blinded by Stevens-Johnson syndrome. Am J Ophthalmol 1999;128:573– 81. 21. Dohlman CH, Terada H. Keratoprosthesis in pemphigoid and Stevens-Johnson syndrome. Adv Exp Med Biol 1998;438: 1021–25. 22. Prabhasawat P, Tseng SCG. Impression cytology study of epithelial phenotype of ocular surface reconstructed by preserved human amniotic membrane. Arch Ophthalmol 1997; 115:1360 – 67. 23. Solomon A, Touhami A, Sandoval H, Tseng SCG. Neurotrophic keratopathy: basic concepts and therapeutic strategies. Comp Ophthalmol Update 2000;3:165–74. 24. Tsubota K, Satake Y, Ohyama M, et al. Surgical reconstruction of the ocular surface in advanced ocular cicatricial pemphigoid and Stevens-Johnson syndrome. Am J Ophthalmol 1996;122:38 –52. 25. Shimazaki J, Shimmura S, Fujishima H, Tsubota K. Association of preoperative tear function with surgical outcome in severe Stevens-Johnson syndrome. Ophthalmology 2000;107:1518 –23. 26. Rao SK, Rajagopal R, Sitalakshmi G, Padmanabhan P. Limbal allografting from related live donors for corneal surface reconstruction. Ophthalmology 1999;106:822–28. 27. Henderson TRM, Coster DJ, Williams KA. The long term outcome of limbal allografts: the search for surviving cells. Br J Ophthalmol 2001;85:604 –9. 28. Daya SM, Bell RWD, Habib NE, et al. Clinical and pathologic findings in human keratolimbal allograft rejection. Cornea 2000;19:443–50. 29. Swift GJ, Aggarwal RK, Davis GJ, et al. Survival of rabbit limbal stem cell allografts. Transplantation 1996;62:568 –74. 30. Shimazaki J, Kaido M, Shinozaki N, et al. Evidence of longterm survival of donor-derived cells after limbal allograft transplantation. Invest Ophthalmol Vis Sci 1999;40:1664 – 8. 31. Shimazaki J, Maruyama F, Shimmura S, et al. Immunologic rejection of the central graft after limbal allograft transplantation combined with penetrating keratoplasty. Cornea 2001; 20:149 –52. 32. Croasdale CR, Schwartz GS, Malling JV, Holland EJ. Keratolimbal allograft: recommendations for tissue procurement and preparation by eye banks, and standard surgical technique. Cornea 1999;18:52– 8. 33. Bersudsky V, Blum-Hareuveni T, Rehany U, Rumelt S. The profile of repeated corneal transplantation. Ophthalmology 2001;108:461– 69. 34. Tsai RJF, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med 2000;343:86 –93. 35. Schwab IR, Reyes M, Isseroff RR. Successful transplantation of bioengineered tissue replacements in patients with ocular surface disease. Cornea 2000;19:421–26. 36. Koizumi N, Inatomi T, Suzuki T, et al. Cultivated corneal epithelial transplantation for ocular surface reconstruction in acute phase of Stevens-Johnson syndrome. Arch Ophthalmol 2001;119:298 –300. 37. Griffith M, Osborne R, Munger R, et al. Functional human corneal equivalents constructed from cell lines. Science 1999; 286:2169 –72.