Cell types of the Epidermis
advertisement

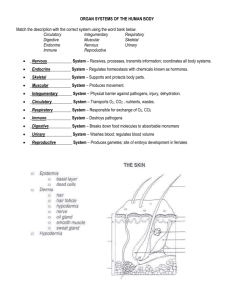
Chapter 5 The Integumentary System General Anatomy • Skin and its accessory structures • Objectives: – – – – – • A large organ composed of all 4 tissue types structure function growth and repair development aging • Square feet? • Thickness? • Weight? 5-1 5-2 Overview Functions of the Skin epidermis • Thermoregulation (sweat – blood vessels) • Protection as physical barrier (cells junctions, cancer prevent, dehydration) • Sensory receptors (sensation) • Excretion and absorption • Synthesis of vitamin D (calcitrol) • 2Types: thick & thin • 2 Major layers of skin (aka: cutaneous layer) 1) epidermis is epithelial tissue dermis Sub-Q 2) dermis is all tissues – AKA: Intradermal layer • Subcutaneous layer (aka: subQ or hypodermis) (adipose & connective tissue) 5-3 5-4 Cell types of the Epidermis Overview of Epidermis • Keratinocytes--90% • Stratified squamous epithelium • Blood vessels? • 4 types of cells • 5 distinct strata (layers) of cells – produce keratin • Melanocytes-----8 % – produce melanin pigment • Langerhans cells (Dendritic cells) – From WBCs – provide immunity • Merkel cells – deepest layer – form touch receptor 5-5 5-6 1 Layers (Strata) of the Epidermis Stratum Basale • Stratum corneum • Stratum lucidum • Stratum granulosum • Stratum spinosum • Stratum basale • Deepest layer- single row of cells (AKA: stratum germinativum) • Combination of merkel cells, melanocytes, keratinocytes stem cells that divide repeatedly • Attached to basement membrane • Scattered protein forms keratin higher up (tonofilaments) 5-7 5-8 Stratum Granulosum Stratum Spinosum • 8 to 10 cell layers • Keratinocytes • Melanin taken in by phagocytosis • Slides look spiny • 3 - 5 layers of flat dying cells (apoptosis!) • keratohyalin granules: (converts protein to keratin) • Lamellar granules: release lipids that repels water 5-9 5-10 Stratum Corneum Stratum Lucidum • Only in thick skin: palms, fingers, & soles • 3 - 5 layers of clear, flat, dead cells • Dead keratinocytes w/ lots of keratin 5-11 • 25 to 30 layers of flat dead cells – lots of keratin and surrounded by lipids • Continuously shed 5-12 2 Keratinization & Epidermal Growth • Stem cells (stratem basale) produce keratinocytes and other cells • Cells are pushed towards surface (mitosis), filling with keratin (keratinization) • ~ 4 week journey Dermis: 2nd layer of skin • Connective tissue layer composed of collagen & elasticextra-cellular fibers, fibroblasts, Secretes matrix macrophages & fat cells • Hair follicles, glands, nerves & blood vessels • 2 major regions of dermis 1 - papillary region 2 - reticular region 5-13 Papillary Region 5-14 Reticular Region • Top 20% of dermis • Composed of CT (w/ elastic fibers) – Areolar tissue • Finger like projections called dermal papillae – Epidermial ridges downward Functions: – anchor epidermis to dermis – contains capillaries – contains Meissner’s corpuscles (touch) & free nerve endings (pain and temperature) • Connective tissue (collagen and elastic fibers) - strength, stretch, & return to shape - Packed with oil glands, sweat gland ducts, fat cells, hair follicles, blood vessels, nerves Hypodermis – subcutaneous fat! 5-15 5-16 Skin Color • melanin – most significant factor in skin color – produced by melanocytes – accumulate in the keratinocytes • eumelanin – brownish black • pheomelanin - a reddish yellow sulfur-containing pigment Lines of cleavage: direction of collagen fibers in reticular region 5-17 Cellular extension of melanocyte Epidermis Pigment granules Golgi apparatus Melanocyte nucleus Basement membrane • Hemoglobin • Carotene (pigment) Dermis 6-18 3 Abnormal Skin Colors Accessory Structures of Skin • cyanosis – blueish hue - from O2 deficiency • erythema – abnormal redness: dilated cutaneous vessels • pallor – pale or ashen color: little blood flow so collagen shows through – emotional stress, low blood pressure, circulatory shock, cold, anemia • albinism – genetic lack of melanin that results in white hair, pale skin, and pink eyes – have inherited recessive, nonfunctional tyrosinase allele • jaundice - yellowing of skin and sclera due to excess bilirubin in blood – cancer, hepatitis, cirrhosis, other compromised liver function • hematoma – (bruise) mass of clotted blood showing through skin – hair – oil glands – sweat glands – nails 6-19 Structure of Hair Functions of Hair? • • • • 5-20 • Dead keratinized cells • Shaft -- visible Prevents heat loss UV Protection Protect eyes Touch receptors – medulla, cortex & cuticle • • • • 5-21 Root = below the surface Follicle surrounds root Blood vessels Germinal cell layer 5-22 Medulla Arrector pili muscle Cortex (tightly packed cells) Cuticle (scales) Follicle surrounds the root Sebaceous gland papilla Bulb 5-23 5-24 4 Hair Related Structures The Hair Cycle. • Arrector pili – smooth muscle in dermis – Hair root plexus – (nerves detect hair movement) Old club hair Epidermis Sebaceous gland Piloerector New hair Club hair (detached from matrix) Club Bulge Hair matrix Hair bulb Degeneration of lower follicle Dermal papilla Dermis 1 Anagen (early) Anagen (mature) (Growing phase, 6–8 years) Stem cells multiply and follicle grows deeper into dermis; hair matrix cells multiply and keratinize, causing hair to grow upward; old club hair may persist temporarily alongside newly growing hair. 2 Catagen (Degenerative phase, 2–3 weeks) Hair growth ceases; hair bulb keratinizes and forms club hair; lower follicle degenerates. 3 Telogen (Resting phase, 1–3 months) Dermal papilla has ascended to level of bulge; club hair falls out, usually in telogen or next anagen. 5-25 Glands of the Skin • Specialized exocrine glands found in dermis • • • • Sebaceous gland (oil) Sebaceous (oil) glands Sudiferous (sweat) glands Ceruminous (wax) glands Mammary (milk) glands Merocrine (Eccrine) sweat gland Sudiferous Sudiferous 5-27 Apocrinesweat sweatgland gland Apocrine Histology of skin glands 5-28 Sudoriferous (sweat) glands (2 types) Sebaceous (oil) glands 1. Eccrine (sweat) glands – most areas of skin – secretory portion in dermis with duct to surface – perspiration/evaporation 2. Apocrine (sweat) glands – axillary and pubic regions – secretory portion in dermis with duct to hair follicle • Secretory portion in the dermis • Most open onto hair shafts • Sebum (oily substance) – keeps hair and skin soft & pliable – inhibits growth of bacteria/fungi 5-29 5-30 5 Fingernail Structure Ceruminous glands Free edge Nail body Nail groove • Modified sweat glands produce waxy secretion in ear canal • Cerumin (earwax = oil and wax glands) • ??? Function Nail fold Lunule Eponychium (cuticle) Nail root Nail plate Free edge 5-31 Nail body Nail bed Degrees of Burn Injuries Nail fold Eponychium (cuticle) 6-32 Nail matrix Degrees of Burn Injuries Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Partial-thickness burns (a) First degree Partial-thickness burns Full-thickness burns (b) Second degree (c) Third degree (a) First degree (b) Second degree Full-thickness burns (c) Third degree a: © SPL/Custom Medical Stock Photo, Inc.; b-c: © John Radcliffe/Photo Researchers, Inc. Figure 6.13 6-33 Figure 6.13 6