ARTICLE IN PRESS
PHYST-709; No. of Pages 5
Physiotherapy xxx (2013) xxx–xxx
Effects of kinesiotaping on foot posture in participants with pronated foot:
A quasi-randomised, double-blind study
Alejandro Luque-Suarez a,∗ , Gabriel Gijon-Nogueron b , Francisco Javier Baron-Lopez c ,
Maria Teresa Labajos-Manzanares a , Julia Hush d , Mark Jonathan Hancock d
a Physiotherapy Department, University of Malaga, Malaga, Spain
Nursing and Podiatry Department, University of Malaga, Malaga, Spain
c Faculty of Medicine, University of Malaga, Malaga, Spain
Department of Health Professions, Faculty of Human Sciences, Macquarie University, Sydney, Australia
b
d
Abstract
Objective To investigate whether kinesiotaping improves excessive foot pronation compared with sham kinesiotaping.
Design Quasi-randomised, double-blind study.
Setting One primary care centre.
Participants One hundred and thirty participants were screened for inclusion. Sixty-eight participants with pronated feet [Foot Posture Index
(FPI) ≥ 6] were enrolled, and the follow-up rate was 100%.
Interventions Participants were allocated into one of two groups: an experimental kinesiotaping group (KT1) and a sham taping group (KT2).
Measures were collected by a blinded assessor at baseline, and 1 minute, 10 minutes, 60 minutes and 24 hours after taping.
Main outcome measures The primary outcome was total FPI score, and the secondary outcome was rear-foot FPI score.
Results There were no significant differences in total FPI score between kinesiotaping and sham taping at any time point. Similarly, there
were no significant differences in rear-foot FPI score, apart from at 60-minute follow-up when the difference between groups was significant
(P = 0.04) but the effect size was very small (0.85 points on the rear-foot FPI score between −6 and +6).
Conclusions Kinesiotaping does not correct foot pronation compared with sham kinesiotaping in people with pronated feet.
© 2013 Chartered Society of Physiotherapy. Published by Elsevier Ltd. All rights reserved.
Keywords: Foot; Pronation; Athletic taping
Introduction
Excessive foot pronation has been defined as a flattening
or loss of the medial longitudinal arch [1,2]. The subtalar and
midtarsal joints exhibit movement beyond the normal range
of motion, and the foot remains pronated for a prolonged
period of time during the gait cycle [3]. This condition has
been cited as a contributing factor to many lower limb overuse
injuries. A pronated foot type has been associated with medial
tibial stress syndrome [4], plantar fasciitis [5], hallux rigidus
[6] and patellofemoral pain syndrome [7]. Several tools have
∗ Correspondence: Facultad de Ciencias de la Salud, Universidad de
Malaga, Paseo de Martiricos, s/n, 29009 Malaga, Spain.
Tel.: +34 952137068; fax: +34 952132913.
E-mail address: aluques@uma.es (A. Luque-Suarez).
been developed to assess the degree of foot pronation, including the navicular drop test [8,9], tibial rotation angles [10] and
Foot Posture Index (FPI) [11].
Interventions used to attempt to correct excessive pronation include prescription of orthotics [12] and taping.
Low-dye taping and high-taping techniques have been investigated in the correction of foot pronation [13–17]; however,
to the authors’ knowledge, kinesiotaping has not been examined to date.
Kinesiotaping has recently become increasingly popular
for the management of musculoskeletal impairments, including foot pronation. Kinesiotaping is designed to mimic the
qualities of human skin. Unlike rigid tape, which is used in
most traditional taping techniques, kinesiotaping has comparable thickness to the skin epidermis and can be stretched
longitudinally between 30% and 40% of its resting length
[18].
0031-9406/$ – see front matter © 2013 Chartered Society of Physiotherapy. Published by Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.physio.2013.04.005
Please cite this article in press as: Luque-Suarez A, et al. Effects of kinesiotaping on foot posture in participants with pronated foot: A
quasi-randomised, double-blind study. Physiotherapy (2013), http://dx.doi.org/10.1016/j.physio.2013.04.005
PHYST-709; No. of Pages 5
ARTICLE IN PRESS
2
A. Luque-Suarez et al. / Physiotherapy xxx (2013) xxx–xxx
While evidence exists that traditional taping can be effective in controlling excessive pronation [16,17,19,20], no
studies have been published regarding the effectiveness of
kinesiotaping for controlling foot pronation. The beneficial
effects of traditional taping on correction of foot pronation
have been shown to reduce after 10 to 30 minutes [17,19].
Current evidence suggests that traditional taping interventions may be effective via a sensorimotor or psychophysical
feedback loop, rather than simply by ‘motion control’ [21].
In this sense, kinesiotaping has been shown to be effective
in providing alignment correction in scapular movements
[22] by offering constant proprioceptive feedback, although
underlying mechanisms remain unclear. Therefore, it is feasible that kinesiotaping may be effective in correcting excessive
pronation despite lacking the rigid properties of traditional
tape. If kinesiotaping could reduce pronation and the effects
could be maintained over time, it could be a simple alternative to traditional taping in people with overpronated
feet.
As such, the aim of this study was to investigate whether
kinesiotaping can improve excessive pronation, and if so, how
well this correction is maintained over the first 24 hours.
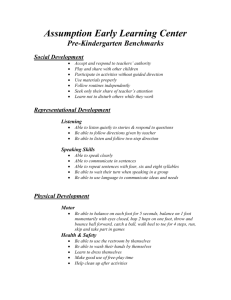
Fig. 1. Participant in experimental kinesiotaping group.
Methods
Participants
One hundred and thirty volunteers from the student body
of the Health Sciences School, University of Malaga were
screened for inclusion in the study. The inclusion criteria
were: (i) FPI score of 6 to 12; (ii) no ankle injury within
the previous 6 months; (iii) no ankle pain at the time of
the study; (4) age between 18 and 40 years; and (5) able
to provide informed, written consent. Sixty-eight participants were enrolled into the study (Fig. A, see supplementary
online material). Informed written consent was obtained from
all participants before enrolment, and all rights of the participants were protected. All procedures were approved by
the Medical Research Ethics Committee of the Faculty of
Nursing, Physiotherapy, Podiatry and Occupational Therapy,
University of Malaga and in accordance with the Declaration
of Helsinki.
Protocol
Baseline assessment/screening
All potential participants completed a questionnaire
regarding demographic data (gender, age, height and weight).
Subsequently, the FPI score of all potential participants was
assessed on the foot of the dominant lower limb by an experienced podiatrist (GGN), who was unaware of the requirement
of an FPI score ≥6 for inclusion in the study. The assessor of
FPI was also blinded to the participant’s identity; a folding
screen was placed between the subject and the assessor, and
only the foot and 10 cm of shank were visible to the assessor.
Following the collection of baseline data, participants who
met the inclusion criteria were allocated to one of two groups:
experimental kinesiotaping group (KT1) or placebo kinesiotaping group (KT2), based on alternative entry into the study.
Participants returned the following day for kinesiotaping
according to their group allocation. Participants underwent
blinded assessment of their FPI score immediately after taping, and then 1 minute, 10 minutes, 60 minutes and 24 hours
later (Fig. A, see supplementary online material).
When the assessor scored FPI for each participant, the
values were recorded by a research assistant. As such, the
assessor was blinded to the treatment group (taping or sham
taping), identity of participant (only foot was visible) and
order of testing (each test could be any of the four follow-up
time points).
All taping was applied by the primary author (ALS), an
experienced kinesiotaping practitioner, to the foot of the dominant lower limb of each participant.
Experimental group (KT1)
Kinesiotaping was applied according to procedures recommended by Pijnappel [23]. Standard 5-cm blue Cure© tape
was used for both groups. A single strip, 20 cm in length, was
applied from the fibula (lateral malleolus), around the calcaneus, with 100% stretch, to the middle third of the medial
tibia. The strip was applied directly to the skin, with the
subject in a supine position and the rear foot positioned in
a supinated position (Fig. 1). Once applied, the instructor
warmed up the kinesiotaping strip by rubbing his hand three
times from the fibula (malleolus) to the middle third of the
tibia in order to maximise tape adhesion.
Please cite this article in press as: Luque-Suarez A, et al. Effects of kinesiotaping on foot posture in participants with pronated foot: A
quasi-randomised, double-blind study. Physiotherapy (2013), http://dx.doi.org/10.1016/j.physio.2013.04.005
ARTICLE IN PRESS
PHYST-709; No. of Pages 5
A. Luque-Suarez et al. / Physiotherapy xxx (2013) xxx–xxx
3
Table 1
Baseline characteristics of subjects.
Age in years, mean (SD)
Females, n (%)
Height in cm, mean (SD)
Weight in kg, mean (SD)
FPI, mean (SD)
Rear-foot FPI, mean (SD)
Experimental group (KT1) n = 34
Sham group (KT2) n = 34
P-value
25 (6)
22 (65%)
169.7 (6.5)
65.5 (8.2)
8.3 (1.7)
3.8 (1.5)
25 (7)
20 (59%)
169.3 (7.1)
66.6 (8.0)
8.2 (1.7)
3.7 (1.4)
0.884
0.624
0.980
0.771
0.780
0.690
FPI, Foot Posture Index; SD, standard deviation.
Sham kinesiotaping (KT2)
In order to simulate the experimental taping technique
(KT1) but without the mechanical effect, the sham kinesiotape was applied in an identical manner but without tension
and without any mechanical correction (i.e. the rear foot
was positioned in neutral). A longer strip of tape (28 cm)
was used as the tape was not stretched. This resulted in the
tape travelling the same distance on the patient’s skin as the
KT1 group, and enabled blinding of the participant and the
outcome assessor.
a statistician blinded to group status. P < 0.05 was considered
to be statistically significant. Data were tested for normality
using the Kolmogorov–Smirnoff test, and all data were
normally distributed. Linear regression was used to evaluate
the influence of treatment group on FPI scores for each of
the four follow-up time points. Baseline FPI scores were
added as a covariate in each model. Separated analyses were
performed for total FPI score and rear-foot FPI score.
Results
Outcome measure: FPI measurements
Foot pronation was assessed using the FPI, measured
immediately after taping, and then 1 minute, 10 minutes,
60 minutes and 24 hours later. The FPI is a six-item clinical
assessment tool used to evaluate foot posture with acceptable validity [24]. The FPI has demonstrated good intrarater
reliability (0.893–0.958) [25]. The FPI evaluates the multisegmental nature of foot posture in all three planes, and does
not require the use of specialised equipment. Each item of the
FPI is scored between −2 and +2, to give a total between −12
(highly supinated) and +12 (highly pronated). Items include:
talar head palpation, curves above and below the lateral malleoli, calcaneal angle, talonavicular bulge, medial longitudinal
arch, and fore-foot to rear-foot alignment. The FPI score was
measured by a single blinded podiatrist, experienced in using
the FPI, for all participants and at all time points (including baseline). Participants were assessed while in a relaxed
standing position.
The primary outcome measure was the total FPI score
(scale from −12 to +12), and the secondary outcome measure
was the rear-foot FPI score (scale from −6 to +6). Rear-foot
FPI score was calculated from the following items: talar head
palpation, curves above and below the lateral malleoli and
calcaneal angle. This was chosen because the intervention
was applied directly to the calcaneus and was therefore most
likely to influence rear-foot posture.
A between-group difference of 1.5 points was considered
to be clinically important. Using the baseline standard deviation (SD) of 1.7, 27 participants per group provided more
than 90% power to detect a difference of 1.5 points.
Data analysis
Data were analysed using Statistical Package for the
Social Sciences Version 19 (IBM Corp., New York, USA) by
One hundred and thirty participants were screened. Of
these, 62 were excluded because they did not have a pronated
foot (FPI score ≤5), and 68 were enrolled into the study (Fig.
A, see supplementary online material): 34 in KT1 and 34 in
KT2.
Demographic characteristics and baseline FPI measures
are shown in Table 1. The mean age of the participants was
24 years, and 65% were female. Mean baseline total FPI score
was 8.3 (SD 1.7) (scale from −12 to +12) and mean rear-foot
FPI score was 3.8 (SD 1.5) (scale from −6 to +6). There were
no significant differences in the demographic characteristics
or FPI scores between the two groups at baseline.
No adverse effects were reported by any of the participants
during treatment or follow-up periods.
Table 2 shows the effects of active kinesiotaping (KT1)
compared with sham taping (KT2) on FPI score, and Table 3
shows the effects on rear-foot FPI score. Both tables present
KT1 and KT2 means and effect sizes with associated 95%
confidence intervals at 1 minute, 10 minutes, 60 minutes and
24 hours after treatment for FPI measurement. There were no
significant differences in total FPI score between kinesiotaping and sham taping at any time point. Similarly, there were
no significant differences in rear-foot FPI score, apart from
at 60-minute follow-up where the difference between groups
just reached statistical significance (P = 0.04) but the effect
size was very small (0.85 points on the FPI).
Discussion
This study investigated whether kinesiotaping is effective in reducing pronation in individuals with pronated feet
compared with sham kinesiotaping. The results suggest that
kinesiotaping is not effective in reducing pronation measured
Please cite this article in press as: Luque-Suarez A, et al. Effects of kinesiotaping on foot posture in participants with pronated foot: A
quasi-randomised, double-blind study. Physiotherapy (2013), http://dx.doi.org/10.1016/j.physio.2013.04.005
PHYST-709; No. of Pages 5
ARTICLE IN PRESS
4
A. Luque-Suarez et al. / Physiotherapy xxx (2013) xxx–xxx
Table 2
Change scores in Foot Posture Index after treatment.
1 minute
10 minutes
60 minutes
24 hours
Experimental group
(KT1) mean (SD)
Sham group
(KT2) mean (SD)
Between-group difference
(mean, 95% CI)
P-value
4.76 (2.41)
5.53 (2.02)
5.35 (2.59)
6.56 (2.50)
5.15 (2.29)
5.18 (2.42)
5.94 (2.16)
6.38 (2.37)
0.41 (−0.72 to 1.54)
−0.35 (−1.38 to0.74)
0.60 (−0.58 to 1.75)
−0.18 (−1.12 to0.93)
0.47
0.55
0.32
0.85
Experimental group
(KT1) mean (SD)
Sham group
(KT2) mean (SD)
Between-group difference
mean (95% CI)
P-value
2.62 (1.71)
2.59 (1.44)
2.74 (1.71)
3.59 (1.63)
3.09 (1.86)
3.29 (1.57)
3.59 (1.74)
3.50 (1.80)
0.47 (−0.31 to 1.35)
0.70 (−0.01 to 1.45)
0.85 (0.27 to 1.71)
−0.09 (−0.76 to 7.3)
0.21
0.05
0.04
0.97
SD, standard deviation; CI, confidence interval.
Table 3
Change scores in rear-foot Foot Posture Index after treatment.
1 minute
10 minutes
60 minutes
24 hours
SD, standard deviation; CI, confidence interval.
using total FPI score or rear-foot FPI score. No change in the
effectiveness of kinesiotaping was identified during the first
24 hours post application.
The strengths of this study were: (i) the outcome assessor
and statistician were blinded to group allocation; and (ii) FPI
scores were collected at four time points after kinesiotaping
to investigate how the effect of kinesiotaping changed over
time. All participants enrolled in the study were followed-up.
However, a limitation of the current study was the allocation system used, based on alternative entry into the study,
which may have contributed to bias. Furthermore, while
these results provide information about the effects of kinesiotaping on foot posture in individuals without lower limb
injuries or pain, the effects on a clinical population are
unknown.
To the authors’ knowledge, this is the first study to investigate the effect of kinesiotaping on foot pronation. However,
previous research has been conducted on the effects of
kinesiotaping on the ankle, such as effects on the Achilles
tendon [26] and proprioception [27]. Beneficial therapeutic
effects of kinesiotaping on self-reported outcomes such as
pain and range of movement have been reported [28] in
patients with ankle sprains and plantar fasciitis [29]. To the
authors’ knowledge, no previous studies have used the FPI
to obtain quantitative measures of foot posture after tape
application. Previous studies have investigated the effect of
traditional taping on foot pronation using the navicular drop
test [3,19], footprint in plantar pressure platform [3] and rearfoot movement by digitisation of high-speed film data [17].
Holmes et al. [19] applied modified low-dye taping to correct
subtalar misalignment in pronated feet, and reported significant correction of subtalar joint position, measured using
the navicular drop test, 10 minutes after taping. O’Sullivan
et al. [30] reduced pronation with low-dye taping in 20
healthy subjects with a navicular drop test exceeding 10 mm.
Therefore, the current evidence suggests that rigid taping
may be more effective than kinesiotaping in correcting foot
pronation; however, other differences such as the taping
technique (e.g. low-dye taping) and the outcome measure
used (e.g. subtalar joint position) may be responsible for
the differences between studies, and further investigation of
these factors is required.
While the current study did not find any effects of kinesiotaping on foot pronation, it does not rule out the possibility
that such taping may improve clinical outcomes such as pain
and function in people presenting for care with symptoms
related to foot pronation. Further trials on individuals with
pain and excessive pronation are required to investigate this
issue. However, if future trials do find that kinesiotaping of
the foot improves clinical outcomes, the current study suggests that it is unlikely that these effects are due to mechanical
correction of foot pronation.
Conclusion
Kinesiotaping did not correct foot pronation compared
with sham kinesiotaping in people with pronated feet
24 hours after tape application.
Ethical approval: All procedures were approved by the Medical Research Ethics Committee (07/2010) of the Faculty of
Nursing, Physiotherapy, Podiatry and Occupational Therapy,
University of Malaga, and conducted in accordance with the
Declaration of Helsinki.
Conflict of interest: None declared.
Appendix A. Supplementary data
Supplementary data associated with this article can be
found, in the online version, at http://dx.doi.org/10.1016/
j.physio.2013.04.005.
Please cite this article in press as: Luque-Suarez A, et al. Effects of kinesiotaping on foot posture in participants with pronated foot: A
quasi-randomised, double-blind study. Physiotherapy (2013), http://dx.doi.org/10.1016/j.physio.2013.04.005
PHYST-709; No. of Pages 5
ARTICLE IN PRESS
A. Luque-Suarez et al. / Physiotherapy xxx (2013) xxx–xxx
References
[1] Franco AH. Pes cavus and pes planus. Analyses and treatment. Phys
Ther 1987;67:688–94.
[2] Scranton Jr PE, Pedegana LR, Whitesel JP. Gait analysis, alterations
in support phase forces using supportive devices. Am J Sports Med
1982;10:6–11.
[3] Lange B, Chipchase L, Evans A. The effect of low-dye taping on plantar
pressures, during gait, in subjects with navicular drop exceeding 10 mm.
J Orthop Sports Phys Ther 2004;34:201–9.
[4] Raissi GR, Cherati AD, Mansoori KD, Razi MD. The relationship
between lower extremity alignment and medial tibial stress syndrome
among non-professional athletes. Sports Med Arthrosc Rehabil Ther
Technol 2009;1:11.
[5] Graham ME, Jawrani NT, Goel VK. Evaluating plantar fascia strain
in hyperpronating cadaveric feet following an extra-osseous talotarsal
stabilization procedure. J Foot Ankle Surg 2011;50:682–6.
[6] Beeson P, Phillips C, Corr S, Ribbans WJ. Hallux rigidus: a
cross-sectional study to evaluate clinical parameters. Foot 2009;19:
80–92.
[7] Barton CJ, Bonanno D, Levinger P, Menz HB. Foot and ankle characteristics in patellofemoral pain syndrome: a case control and reliability
study. J Orthop Sports Phys Ther 2010;40:286–96.
[8] Bencke J, Christiansen D, Jensen K, Okholm A, Sonne-Holm S, Bandholm T. Measuring medial longitudinal arch deformation during gait.
A reliability study. Gait Posture 2012;35:400–4.
[9] Nilsson MK, Friis R, Michaelsen MS, Jakobsen PA, Nielsen RO. Classification of the height and flexibility of the medial longitudinal arch
of the foot. J Foot Ankle Res 2012;5:3.
[10] Pascual Huerta J, Ropa Moreno JM, Kirby KA, García Carmona FJ,
Orejana García AM. Effect of 7-degree rearfoot varus and valgus wedging on rearfoot kinematics and kinetics during the stance phase of
walking. J Am Podiatr Med Assoc 2009;99:415–21.
[11] Barton CJ, Levinger P, Crossley KM, Webster KE, Menz HB. Relationships between the Foot Posture Index and foot kinematics during gait
in individuals with and without patellofemoral pain syndrome. J Foot
Ankle Res 2011;4:10.
[12] Pinto RZ, Souza TR, Maher CG. External devices (including orthotics)
to control excessive foot pronation. Br J Sports Med 2012;46:110–1.
[13] Yoho R, Rivera JJ, Renschler R, Vardaxis VG, Dikis J. A biomechanical
analysis of the effects of low-dye taping on arch deformation during
gait. Foot (Edinb) 2012;22:283–6.
[14] Franettovich M, Chapman A, Blanch P, Vicenzino B. Continual use of
augmented low-dye taping increases arch height in standing but does
not influence neuromotor control of gait. Gait Posture 2010;31:247–50.
[15] Nolan D, Kennedy N. Effects of low-dye taping on plantar pressure pre
and post exercise: an exploratory study. BMC Musculoskelet Disord
2009;21:10–40.
5
[16] Franettovich MM, Murley GS, David BS, Bird AR. A comparison of
augmented low-dye taping and ankle bracing on lower limb muscle
activity during walking in adults with flat-arched foot posture. J Sci
Med Sport 2012;15:8–13.
[17] Harradine P, Herrington L, Wright R. The effect of low dye taping
upon rearfoot motion and position before and after exercise. Foot
2001;11:57–60.
[18] Gonzalez-Iglesias J, Fernandez-de-Las-Penas C, Cleland JA, Huijbregts P, Del Rosario Gutierrez-Vega M. Short-term effects of cervical
kinesiotaping on pain and cervical range of motion in patients with acute
whiplash injury: a randomized clinical trial. J Orthop Sports Phys Ther
2009;39:515–21.
[19] Holmes CF, Wilcox D, Fletcher JP. Effect of a modified, low-dye
medial longitudinal arch taping procedure on the subtalar joint neutral position before and after light exercise. J Orthop Sports Phys Ther
2002;32:194–201.
[20] O’Sullivan K, Kennedy N, O’Neill E, Ni Mhainin U. The effect of lowdye taping on rearfoot motion and plantar pressure during the stance
phase of gait. BMC Musculoskelet Disord 2008;9:111.
[21] Stacoff A, Reinschmidt C, Nigg BM, van den Bogert AJ, Lundberg
A, Denoth J, et al. Effects of foot orthoses on skeletal motion during
running. Clin Biomech (Bristol, Avon) 2000;15:54–64.
[22] Hsu YH, Chen WY, Lin HC, Wang WT, Shih YF. The effects of
taping on scapular kinematics and muscle performance in baseball
players with shoulder impingement syndrome. J Electromyogr Kinesiol
2009;19:1092–9.
[23] Pijnappel H. Medical taping concept. Aneid (UK) Ltd; 2009.
[24] Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a
novel rating system for scoring standing foot posture: the Foot Posture
Index. Clin Biomech (Bristol Avon) 2006;21:89–98.
[25] Cornwall MW, McPoil TG, Lebec M, Vicenzino B, Wilson J. Reliability of the modified Foot Posture Index. J Am Podiatr Med Assoc
2008;98:7–13.
[26] Bicici S, Karatas N, Baltaci G. Effect of athletic taping and kinesiotaping(R) on measurements of functional performance in basketball
players with chronic inversion ankle sprains. Int J Sports Phys Ther
2012;7:154–66.
[27] Lee JH, Yoo WG. Treatment of chronic Achilles tendon pain by kinesio
taping in an amateur badminton player. Phys Ther Sport 2012;13:115–9.
[28] Gopal Nambi S, Bijal Tarun Shah. Kinesio taping versus Mulligan’s
mobilization with movement in sub-acute lateral ankle sprain in secondary school hockey players – comparative study. Int J Pharm Sci
Health Care 2012;2:136–49.
[29] Tsai C-T, Chang W-D, Lee J-P. Effects of short-term treatment with
kinesiotaping for plantar fasciitis. J Musculoskelet Pain 2010;18:71–80.
[30] O’Sullivan K, Kennedy N, O’Neill E, Ni Mhainin U. The effect of lowdye taping on rearfoot motion and plantar pressure during the stance
phase of gait. BMC Musculoskelet Disord 2008;18:1–9.
Available online at www.sciencedirect.com
Please cite this article in press as: Luque-Suarez A, et al. Effects of kinesiotaping on foot posture in participants with pronated foot: A
quasi-randomised, double-blind study. Physiotherapy (2013), http://dx.doi.org/10.1016/j.physio.2013.04.005