Bones and Skeletal Tissues
advertisement

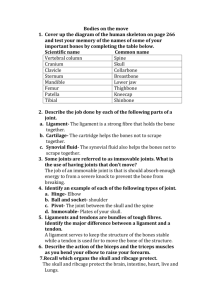
6 Bones and Skeletal Tissues Cartilage • Location and basic structure • Found throughout adult body • Ear and epiglottis • Articular cartilages and costal cartilage • Larynx, trachea, and nose • Intervertebral discs, pubic symphysis, and articular discs Cartilage • Is surrounded by perichondrium • Consists primarily of water • Resilient tissue—it springs back to original shape Types of Cartilage • Hyaline cartilage (glassy) • Most abundant cartilage • Provides support through flexibility • Elastic cartilage—contains many elastic fibers • Able to tolerate repeated bending • Fibrocartilage—resists strong compression and strong tension • An intermediate between hyaline and elastic cartilage Cartilages in the Adult Body Growth of Cartilage • Appositional growth • Chondroblasts in surrounding perichondrium produce new cartilage • Interstitial growth • Chondrocytes within cartilage divide and secrete new matrix • Cartilage stops growing when the skeleton stops growing Tissues in Bone • Bones contain several types of tissues • • • • Dominated by bone CT Contain nervous tissue and blood CT Contain cartilage in articular cartilages Contain ET lining blood vessels Function of Bones • Support—provides hard framework • Movement—skeletal muscles use bones as levers • Protection of underlying organs • Mineral storage—reservoir for important minerals • Blood-cell formation—bone contains red marrow • Energy metabolism—osteoblasts secrete osteocalcin Bone Tissue • Bone tissue • Organic components—cells, fibers, and ground substance • Inorganic components—mineral salts that invade bony matrix Extracellular Matrix • Unique composition of matrix • Gives bone exceptional properties • 35%—organic components • Contributes to flexibility and tensile strength • 65%—inorganic components • Provide exceptional harness, resists compression Cells • Three types of cells in bone produces or maintain bone • Osteogenic cells—stem cells that differentiate into osteoblasts • Osteoblasts—actively produce and secrete bone matrix • Bone matrix is osteoid • Osteocytes—keep bone matrix healthy Cells • Osteoclasts • Responsible for resorption of bone • Are derived from a line of white blood cells • Secrete hydrochloric acid and lysosomal enzymes Classification of Bones • Long bones—longer than wide; a shaft plus ends • Short bones—roughly cube-shaped • Flat bones—thin and flattened, usually curved • Irregular bones—various shapes, do not fit into other categories Gross Anatomy of Bones • Compact bone—dense outer layer of bone • Spongy (cancellous) bone—internal network of bone Structure of a Typical Long Bone • Diaphysis—―shaft‖ of a bone • Epiphysis—ends of a bone • Blood vessels—well vascularized • Medullary cavity—hollow cavity filled with yellow marrow • Membranes • Periosteum, perforating fibers (Sharpey’s fibers), and endosteum Structure of a Long Bone Structure of Short, Irregular, and Flat Bones • Flat bones, short bones, and irregular bones • Contain bone marrow but no marrow cavity • Diploë • Internal spongy bone of flat bones Gross Anatomy of Bones • Bone design and stress • Anatomy of a bone reflects stresses • Compression and tension greatest at external surfaces Bone Markings • Superficial surfaces of bones reflect stresses on them • There are three broad categories of bone markings • Projections for muscle attachment • Surfaces that form joints • Depressions and openings Microscopic Structure of Compact Bones • Compact Bone • Contains passage ways for blood vessels, lymph vessels, and nerves • Osteons—long cylindrical structures • Function in support • Structurally—resembles rings of a tree in cross-section Microscopic Structure of Compact Bones • Osteons contain: • • • • Lamellae Central canal Perforating canals Canaliculi Microscopic Structure of Compact Bones • Spongy Bone • Is less complex than compact bone • Trabeculae contain layers of lamellae and osteocytes • Are too small to contain osteons 6 Bones and Skeletal Tissues Bone Development • Ossification (osteogenesis)—bone-tissue formation • Membrane bones—formed directly from mesenchyme • Intramembranous ossification • Other bones—develop initially from hyaline cartilage • Endochondral ossification Intramembranous Ossification Endochondral Ossification • All bones except some bones of the skull and clavicles • Bones are modeled in hyaline cartilage • Begins forming late in the second month of embryonic development • Continues forming until early adulthood Stages in Endochondral Ossification Anatomy of Epiphyseal Growth Areas • In epiphyseal plates of growing bones: • Cartilage is organized for quick, efficient growth • Cartilage cells form tall stacks • Chondroblasts at the top of stacks divide quickly • Pushes the epiphysis away from the diaphysis • Lengthens entire long bone Anatomy of Epiphyseal Growth Areas • Older chondrocytes signal surrounding matrix to calcify • Older chondrocytes then die and disintegrate • Leaves long trabeculae (spicules) of calcified cartilage on diaphysis side • Trabeculae are partly eroded by osteoclasts • Osteoblasts then cover trabeculae with bone tissue • Trabeculae finally eaten away from their tips by osteoclasts Organization of Cartilage within Epiphyseal Plate of Growing Long Bone Postnatal Growth of Endochondral Bones • During childhood and adolescence: • • • • Bones lengthen entirely by growth of the epiphyseal plates Cartilage is replaced with bone CT as quickly as it grows Epiphyseal plate maintains constant thickness Whole bone lengthens Hormonal Regulation of Bone Growth • Growth hormone—produced by the pituitary gland • Stimulates epiphyseal plates • Thyroid hormone—ensures that the skeleton retains proper proportions • Sex hormones (estrogen and testosterone) • Promote bone growth • Later induces closure of epiphyseal plates Postnatal Growth of Endochondral Bones • As adolescence draws to an end: • Chondroblasts divide less often • Epiphyseal plates become thinner • Cartilage stops growing • Replaced by bone tissue • Long bones stop lengthening when diaphysis and epiphysis fuse Bone Remodeling • Bone is dynamic living tissue • 500 mg of calcium may enter or leave the adult skeleton each day • Cancellous bone of the skeleton is replaced every 3–4 years • Compact bone is replaced every 10 years Postnatal Growth of Endochondral Bones • Growing bones widen as they lengthen • Osteoblasts—add bone tissue to the external surface of the diaphysis • Osteoclasts—remove bone from the internal surface of the diaphysis • Appositional growth—growth of a bone by addition of bone tissue to its surface Bone Remodeling • Bone deposit and removal • Occurs at periosteal and endosteal surfaces • Bone remodeling • Bone deposition—accomplished by osteoblasts • Bone reabsorption—accomplished by osteoclasts Remodeling, Spongy Bone Osteoclast—A Bone-Degrading Cell • A giant cell with many nuclei • Crawls along bone surfaces • Breaks down bone tissue • Secretes concentrated HCl • Lysosomal enzymes are released • Derived from hematopoietic stem cells Repair of Bone Fractures • Simple and compound fractures • Treatment by reduction • Closed reduction • Open reduction Stages of Healing a Fracture Common Types of Fractures Disorders of Bones • Osteoporosis • Characterized by low bone mass • Bone reabsorption outpaces bone deposition • Occurs most often in women after menopause Osteoporosis Disorders of Bones • Osteomalacia • Occurs in adults—bones are inadequately mineralized • Rickets • Occurs in children—analogous to osteomalacia Disorders of Bones • Paget’s disease • Characterized by excessive rate of bone deposition • Osteosarcoma • A form of bone cancer The Skeleton Throughout Life • Cartilage grows quickly in youth • Skeleton shows fewer chondrocytes in the elderly • Bones are a timetable • Mesoderm • Gives rise to embryonic mesenchyme cells • Mesenchyme • Produces membranes and cartilage • Membranes and cartilage ossify The Skeleton Throughout Life • Skeleton grows until the age of 18–21 years • In children and adolescents, bone formation exceeds rate of bone reabsorption • In young adults, bone formation and bone reabsorption are in balance • In old age, reabsorption predominates • Bone mass declines with age 7 Bones, Part 1: The Axial Skeleton The Skeleton • Consists of: • Bones, cartilage, joints, and ligaments • Composed of 206 named bones grouped into two divisions • Axial skeleton (80 bones) • Appendicular skeleton (126 bones) The Axial Skeleton • Formed from 80 named bones • Consists of skull, vertebral column, and bony thorax The Axial Skeleton The Skull • Formed by cranial and facial bones The Cranium • Is the body’s most complex bony structure • Formed by cranial and facial bones • The cranium • Encloses and protects brain • Provides attachment for head and neck muscles The Face • Facial bones serve to • • • • • Form framework of the face Form cavities for the sense organs of sight, taste, and smell Provide openings for the passage of air and food Hold the teeth in place Anchor muscles of the face Overview of Skull Geography • Facial bones form anterior aspect • Cranium is divided into cranial vault and the base • Internally, prominent bony ridges divide skull into distinct fossae Overview of Skull Geography • The skull contains smaller cavities • • • • Middle and inner ear cavities—in lateral aspect of cranial base Nasal cavity—lies in and posterior to the nose Orbits—house the eyeballs Air-filled sinuses—occur in several bones around the nasal cavity Overview of Skull Geography • The skull contains approximately 85 named openings • Foramina, canals, and fissures • Provide openings for important structures • Spinal cord • Blood vessels serving the brain • 12 pairs of cranial nerves Cranial Bones • Formed from eight large bones • Paired bones include • Temporal bones • Parietal bones • Unpaired bones include • Frontal bone • Occipital bone • Sphenoid bone • Ethmoid bone Parietal Bones and Sutures • Parietal bones form superior and lateral parts of skull • Four sutures of the cranium • Coronal suture—runs in the coronal plane • Located where parietal bones meet the frontal bone • Squamous suture—occurs where each parietal bone meets a temporal bone inferiorly Parietal Bones and Sutures • Four sutures of the cranium (continued) • Sagittal suture—occurs where right and left parietal bones meet superiorly • Lambdoid suture—occurs where the parietal bones meet the occipital bone posteriorly Sutural Bones • Small bones that occur within sutures • Irregular in shape, size, and location • Not all people have sutural bones The Skull— Posterior View Frontal Bone • Forms the forehead and roofs of orbits • Supraorbital margin—superior margin of orbits • Glabella—smooth part of frontal bone between superciliary arches • Frontal sinuses within frontal bone • Contributes to anterior cranial fossa Occipital Bone • Forms the posterior portion of the cranium and cranial base • Articulates with the temporal bones and parietal bones • Forms the posterior cranial fossa • Foramen magnum located at its base Occipital Bone • Features and structures • Occipital condyles • Hypoglossal foramen • External occipital protuberance • Superior nuchal lines • Inferior nuchal lines Inferior Aspect of the Skull Temporal Bones • Lie inferior to parietal bones • Form the inferolateral portion of the skull • Term ―temporal‖ comes from Latin word for time • Specific regions of temporal bone • Squamous, temporal, petrous, and mastoid regions Lateral Aspect of the Skull The Temporal Bone • The mastoid process • Site for neck muscle attachment • Contains air sinuses • Petrous region • Projects medially, contributes to cranial base • Houses cavities of middle and internal ear • Contributes to the middle and posterior cranial fossae The Temporal Bone • Foramina of the temporal bone • Jugular foramen • At boundary with occipital bone • Carotid canal • Formane lacerum • Internal accoustic meatus 7 Bones, Part 1: The Axial Skeleton The Sphenoid Bone • Spans the width of the cranial floor • Resembles a butterfly or bat • Consists of a body and three pairs of processes • Contains five important openings • Is the ―keystone‖ of the cranium The Ethmoid Bone • Lies between nasal and sphenoid bones • Forms most of the medial bony region between the nasal cavity and orbits The Ethmoid Bone • Cribiform plate—superior surface of the ethmoid bone • Contain olfactory foramina • Crista galli—attachment for falx cerebri • Perpendicular plate—forms superior part of nasal septum The Ethmoid Bone • Lateral masses—contain air cells • Superior and middle nasal conchae • Extend medially from laterial masses The Ethmoid Bone Facial Bones • Unpaired bones • Mandible and vomer • Paired bones • • • • • • Maxillae Zygomatic bones Nasal bones Lacrimal bones Palatine bones Inferior nasal conchae Facial Bones Mandible • The lower jawbone is the largest and strongest facial bone • Composed of two main parts • Horizontal body • Two upright rami Mandible Maxillary Bones • Articulate with all other facial bones except the mandible • Contain maxillary sinuses—largest paranasal sinuses • Forms part of the inferior orbital fissure • Are the ―keystone‖ bones of the face Other Bones of the Face • Zygomatic bones • Form lateral wall of orbits • Nasal bones • Form bridge of nose • Lacrimal bones • Located in the medial orbital walls • Palatine bones • Complete the posterior part of the hard palate Other Bones of the Face • Vomer • Forms the inferior part of the nasal septum • Inferior nasal conchae • Thin, curved bones that project medially form the lateral walls of the nasal cavity 7 Bones, Part 1: The Axial Skeleton Special Parts of the Skull • Orbits • Nasal cavity • Paranasal sinuses • Hyoid bone Nasal Cavity Nasal Septum Paranasal Sinuses • Air-filled sinuses are located within • • • • Frontal bone Ethmoid bone Sphenoid bone Maxillary bones • Lined with mucous membrane • Lighten the skull Orbits The Hyoid Bone • Lies inferior to the mandible • The only bone with no direct articulation with any other bone • Acts as a movable base for the tongue 7 Bones, Part 1: The Axial Skeleton The Vertebral Column • Formed from 26 bones in the adult • Transmits weight of trunk to the lower limbs • Surrounds and protects the spinal cord The Vertebral Column • Serves as attachment sites for muscles of the neck and back • Held in place by ligaments • Anterior and posterior longitudinal ligaments • Ligamentum flavum The Vertebral Column Regions and Normal Curvatures • The Vertebral column has five major regions • 7 cervical vertebrae of the neck region • 12 thoracic vertebrae • 5 lumbar vertebrae • Sacrum—five fused bones • Inferior to lumbar vertebrae • Coccyx—inferior to sacrum Regions and Normal Curvatures • Curvatures of the spine • Cervical and lumbar curvatures • Concave posteriorly • Thoracic and sacral curvatures • Convex posteriority Regions and Normal Curvatures • Curvatures increase resilience of spine • Thoracic and sacral curvatures • Primary curvatures • Present at birth • Lumbar curvature • Develops when baby begins to walk Ligaments of the Spine • Major supporting ligaments • Anterior longitudinal ligament • Attaches to bony vertebrae and intervertebral discs • Prevents hyperextension • Posterior longitudinal ligament • Narrow and relatively weak • Attaches to intervertebral discs Intervertebral Discs • Are cushion-like pads between vertebrae • Composed of • Nucleus pulposus • Anulus fibrosus Intervertebral Discs • Nucleus pulposus • Gelatinous inner sphere • Absorbs compressive stresses • Anulus fibrosus • Outer fings formed of ligament • Inner rings formed of fibrocartilage • Contain the nucleus pulposus General Structure of Vertebrae • Common structures to all regions • • • • • • • Body Vertebral arch Vertebral foramen Spinous process Transverse process Superior and inferior articular processes Intervertebral foramina 7 Bones, Part 1: The Axial Skeleton Regions Vertebral Characteristics • Specific regions of the spine perform specific functions • Types of movement that occur between vertebrae • Flexion and extension • Lateral flexion • Rotation in the long axis Cervical Vertebrae • Seven cervical vertebrae (C1–C7)—smallest and lightest vertebrae • C3–C7 are typical cervical vertebrae • • • • • Body is wider laterally Spinous processes are short and bifid (except C7) Vertebral foramen are large and triangular Transverse processes contain transverse foramina Superior articular facets face superoposteriorly The Atlas • C1 is termed the atlas • Lacks a body and spinous process • Supports the skull • Superior articular facets receive the occipital condyles • Allows flexion and extension of neck • Nodding the head ―yes‖ The Axis • Has a body and spinous process • Dens (odontoid process) projects superiorly • Formed from fusion of the body of the atlas with the axis • Acts as a pivot for rotation of the atlas and skull • Participates in rotating the head from side to side 7 Bones, Part 1: The Axial Skeleton Thoracic Vertebrae (T1—T12) • All articulate with ribs • Have heart-shaped bodies from the superior view • Each side of the body of T1–T10 bears demifacts for articulation with ribs • T1 has a full facet for the first rib • T10–T12 only have a single facet Thoracic Vertebrae • Spinous processes are long and point inferiorly • Vertebral foramen are circular • Transverse processes articulate with tubercles of ribs • Superior articular facets point posteriorly • Inferior articular processes point anteriorly • Allows rotation and prevents flexion and extension Lumbar Vertebrae (L1—L5) • Bodies are thick and robust • Transverse processes are thin and tapered • Spinous processes are thick, blunt, and point posteriorly • Vertebral foramina are triangular • Superior and inferior articular facets directly medially • Allows flexion and extension—rotation prevented Sacrum (S1—S5) • Shapes the posterior wall of pelvis • Formed from 5 fused vertebrae • Superior surface articulates with L5 • Inferiorly articulates with coccyx • Sacral promontory • Where the first sacral vertebrae bulges into pelvic cavity • Center of gravity is 1 cm posterior to sacral promontory • Ala—develops from fused rib elements Sacrum • Sacral foramina • Ventral foramina • Passage for ventral rami of sacral spinal nerves • Dorsal foramina • Passage for dorsal rami of sacral spinal nerves Coccyx • Is the ―tailbone‖ • Formed from 3—5 fused vertebrae • Offers only slight support to pelvic organs 7 Bones, Part 1: The Axial Skeleton The Thoracic Cage • Forms the framework of the chest • Components • Thoracic vertebrae—posteriorly • Ribs—laterally • Sternum and costal cartilage—anteriorly • Protects thoracic organs • Supports shoulder girdle and upper limbs • Provides attachment sites for muscles Sternum • Formed from three sections • Manubrium—superior section • Articulates with medial end of clavicles • Body—bulk of sternum • Sides are notched at articulations for costal cartilage of ribs 2– 7 • Xiphoid process—inferior end of sternum • Ossifies around age 40 Sternum • Anatomical landmarks • Jugular notch • Central indentation at superior border of the manubrium • Sternal angle • A horizontal ridge where the manubrium joins the body • Xiphisternal joint • Where sternal body and xiphoid process fuse • Lies at the level of the 9th thoracic vertebra Ribs • All ribs attach to vertebral column posteriorly • True ribs - superior seven pairs of ribs • Attach to sternum by costal cartilage • False ribs—inferior five pairs of ribs • Ribs 11–12 are known as floating ribs Disorders of the Axial Skeleton • Cleft palate • A common congenital disorder • Right and left halves of palate fail to fuse medially • Stenosis of the lumbar spine • Narrowing of the vertebral canal • Can compress roots of spinal nerves Disorders of the Axial Skeleton • Abnormal spinal curvatures • Scoliosis—an abnormal lateral curvature • Kyphosis—an exaggerated thoracic curvature • Lordosis—an accentuated lumbar curvature; ―swayback‖ The Axial Skeleton Throughout Life • Membrane bones begin to ossify in second month of development • Bone tissue grows outward from ossification centers • Fontanels • Unossified remnants of membranes Fontanelles The Axial Skeleton Throughout Life • Many bones of the face and skull form by intramembranous ossification • Endochondral bones of the skull • • • • Occipital bone Sphenoid Ethmoid bones Parts of the temporal bone The Axial Skeleton Throughout Life • Aging of the axial skeleton • • • • Water content of the intervertebral discs decreases By age 55, loss of a few centimeters in height is common Thorax becomes more rigid Bones lose mass with age 8 Bones, Part 1: The Appendicular Skeleton The Appendicular Skeleton • Pectoral girdle • Attaches the upper limbs to the trunk • Pelvic girdle • Attaches the lower limbs to the trunk • Upper and lower limbs differ in function • Share the same structural plan The Pectoral Girdle • Consists of the clavicle and the scapula • Pectoral girdles do not quite encircle the body completely • Medial end of each clavicle articulates with the manubrium and first rib • Laterally—the ends of the clavicles join the scapulae • Scapulae do not join each other or the axial skeleton The Pectoral Girdle • Provides attachment for many muscles that move the upper limb • Girdle is very light and upper limbs are mobile • Only clavicle articulates with the axial skeleton • Socket of the shoulder joint (glenoid cavity) is shallow • Good for flexibility, bad for stability Articulated Pectoral Girdle Clavicles • Extend horizontally across the superior thorax • Sternal end articulates with the manubrium • Acromial end articulates with scapula Clavicles • Provide attachment for muscles • Hold the scapulae and arms laterally • Transmit compression forces from the upper limbs to the axial skeleton Scapulae • Lie on the dorsal surface of the rib cage • Located between ribs 2–7 • Have three borders • Superior • Medial (vertebral) • Lateral (axillary) • Have three angles • Lateral, superior, and inferior The Upper Limb • 30 bones form each upper limb • Grouped into bones of the: • Arm • Forearm • Hand Arm • Region of the upper limb between the shoulder and elbow • Humerus • • • • The only bone of the arm Longest and strongest bone of the upper limb Articulates with the scapula at the shoulder Articulates with the radius and ulna at the elbow Arm • Humerus • Many structures of the humerus provide sites for muscle attachment • Other structures of the humerus provide articulation sites for other bones Forearm • Formed from the radius and ulna • Proximal ends articulate with the humerus • Distal ends articulate with carpals Forearm • Radius and ulna articulate with each other • At the proximal and distal radioulnar joints • The interosseous membrane • Interconnects radius and ulna • In anatomical position; the radius is lateral and the ulna is medial Ulna • Main bone responsible for forming the elbow joint with the humerus • Hinge joint allows forearm to bend on arm • Distal end is separated from carpals by fibrocartilage • Plays little to no role in hand movement Proximal Part of the Ulna Radius and Ulna Radius • Superior surface of the head of the radius articulates with the capitulum • Medially—the head of the radius articulates with the radial notch of the ulna • Contributes heavily to the wrist joint • Distal radius articulates with carpal bones • When radius moves, the hand moves with it Distal Ends of the Radius and Ulna 8 Bones, Part 1: The Appendicular Skeleton Hand • Includes the following bones • Carpus—wrist • Metacarpals—palm • Phalanges—fingers Carpus • Forms the true wrist—the proximal region of the hand • Gliding movements occur between carpals • Composed of eight marble-sized bones Carpus • Carpal bones • Are arranged in two irregular rows • Proximal row from lateral to medial • Scaphoid, lunate, triquetral, and pisiform • Distal row from lateral to medial • Trapezium, trapezoid, capitate, and hamate • A mnemonic to help remember carpals: • Sally left the party to take Carmen home Bones of the Hand Metacarpus • Five metacarpals radiate distally from the wrist • Metacarpals form the palm • Numbered 1–5, beginning with the pollex (thumb) • Articulate proximally with the distal row of carpals • Articulate distally with the proximal phalanges Phalanges • Numbered 1–5, beginning with the pollex (thumb) • Except for the thumb, each finger has three phalanges • Proximal, middle, and distal Bones of the Appendicular Skeleton Pelvic Girdle • Attaches lower limbs to the spine • Supports visceral organs • Attaches to the axial skeleton by strong ligaments • Acetabulum is a deep cup that holds the head of the femur • Lower limbs have less freedom of movement • Are more stable than the arm Pelvic Girdle • Consists of paired hip bones (coxal bones) • Hip bones unite anteriorly with each other • Articulates posteriorly with the sacrum Bones of the Pelvic Girdle • A deep, basin-like structure • Formed by: • Coxal bones, sacrum, and coccyx The Pelvic Girdle • Consists of three separate bones in childhood • Ilium, ischium, and pubis • Bones fuse, retain separate names to regions of the coxal bones • Acetabulum • A deep hemispherical socket on lateral pelvic surface Ilium • Large, flaring bone • Forms the superior region of the coxal bone • Site of attachment for many muscles • Articulation with the sacrum forms sacroiliac joint Ischium • Forms posteroinferior region of the coxal bone • Anteriorly—joins the pubis • Ischial tuberosities • Are the strongest part of the hip bone Pubis • Forms the anterior region of the coxal bone • Lies horizontally in anatomical position • Pubic symphysis • The two pubic bones are joined by fibrocartilage at the midline • Pubic arch—inferior to the pubic symphysis • Angle helps distinguish male from female pelves Lateral and Medial Views of the Hip Bone True and False Pelves • Bony pelvis is divided into two regions • False (greater) pelvis—bounded by alae of the iliac bones • True (lesser) pelvis—inferior to pelvic brim • Forms a bowl containing the pelvic organs 8 Bones, Part 1: The Appendicular Skeleton Pelvic Structures and Childbearing • Major differences between male and female pelves • Female pelvis is adapted for childbearing • Pelvis is lighter, wider, and shallower than in the male • Provides more room in the true pelvis Female and Male Pelves The Lower Limb • Carries the entire weight of the erect body • Bones of lower limb are thicker and stronger than those of upper limb • Divided into three segments • Thigh, leg, and foot Thigh • The region of the lower limb between the hip and the knee • Femur—the single bone of the thigh • Longest and strongest bone of the body • Ball-shaped head articulates with the acetabulum Structures of the Femur Patella • Triangular sesamoid bone • Imbedded in the tendon that secures the quadriceps muscles • Protects the knee anteriorly • Improves leverage of the thigh muscles across the knee Leg • Refers to the region of the lower limb between the knee and the ankle • Composed of the tibia and fibula • Tibia—more massive medial bone of the leg • Receives weight of the body from the femur • Fibula—stick-like lateral bone of the leg • Interosseous membrane • Connects the tibia and fibula Leg • Tibia articulates with femur at superior end • Forms the knee joint • Tibia articulates with talus at the inferior end • Forms the ankle joint • Fibula does not contribute to the knee joint • Stabilizes the ankle joint Structures of the Tibia and Fibula The Foot • Foot is composed of • Tarsus, metatarsus, and the phalanges • Important functions • Supports body weight • Acts as a lever to propel body forward when walking • Segmentation makes foot pliable and adapted to uneven ground Tarsus • Makes up the posterior half of the foot • Contains seven bones called tarsals • Body weight is primarily borne by the talus and calcaneus • Trochlea of the talus • Site of articulation with the tibia • Other tarsals are: • Cuboid and navicular • Medial, intermediate, and lateral cuneiforms Metatarsus • Consists of five small long bones called metatarsals • Numbered 1–5 beginning with the hallux (great toe) • First metatarsal supports body weight Phalanges of the Toes • 14 phalanges of the toes • Smaller and less nimble than those of the fingers • Structure and arrangement are similar to phalanges of fingers • Except for the great toe, each toe has three phalanges • Proximal, middle, and distal Arches of the Foot • Foot has three important arches • Medial and lateral longitudinal arch • Transverse arch • Arches are maintained by • Interlocking shapes of tarsals • Ligaments and tendons • ―Keystones‖ of arches • Talus—medial longitudinal arch • Cuboid—lateral longitudinal arch Lower Limb and Pelvis Disorders of the Appendicular Skeleton • Bone fractures • Hip dysplasia • Head of the femur slips out of acetabulum • Clubfoot • Soles of the feet turn medially The Appendicular Skeleton Throughout Life • Growth of the appendicular skeleton • Increases height • Changes body proportions • Upper/lower body ratio changes with age • At birth, head and trunk are 1.5 times as long as lower limbs • Lower limbs grow faster than the trunk • Upper/lower body ratio of 1 to 1 by age 10 Changes in Body Proportions The Appendicular Skeleton Throughout Life • Few changes occur in adult skeleton until middle age, when • Skeleton loses mass • Osteoporosis and limb fractures become more common 9 Joints Joints • Rigid elements of the skeleton meet at joints or articulations • Greek root ―arthro‖ means joint • Structure of joints • Enables resistance to crushing, tearing, and other forces Classifications of Joints • Joints can be classified by function or structure • Functional classification—based on amount of movement • Synarthroses—immovable; common in axial skeleton • Amphiarthroses—slightly movable; common in axial skeleton • Diarthroses—freely movable; common in appendicular skeleton (all synovial joints) Classifications of Joints • Structural classification based on • Material that binds bones together • Presence or absence of a joint cavity • Structural classifications include • Fibrous • Cartilaginous • Synovial Fibrous Joints • Bones are connected by fibrous connective tissue • Do not have a joint cavity • Most are immovable or slightly movable • Types • Sutures • Syndesmoses • Gomphoses Sutures • Bones are tightly bound by a minimal amount of fibrous tissue • Only occur between the bones of the skull • Allow bone growth so the skull can expand with brain during childhood • Fibrous tissue ossifies in middle age • Synostoses—closed sutures Syndesmoses • Bones are connected exclusively by ligaments • Amount of movement depends on length of fibers • Tibiofibular joint—immovable synarthrosis • Interosseous membrane between radius and ulna • Freely movable diarthrosis Gomphoses • Tooth in a socket • Connecting ligament—the periodontal ligament Fibrous Joints Cartilaginous Joints • Bones are united by cartilage • Lack a joint cavity • Two types • Synchondroses • Symphyses Synchondroses • Hyaline cartilage unites bones • Epiphyseal plates • Joint between first rib and manubrium Symphyses • Fibrocartilage unites bones; resists tension and compression • Slightly movable joints that provide strength with flexibility • Intervertebral discs • Pubic symphysis • Hyaline cartilage—present as articular cartilage Symphyses Synovial Joints • Most movable type of joint • All are diarthroses • Each contains a fluid-filled joint cavity General Structure of Synovial Joints • Articular cartilage • Ends of opposing bones are covered with hyaline cartilage • Absorbs compression • Joint cavity (synovial cavity) • Unique to synovial joints • Cavity is a potential space that holds a small amount of synovial fluid General Structure of Synovial Joints • Articular capsule—joint cavity is enclosed in a two-layered capsule • Fibrous capsule—dense irregular connective tissue, which strengthens joint • Synovial membrane—loose connective tissue • Lines joint capsule and covers internal joint surfaces • Functions to make synovial fluid General Structure of Synovial Joints • Synovial fluid • A viscous fluid similar to raw egg white • A filtrate of blood • Arises from capillaries in synovial membrane • Contains glycoprotein molecules secreted by fibroblasts • Reinforcing ligaments • Often are thickened parts of the fibrous capsule • Sometimes are extracapsular ligaments—located outside the capsule • Sometimes are intracapsular ligaments—located internal to the capsule General Structure of Synovial Joints • Richly supplied with sensory nerves • Detect pain • Most monitor how much the capsule is being stretched General Structure of Synovial Joints • Have a rich blood supply • Most supply the synovial membrane • Extensive capillary beds produce basis of synovial fluid • Branches of several major nerves and blood vessels Synovial Joints with Articular Discs • Some synovial joints contain an articular disc • Occur in the temporomandibular joint and at the knee joint • Occur in joints whose articulating bones have somewhat different shapes 9 Joints How Synovial Joints Function • Synovial joints—lubricating devices • Friction could overheat and destroy joint tissue • Are subjected to compressive forces • Fluid is squeezed out as opposing cartilages touch • Cartilages ride on the slippery film Bursae and Tendon Sheaths • Bursae and tendon sheaths are not synovial joints • Closed bags of lubricant • Reduce friction between body elements • Bursa—a flattened fibrous sac lined by a synovial membrane • Tendon sheath—an elongated bursa that wraps around a tendon Bursae and Tendon Sheaths Movements Allowed by Synovial Joints • Three basic types of movement • Gliding—one bone across the surface of another • Angular movement—movements change the angle between bones • Rotation—movement around a bone's long axis Gliding Joints • Flat surfaces of two bones slip across each other • Gliding occurs between • Carpals • Articular processes of vertebrae • Tarsals Angular Movements • Increase or decrease angle between bones • Movements involve • Flexion and extension • Abduction and adduction • Circumduction Rotation • Involves turning movement of a bone around its long axis • The only movement allowed between atlas and axis vertebrae • Occurs at the hip and shoulder joints Rotation Special Movements • Elevation—lifting a body part superiorly • Depression—moving the elevated part inferiorly Special Movements • Protraction—nonangular movement anteriorly • Retraction—nonangular movement posteriorly Special Movements • Supination—forearm rotates laterally, palm faces anteriorly • Pronation—forearm rotates medially, palm faces posteriorly • Brings radius across the ulna Special Movements • Opposition—thumb moves across the palm to touch the tips of other fingers 9 Joints Special Movements • Inversion and eversion • Special movements at the foot • Inversion—turns sole medially • Eversion—turns sole laterally Special Movements Special Movements • Dorsiflexion and plantar flexion • Up-and-down movements of the foot • Dorsiflexion—lifting the foot so its superior surface approaches the shin • Plantar flexion—depressing the foot, elevating the heel Special Movements Synovial Joints Classified by Shape • Plane joint • Articular surfaces are flat planes • Short gliding movements are allowed • Intertarsal and intercarpal joints • Movements are nonaxial • Gliding does not involve rotation around any axis Plane Joint Synovial Joints Classified by Shape • Hinge joints • • • • Cylindrical end of one bone fits into a trough on another bone Angular movement is allowed in one plane Elbow, ankle, and joints between phalanges Movement is uniaxial—allows movement around one axis only Hinge Joint Synovial Joints Classified by Shape • Pivot joints • Classified as uniaxial – rotating bone only turns around its long axis • Examples • Proximal radioulnar joint • Joint between atlas and axis Pivot Joint Synovial Joints Classified by Shape • Condyloid joints • Allow moving bone to travel • Side to side—abduction-adduction • Back and forth—flexion-extension • Classified as biaxial—movement occurs around two axes Condyloid Joint Synovial Joints Classified by Shape • Saddle joints • Each articular surface has concave and convex surfaces • Classified as biaxial joints • 1st carpometacarpal joint is a good example • Allows opposition of the thumb Synovial Joints Classified by Shape 9 Joints Synovial Joints Classified by Shape • Ball-and-socket joints • Spherical head of one bone fits into round socket of another • Classified as multiaxial—allow movement in all axes • Shoulder and hip joints are examples Ball-and-Socket Joint Factors Influencing Stability of Synovial Joints • Articular surfaces • Shapes of articulating surfaces determine movements possible • Seldom play a major role in joint stability • Exceptions that do provide stability • Hip joint, elbow joint, and ankle Factors Influencing Stability of Synovial Joints • Ligaments • Capsules and ligaments prevent excessive motions • On the medial or inferior side of a joint – prevent excessive abduction • Lateral or superiorly located—resist adduction Factors Influencing Stability of Synovial Joints • Ligaments (continued) • Anterior ligaments—resist extension and lateral rotation • Posterior ligaments—resist flexion and medial rotation • The more ligaments, usually stronger and more stable Factors Influencing Stability of Synovial Joints • Muscle tone • Helps stabilize joints by keeping tension on tendons • Is important in reinforcing: • Shoulder and knee joints • Supporting joints in arches of the foot Selected Synovial Joints • Sternoclavicular joint • Is a saddle joint • Four ligaments surround the joint • Anterior and posterior sternoclavicular ligaments • Interclavicular ligament • Costoclavicular ligament • Performs multiple complex movements Selected Synovial Joints • Temporomandibular Joint • • • • Is a modified hinge joint The head of the mandible articulates with the temporal bone Lateral excursion is a side-to-side movement Two surfaces of the articular disc allow • Hinge-like movement • Gliding of superior surface anteriorly 9 Joints Selected Synovial Joints • Shoulder (glenohumeral) joint • The most freely movable joint lacks stability • Articular capsule is thin and loose • Muscle tendons contribute to joint stability Glenohumeral Joint Glenohumeral Joint • The rotator cuff is made up of four muscles and their associated tendons • • • • Subscapularis Supraspinatus Infraspinatus Teres minor • Rotator cuff injuries are common shoulder injuries The Shoulder Joint The Shoulder Joint Selected Synovial Joints • Elbow joint • Allows flexion and extension • The humerus’ articulation with the trochlear notch of the ulna forms the hinge • Tendons of biceps and triceps brachii provide stability Wrist Joint • Stabilized by numerous ligaments • Composed of radiocarpal and intercarpal joint • Radiocarpal joint—joint between the radius and proximal carpals (the scaphoid and lunate) • Allows for flexion, extension, adduction, abduction, and circumduction • Intercarpal joint—joint between the proximal and distal rows or carpals • Allows for gliding movement Selected Synovial Joints • Hip joint • A ball-and-socket structure • Movements occur in all axes • Limited by ligaments and acetabulum • Head of femur articulates with acetabulum • Stability comes chiefly from acetabulum and capsular ligaments • Muscle tendons contribute somewhat to stability Selected Synovial Joints • Knee joint • • • • • • The largest and most complex joint Primarily acts as a hinge joint Has some capacity for rotation when leg is flexed Structurally considered compound and bicondyloid Two fibrocartilage menisci occur within the joint cavity Femoropatellar joint—shares the joint cavity • Allows patella to glide across the distal femur Knee Joint • Capsule of the knee joint • Covers posterior and lateral aspects of the knee • Covers tibial and femoral condyles • Does not cover the anterior aspect of the knee • Anteriorly covered by three ligaments • Patellar ligament • Medial and lateral patellar retinacula Anterior View of Knee Knee Joint • Ligaments of the knee joint • Become taut when knee is extended • These extracapsular and capsular ligaments are • Fibular and tibial collateral ligament • Oblique popliteal ligament • Arcuate popliteal ligament Posterior View of Knee Joint Knee Joint • Intracapsular ligaments • Cruciate ligaments • Cross each other like an ―X‖ • Each cruciate ligament runs from the proximal tibia to the distal femur • Anterior cruciate ligament • Posterior cruciate ligament Anterior View of Flexed Knee Knee Joint • Intracapsular ligaments • Cruciate ligaments—prevent undesirable movements at the knee • Anterior cruciate ligament—prevents anterior sliding of the tibia • Posterior cruciate ligament—prevents forward sliding of the femur or backward displacement of the tibia Stabilizing function of cruciate ligaments The “Unhappy Triad” • Lateral blows to the knee can tear: • Tibial collateral ligament and medial meniscus • Anterior cruciate ligament The “Unhappy Triad” Selected Synovial Joint • Ankle joint • A hinge joint between • United inferior ends of tibia and fibula • The talus of the foot • Allows the movements • Dorsiflexion and plantar flexion only The Ankle Joint • Medially and laterally stabilized by ligaments • Medial (deltoid) ligament • Lateral ligament • Inferior ends of tibia and fibula are joined by ligaments • Anterior and posterior tibiofibular ligaments Disorders of Joints • Structure of joints makes them prone to traumatic stress • Function of joints makes them subject to friction and wear • Affected by inflammatory and degenerative processes Joint Injuries • Torn cartilage—common injury to meniscus of knee joint • Sprains—ligaments of a reinforcing joint are stretched or torn • Dislocation—occurs when the bones of a joint are forced out of alignment Inflammatory and Degenerative Conditions • Bursitis—inflammation of a bursa due to injury or friction • Tendonitis—inflammation of a tendon sheath Inflammatory and Degenerative Conditions • Arthritis—describes over 100 kinds of joint-damaging diseases • Osteoarthritis—most common type of ―wear and tear‖ arthritis • Rheumatoid arthritis—a chronic inflammatory disorder • Gouty arthritis (gout)—uric acid build-up causes pain in joints • Lyme disease—inflammatory disease often resulting in joint pain The Joints Throughout Life • Synovial joints develop from mesenchyme • By Week 8 of fetal development, joints resemble adult joints • Outer region of mesenchyme becomes fibrous joint capsule • Inner region becomes the joint cavity The Joints Throughout Life • During youth—injury may tear an epiphysis off a bone shaft • Advancing age—osteoarthritis becomes more common • Exercise—helps maintain joint health 10 Muscle Tissue Muscle • Muscle—a Latin word for ―little mouse‖ • Muscle is the primary tissue in the: • Heart (cardiac MT) • Walls of hollow organs (smooth MT) • Skeletal muscle • Makes up nearly half the body’s mass Overview of Muscle Tissue • Functions of muscle tissue • Movement • Skeletal muscle—attached to skeleton • Moves body by moving the bones • Smooth muscle—squeezes fluids and other substances through hollow organs Overview of Muscle Tissue • Functions of muscle tissue (continued) • Maintenance of posture—enables the body to remain sitting or standing • Joint stabilization • Heat generation • Muscle contractions produce heat • Helps maintain normal body temperature Functional Features of Muscles • Functional features • Contractility • Long cells shorten and generate pulling force • Excitability • Electrical nerve impulse stimulates the muscle cell to contract • Extensibility • Can be stretched back to its original length by contraction of an opposing muscle • Elasticity • Can recoil after being stretched Types of Muscle Tissue • Skeletal muscle tissue • Packaged into skeletal muscles • Makes up 40% of body weight • Cells are striated Types of Muscle Tissue • Cardiac muscle tissue—occurs only in the walls of the heart • Smooth muscle tissue—occupies the walls of hollow organs • Cells lack striations Similarities of Muscle Tissue • Cells of smooth and skeletal muscle • Are known as fibers • Muscle contraction • Depends on two types of myofilaments (contractile proteins) • One type contains actin • Another type contains myosin • These two proteins generate contractile force Similarities of Muscle Tissues • Plasma membrane is called a sarcolemma • Cytoplasm is called sarcoplasm Skeletal Muscle • Each muscle is an organ • Consists mostly of muscle tissue • Skeletal muscle also contains • Connective tissue • Blood vessels • Nerves Basic Features of a Skeletal Muscle • Connective tissue and fascicles • Sheaths of connective tissue bind a skeletal muscle and its fibers together • Epimysium—dense regular connective tissue surrounding entire muscle • Perimysium—surrounds each fascicle (group of muscle fibers) • Endomysium—a fine sheath of connective tissue wrapping each muscle cell Basic Features of a Skeletal Muscle • Connective tissue sheaths are continuous with tendons • When muscle fibers contract, pull is exerted on all layers of connective tissue are tendon • Sheaths provide elasticity and carry blood vessels and nerves Connective Tissue Sheaths in Skeletal Muscle Basic Features of a Skeletal Muscle • Nerves and blood vessels • Each skeletal muscle supplied by branches of • One nerve • One artery • One or more veins Basic Features of a Skeletal Muscle • Nerves and blood vessels (continued) • Nerves and vessels branch repeatedly • Smallest nerve branches serve: • Individual muscle fibers • Neuromuscular junction—signals the muscle to contract Basic Features of a Skeletal Muscle • Muscle attachments • Most skeletal muscles run from one bone to another • One bone will move, other bone remains fixed • Origin—less movable attachment • Insertion—more movable attachment Basic Features of a Skeletal Muscle • Muscle attachments (continued) • Muscles attach to origins and insertions by CT • Fleshy attachments—CT fibers are short • Indirect attachments—CT forms a tendon or aponeurosis • Bone markings present where tendons meet bones • Tubercles, trochanters, and crests Microscopic and Functional Anatomy of Skeletal Muscle Tissue • The skeletal muscle fiber • Fibers are long and cylindrical • Are huge cells—diameter is 10–100µm • Length—several centimeters to dozens of centimeters • Each cell formed by fusion of embryonic cells • Cells are multinucleate • Nuclei are peripherally located Diagram of Part of a Muscle Fiber Myofibrils and Sarcomeres • Striations result from internal structure of myofibrils • Myofibrils • • • • Are long rods within cytoplasm Make up 80% of the cytoplasm Are a specialized contractile organelle found in muscle tissue Are a long row of repeating segments called sarcomeres (functional unit of Skeletal MT) Sarcomere • Basic unit of contraction of skeletal muscle • Z disc (Z line)—boundaries of each sarcomere • Thin (actin) filaments—extend from Z disc toward the center of the sarcomere • Thick (myosin) filaments—located in the center of the sarcomere • Overlap inner ends of the thin filaments • Contain ATPase enzymes Sarcomere Structure • A bands—full length of the thick filament • Includes inner end of thin filaments • H zone—center part of A band where no thin filaments occur • A bands and I bands refract polarized light differently • A bands—anisotropic • I bands—isotropic Sarcomere Structure (continued) • M line—in center of H zone • Contains tiny rods that hold thick filaments together • I band—region with only thin filaments • Lies within two adjacent sarcomeres Sarcomere Structure (continued) Sarcoplasmic Reticulum and T Tubules • Sarcoplasmic reticulum • A specialized smooth ER • Interconnecting tubules surround each myofibril • Some tubules form cross-channels called terminal cisternae • Cisternae occur in pairs on either side of a t tubule Sarcoplasmic Reticulum and T Tubules • Sarcoplasmic reticulum • Contains calcium ions—released when muscle is stimulated to contract • Calcium ions diffuse through cytoplasm • Trigger the sliding filament mechanism • T tubules—deep invaginations of sarcolemma • Triad—T tubule flanked by two terminal cisterns Mechanism of Contraction • Two major types of contraction • Concentric contraction—muscle shortens to do work • Eccentric contraction—muscle generates force as it lengthens • Muscle acts as a ―brake‖ to resist gravity • ―Down‖ portion of a pushup is an example Mechanism of Contraction • Sliding filament mechanism • Explains concentric contraction • Myosin head attach to thin filaments at both ends of a sarcomere • Then pull thin filaments toward the center of the sarcomere • Thin and thick filaments do not shorten • Initiated by release of calcium ions from the SR • Powered by ATP Sliding Filament Mechanism • Contraction changes the striation pattern • Fully relaxed—thin filaments partially overlap thin filaments • Contraction—Z discs move closer together • Sarcomere shortens • I bands shorten, H zone disappears • A band remains the same length Microscopic and Functional Anatomy of Skeletal Muscle Tissue • Muscle extension • Muscle is stretched by a movement opposite that which contracts it • Muscle fiber length and force of contraction • Greatest force produced when a fiber starts out slightly stretched • Myosin heads can pull along the entire length of the thin filaments The Role of Titin • Titin—a spring-like molecule in sarcomeres • Resists overstretching • Holds thick filaments in place • Unfolds when muscle is stretched Innervation of Skeletal Muscle • Motor neurons innervate skeletal muscle tissue • Neuromuscular junction is the point where nerve ending and muscle fiber meet • Axon terminals—at ends of axons • Store neurotransmitters • Synaptic cleft—space between axon terminal and sarcolemma The Neuromuscular Junction Motor Units 10 Muscle Tissue Types of Skeletal Muscle Fibers • Skeletal muscle fibers are categorized according to two characteristics • How they manufacture energy (ATP) • How quickly they contract • Oxidative fibers—produce ATP aerobically • Glycolytic fibers—produce ATP anaerobically by glycolysis Types of Skeletal Muscle Fibers • Skeletal muscle fibers • Are divided into three classes • Slow oxidative fibers • Red slow oxidative fibers • Fast glycolytic fibers • White fast glycolytic fibers • Fast oxidative fibers • Intermediate fibers Types of Skeletal Muscle Fibers • Slow oxidative fibers • • • • • • Red color due to abundant myoglobin Obtain energy from aerobic metabolic reactions Contain a large number of mitochondria Richly supplied with capillaries Contract slowly and resistant to fatigue Fibers are small in diameter Types of Skeletal Muscle Fibers • Fast glycolytic fibers • • • • • Contain little myoglobin and few mitochondria About twice the diameter of slow-oxidative fibers Contain more myofilaments and generate more power Depend on anaerobic pathways Contract rapidly and tire quickly Types of Skeletal Muscle Fibers • Fast oxidative fibers • • • • • • Have an intermediate diameter Contract quickly like fast glycolytic fibers Are oxygen-dependent Have high myoglobin content and rich supply of capillaries Somewhat fatigue-resistant More powerful than slow oxidative fibers Disorders of Muscle Tissue • Muscle tissues experience few disorders • Heart muscle is the exception • Skeletal muscle • Remarkably resistant to infection • Smooth muscle • Problems stem from external irritants Disorders of Muscle Tissue • Muscular dystrophy • A group of inherited muscle destroying disease • Affected muscles enlarge with fat and connective tissue • Muscles degenerate • Types of muscular dystrophy • Duchenne muscular dystrophy • Myotonic dystrophy Disorders of Muscle Tissue • Myofascial pain syndrome • Pain is caused by tightened bands of muscle fibers • Fibromyalgia • A mysterious chronic-pain syndrome • Affects mostly women • Symptoms—fatigue, sleep abnormalities, severe musculoskeletal pain, and headache Muscle Tissue Throughout Life • Muscle tissue develops from myoblasts • Myoblasts fuse to form skeletal muscle fibers • Skeletal muscles contract by the seventh week of development Muscle Tissue Throughout Life • Cardiac muscle • Pumps blood three weeks after fertilization • Satellite cells • Surround skeletal muscle fibers • Resemble undifferentiated myoblasts • Fuse into existing muscle fibers to help them grow Muscle Tissue Throughout Life • With increased age • Amount of connective tissue increases in muscles • Number of muscle fibers decreases • Loss of muscle mass with aging • Decrease in muscular strength is 50% by age 80 • Sarcopenia—muscle wasting 11 Muscles of the Body Muscles of the Body • Skeletal muscles • Produce movements • Blinking of eye, standing on tiptoe, swallowing food, etc. • General principles of leverage • Muscles act with or against each other • Criteria used in naming muscles Arrangement of Fascicles in Muscles • Skeletal muscles—consist of fascicles • Fascicles—arranged in different patterns • Fascicle arrangement—tells about action of a muscle Arrangement of Fascicles in Muscles • Types of fascicle arrangement • Parallel—fascicles run parallel to the long axis of the muscle • Strap-like—sternocleidomastoid • Fusiform—biceps brachii Arrangement of Fascicles in Muscles • Types of fascicle arrangement • Convergent • Origin of the muscle is broad • Fascicles converge toward the tendon of insertion • Example—pectoralis major Arrangement of Fascicles in Muscles • Types of fascicle arrangement • Pennate • Unipennate—fascicles insert into one side of the tendon • Bipennate—fascicles insert into the tendon from both sides • Multipennate—fascicles insert into one large tendon from all sides Arrangement of Fascicles in Muscles • Circular • Fascicles are arranged in concentric rings • Surround external body openings • Sphincter—general name for a circular muscle • Examples • Orbicularis oris and orbicularis oculi Lever Systems: Bone-Muscle Relationships • Movement of skeletal muscles involves leverage • • • • Lever—a rigid bar that moves Fulcrum—a fixed point Effort—applied force Load—resistance Lever Systems: Bone-Muscle Relationships • Bones—act as levers • Joints—act as fulcrums • Muscle contraction—provides effort • Applies force where muscle attaches to bone • Load—bone, overlying tissue, and anything lifted Lever Systems: Bone-Muscle Relationships • Levers allow a given effort to • Move a heavier load • Move a load farther • Mechanical advantage • Moves a large load over small distances • Mechanical disadvantage • Allows a load to be moved over a large distance Lever Systems: Bone-Muscle Relationships • First-class lever • Effort applied at one end • Load is at the opposite end • Fulcrum is located between load and effort Lever Systems: Bone-Muscle Relationships • Examples—seesaws, scissors, and lifting your head off your chest Lever Systems: Bone-Muscle Relationships • Second-class lever • • • • Effort applied at one end Fulcrum is at the opposite end Load is between the effort and fulcrum Examples—wheelbarrow or standing on tiptoe • An uncommon type of lever in the body • Work at a mechanical advantage Lever Systems: Bone-Muscle Relationships • Third-class lever • Effort is applied between the load and the fulcrum • Work speedily • Always at a mechanical disadvantage Lever Systems: Bone-Muscle Relationships • Most skeletal muscles are third-class levers • Example—biceps brachii • Fulcrum—the elbow joint • Force—exerted on the proximal region of the radius • Load—the distal part of the forearm Organization Scheme Based on Embryonic Development • Overview based on • Embryonic origin • General function • Muscles develop from mesoderm • Myotomes • Somitomeres • The first seven myotomes of the head • Splanchnic mesoderm Development and Basic Organization of the Muscles Organization Scheme Based on Embryonic Development • Muscles organized into four groups • • • • Musculature of the visceral organs Pharyngeal arch muscles Axial muscles Limb muscles Organization Scheme Based on Embryonic Development • Musculature of the visceral organs • Includes smooth and cardiac muscle • Develops from splanchnic mesoderm • Pharyngeal arch muscles • Includes • Skeletal muscles of the pharynx • Muscles of the head and neck • Develop from the fourth to seventh somitomeres Pharyngeal Arch Muscles Axial Muscles • Lie anterior and posterior to the body axis • Muscles of the • Thorax, abdomen, and pelvis • Many muscles of the • Neck and some of the head • Function to move the trunk and maintain posture Axial Muscles • Develop from myotomes and some somitomeres • Dorsal regions of myotomes—deep muscles of the back • Ventral regions of myotomes—muscles of the trunk and neck • Respiratory muscles • Anterior abdominal wall muscles • Muscles of the pelvic floor Axial Muscles Limb Muscles • Limb muscles arise from lateral parts of nearby myotomes • Extensors • Muscle mass dorsal to limb bones • Flexors • Muscle mass ventral to limb bones Limb Muscles Muscle Actions and Interactions • A muscle cannot reverse the movement it produces • Another muscle must undo the action • Muscles with opposite actions lie on opposite sides of a joint Muscle Actions and Interactions • Prime mover (agonist) • Has major responsibility for a certain movement • Antagonist • Opposes or reverses a movement • Synergist—helps the prime mover • By adding extra force • By reducing undesirable movements • Fixator • A type of synergist that holds a bone firmly in place Muscle Compartments of the Limbs • Dense fibrous connective tissue divides limb muscles into compartments • Muscles in opposing compartments are • Agonist and antagonist pairs • Each compartment is innervated by a single nerve Muscle Compartments of Arm and Forearm • The upper limb has anterior and posterior compartments • Anterior arm compartment muscles • Flex the shoulder or arm • Innervation is the musculocutaneous nerve • Anterior forearm compartment muscles • Flex the wrist and digits • Innervation is the median or ulnar nerve Muscle Compartments of the Thigh • Posterior compartment muscles • Extend the hip and flex the knee • Innervation is the tibial branch of the sciatic nerve • Anterior compartment muscles • Flex the hip and extend the knee • Innervation is the femoral nerve • Medial compartment • Adduct the thigh • Innervation is the obturator nerve Muscle Compartments of the Thigh and Leg Compartments of the Leg • Posterior compartment muscles • Contains digital and plantar flexors • Innervation is the tibial nerve • Anterior compartment muscles • Contains digital extensors and dorsiflexors • Innervation is the deep fibular nerve • Lateral compartment muscles • Plantar flex and evert the foot • Innervation is the superficial fibular nerve Naming the Skeletal Muscles • Location • Example—the brachialis is located on the arm • Shape • Example—the deltoid is triangular • Relative size • Maximus, minimus, and longus indicate size • Example—gluteus maximus and gluteus minimus Naming the Skeletal Muscles • Direction of fascicles and muscle fibers • Name tells direction in which fibers run • Example—rectus abdominis and transversus abdominis • Location of attachments—name reveals point of origin and insertion • Example—brachioradialis Naming the Skeletal Muscles • Number of origins • Two, three, or four origins • Indicated by the words biceps, triceps, and quadriceps • Action • The action is part of the muscle’s name • Indicates type of muscle movement • Flexor, extensor, adductor, or abductor 11 Muscles of the Body Superficial Muscles of the Body—Anterior View Superficial Muscles of the Body—Posterior View Muscles of the Head—Facial Expression • Muscles of facial expression • • • • Lie in the face and scalp Thin and variable in shape Often insert in the skin—not on bones Innervated by cranial nerve VII—the facial nerve Muscles of the Head—Facial Expression Muscles Mastication and Tongue Movement • Four main pairs of muscles involved in mastication • Innervated by mandibular division of the trigeminal nerve (cranial nerve V) • Prime movers of jaw closure • Masseter and temporalis • Side-to-side movement • Pterygoid muscles • Compression of cheeks • Buccinator muscles Muscles Mastication and Tongue Movement • Extrinsic muscles of the tongue • Move tongue • Laterally • Anteriorly • Posteriorly • All innervated by cranial nerve XII—the hypoglossal nerve Muscles of the Anterior Neck and Throat—Swallowing • The neck is divided into anterior and posterior triangles • Anterior triangle • Divided into suprahyoid and infrahyoid muscles • Participate in swallowing • Pharyngeal constrictors • Squeeze food into the esophagus Muscles of the Neck and Vertebral Column • Head movement • Sternocleidomastoid • Splenius capitis and splenius cervicis Muscles of the Neck and Vertebral Column • Trunk extension • Deep muscles of the back • Maintain normal curvatures of the spine • Form a column from sacrum to the skull • Erector spinae group • Largest of the deep back muscles Deep Muscles of the Thorax—Breathing • Deep muscles provide movements for breathing • External intercostal muscles • Lift the rib cage • Internal intercostal muscles • Aid expiration during heavy breathing Deep Muscles of the Thorax—Breathing • Diaphragm • Most important muscle of respiration • Flattens as it contracts • Increases the volume of the thoracic cavity Muscles of the Abdominal Wall • Lateral and anterior abdominal wall • Formed from three flat muscle sheets • External oblique • Internal oblique • Transversus abdominis • Fourth muscle pair • Rectus abdominis • Inserts at the linea alba Muscles of the Pelvic Floor • Pelvic floor (pelvic diaphragm) • Sheet of two muscles • Both support pelvic organs • Levator ani • Formed from iliococcygeus, puborectalis, and pubococcygeus • Coccygeus Muscles of the Pelvic Floor Muscles of the Perineum • Inferior to the muscles of the pelvic floor • Urogenital diaphragm formed from: • Sphincter urethrae and the deep transverse perineus Muscles of the Perineum • Muscles of the superficial perineal space • Ischiocavernosus • Bulbospongiosus • Superficial transverse perineus Muscles of the Perineum Superficial Muscles of the Anterior Thorax • Movements of the scapula • • • • Pectoralis major Pectoralis minor Serratus anterior Subclavius Superficial Muscles of the Posterior Thorax • Movements of the scapula • • • • Trapezius Levator scapulae Rhomboid major Rhomboid minor Muscles Crossing the Shoulder Joint • Movements of the arm • Deltoid • Pectoralis major Muscles Crossing the Elbow Joint • Posterior muscles—extensors of the forearm • Triceps brachii • Anconeus • Anterior muscles—flexors of the forearm • Biceps brachii—also supinates the forearm • Brachialis • Brachioradialis Muscles of the Forearm • Movements of the wrist, hand, and fingers • Tendons are anchored by • Flexor and extensor retinacula • Most forearm muscles arise from the distal humerus • Movements at the wrist include • Flexion, extension, abduction, and adduction • Wrist and fingers are ―operated‖ by muscles in the forearm Muscles of the Forearm • Flexors • Anterior flexor compartment • Innervated by median and ulnar nerves • Originate from a common tendon • Medial epicondyle of the humerus Superficial Anterior Muscles of the Forearm • Pronator teres • Flexor carpi radialis • Palmaris longus • Flexor carpi ulnaris • Flexor digitorum superficialis Deep Anterior Muscles of the Forearm • Flexor pollicis longus • Flexor digitorum profundus • Pronator quadratus Deep Anterior Muscles of the Forearm Muscles of the Forearm • Extensors • Posterior compartment of the forearm • Innervated by the radial nerve • Originate at a common tendon • Lateral epicondyle of the humerus Superficial Posterior Muscles of the Forearm • Brachioradialis—flexes forearm • Extensor carpi radialis longus • Extensor carpi radialis brevis • Extensor digitorum • Extensor carpi ulnaris Deep Posterior Muscles of the Forearm • Supinator • Abductor pollicis longus • Extensor pollicis brevis and longus • Extensor indicus Intrinsic Muscles of the Hand • Fine movement of the fingers • All located in the palm • Control precise movements • Include muscles of • Adduction, abduction, and opposition Intrinsic Muscles of the Hand • Thenar muscles—ball of thumb • • • • Abductor pollicis brevis Flexor pollicis brevis Opponens pollicis Adductor pollicis • Hypothenar muscles • Abductor digiti minimi • Flexor digiti minimi • Opponens pollicis Intrinsic Muscles of the Hand Intrinsic Muscles of the Hand • Midpalmar muscles • Lumbricals • Palmar interossei • Dorsal interossei Intrinsic Muscles of the Hand Muscles Crossing the Hip and Knee Joints • Thigh and leg movements • Anterior muscles • Flex the thigh and extend the leg at the knee • Posterior muscles • Extend the thigh and flex the leg Muscles Crossing the Hip and Knee Joints • Thigh and leg movements • Adductor muscles—on medial aspect of thigh • Adduct the thigh only • Deep fascia of the thigh • Surrounds and encloses all three groups Muscles Crossing the Hip and Knee Joints • Movements at the hip joint • Muscles that flex the thigh • Originate on vertebral column or pelvis • Muscles that extend the thigh • Arise posterior to the hip joint • Adductors originate medial to the hip joint • Abductors originate lateral to the hip joint Anterior and Medial Muscles • Origin on pelvis or vertebral column • Iliacus • Psoas major • Sartorius • Muscles of the medial compartment • • • • • Adductor longus Adductor brevis Adductor magnus Pectineus Gracilis Anterior and Medial Muscles Muscles of the Anterior Compartment of the Thigh • Quadriceps femoris • Has four separate heads • Has a common insertion at the quadriceps tendon • Powerful knee extensors • Rectus femoris • Vastus lateralis • Vastus medialis • Vastus intermedius • Tensor fasciae latae Muscles of the Anterior Compartment of the Thigh Posterior Muscles • Origin on pelvis or sacrum • Gluteus maximus • Gluteus medius • Gluteus minimus • Lateral rotators • Piriformis • Obturator externus • Obturator internus • Superior and inferior gemellus • Quadratus femoris Posterior Muscles Muscles of the Posterior Compartment of the Thigh • Hamstrings • Biceps femoris • Semitendinosus • Semimembranosus Muscles of the Leg • Fascia lata of the leg surrounds muscles • • • • Tightly binds muscles Prevents swelling during exercise Aids venous return Divides leg into three compartments • Tendons are held in place by • Extensor, fibular, and flexor retinacula • Muscle movement at ankle and intertarsal joints Muscles of the Anterior Compartment • Tibialis anterior • Extensor digitorum longus • Fibularis tertius • Extensor hallucis longus Muscles of the Lateral Compartment • Fibularis longus • Fibularis brevis • Flexor hallucis longus • Extensor hallucis longus • Fibularis tertius Muscles of the Posterior Compartment • Superficial muscles • Triceps surae • Gastrocnemius • Soleus • Plantaris Muscles of the Posterior Compartment • Deep muscles • • • • Popliteus Flexor digitorum longus Flexor hallucis longus Tibialis posterior Intrinsic Muscles of the Foot • Toe movement and foot support • • • • Help to flex, extend, abduct, and adduct the toes Support the arches of the foot Single muscle on dorsal aspect of the foot Many muscles on the plantar aspect Muscles of the Foot • Muscle on the dorsum of the foot • Extensor digitorum brevis • Muscles on the sole of the foot • First layer • Flexor digitorum brevis • Abductor hallucis • Abductor digiti minimi Muscles of the Foot • Second layer • Flexor accessorius • Lumbricals Muscles of the Foot • Third layer • Flexor hallucis brevis • Adductor hallucis • Flexor digiti minimi brevis • Fourth layer • Plantar and dorsal interossei Muscles of the Foot Surface Anatomy • Palpation—feeling internal structures through the skin • ―Living anatomy‖—provides information about • • • • Palpation of arterial pulses Skeleton, muscles, and blood vessels Sounds of the heart and lungs Where to give injections The Head • Cranium—selected structures felt through the skin • • • • • Superciliary arches External occipital protuberance Mastoid process Temporalis muscle—at temple region Frontalis muscle • Feel wrinkling of the forehead when eyebrows are raised Surface Anatomy of Lateral Aspect of the Head The Head • Face—selected structures felt through the skin • • • • • • • Lacrimal fossa Root and bridge of the nose Auricle of the ear Zygomatic arch Masseter muscle Mandible Temporomandibular joint The Neck • Skeletal landmarks • Spinous processes of cervical vertebrae • • • • • C7 is particularly prominent (vertebra prominens) Hyoid bone—in the anterior superior neck Laryngeal prominence—the ―Adam’s Apple‖ Cricoid cartilage—inferior to the laryngeal prominence Jugular notch—depression in the superior part of the sternum The Neck Muscles of the Neck • Sternocleidomastoid—most prominent neck muscle • Sternal head • Clavicular head • Deep to the sternocleidomastoid • Common carotid artery • Internal jugular vein • Trapezius—posterior aspect of the neck Triangles of the Neck • The sternocleidomastoid muscles divide the neck • Anterior triangle • Posterior triangle The Thorax • Sternum—portions felt through the skin • Manubrium, xiphoid process, and sternal angle • Midaxillary line—line from the center of the axilla onto the lateral thoracic wall • Midclavicular line—vertical line from midpoint of the clavicle to the groin Muscles of the Thorax • Pectoralis major • Serratus anterior The Anterior Thorax and Abdomen The Abdomen • Structures felt through the skin • Iliac crest • Anterior superior iliac spine • Inguinal ligament • Runs medially from anterior superior iliac spine to the pubic tubercle • Pubic crest Muscles and other Abdominal Surface Features • Linea alba • The ―white line‖ extending from xiphoid process to the pubic symphysis • Rectus abdominis • Linea semilunaris—lateral margin of rectus abdominis The Pelvis and Perineum • Four bony structures define the perineum • Pubic symphysis • Two ischial tuberosities • Coccyx The Back • Posterior median furrow—vertical groove along the midline • Spinous processes of vertebrae • Spine of the scapula • Medial end is opposite T3 • Medial border of the scapula The Back • Inferior angle of the scapula • Iliac crests • Supracristal line—intersects L4 • Sacrum—superior to cleft in the buttocks • Coccyx—posterior to the anus Surface Anatomy of the Back Muscles of the Back • Trapezius • Latissimus dorsi • Erector spinae Surface Anatomy of the Back Upper Limb and Shoulder • The axilla • • • • Base of the axilla—where armpit hair grows Deep to the axilla—axillary lymph nodes and blood vessels Anterior axillary fold—pectoralis major Posterior axillary fold—latissimus dorsi and teres major Shoulder and Arm The Shoulder • Acromion—lateral end of the spine of the scapula • Acromioclavicular joint • Deltoid muscle • Covers the greater tubercle of the humerus The Arm • The region between the shoulder and elbow • Humerus • Palpated through skin along its entire length • Biceps brachii • Medial bicipital groove • The medial boundary of the biceps brachii • Triceps brachii The Arm The Elbow • Lateral and medial epicondyles of the humerus • Ulnar nerve—―funny bone‖ runs across medial epicondyle • Olecranon process of the ulna • Cubital fossa—(antecubital fossa) • Forms anterior surface of forearm The Anterior Surface of the Forearm and Fist Forearm • Bones • Ulna—palpate entire length • Styloid process and head—distal end • Radius—partly covered in muscle • Head of the radius—proximal end • Styloid process—distal end Muscles of the Forearm • Flexor muscles—anterior forearm • Flexor carpi radialis • Palmaris longus • This muscle is absent in about 30% of people • Extensor muscles—posterior forearm Muscles of the Forearm Other Structures of the Forearm • Anatomical snuff box bordered by • Extensor pollicis brevis • Extensor pollicis longus The Hand • Dorsum of hand • Dorsal venous network • Tendons of extensor digitorum Gluteal Region • Iliac crests • Posterior superior iliac spine • Sacroiliac joint • Prominences of the buttocks • ―Cheeks‖ of the buttocks • Formed from subcutaneous fat and the gluteal muscles The Gluteal Region Lower Limb and Gluteal Region • Natal cleft (gluteal cleft) • Vertical midline groove between ―cheeks‖ • Gluteal fold • Horizontal fold below each ―cheek‖ • Ischial tuberosities • Greater trochanter of the femur • Located at the lateral hip Lower Limb and Gluteal Region Thigh • Medial and lateral condyles of the femur • Patella • Three groups of muscles • Quadriceps femoris—anterior thigh • Vastus lateralis—injection site • Adductors—medial thigh • Hamstrings—posterior thigh Thigh The Thigh • The femoral triangle • Superior border—inguinal ligament • Inferior borders • Sartorius • Adductor longus • Popliteal fossa • Diamond-shaped hollow on posterior knee • Defined by borders of ―hamstring‖ tendons and gastrocnemius Leg and Foot • Palpate patella to find the patellar ligament • Structures of the proximal leg • Tibial tuberosity • Lateral and medial condyles of the tibia • Head of the fibula • Structures of the distal leg • Medial malleolus • Lateral malleolus Leg and Foot Muscle Groups of the Leg • Posterior calf muscles • Gastrocnemius and soleus • Calcaneal tendon—inferior end of the soleus and gastrocnemius • Anterior compartment muscles • Tibialis anterior • Extensor digitorum • Fibularis Muscle Groups of the Leg Foot • Tendons on the dorsal surface of the foot • Extensor digitorum longus tendon • Extensor hallucis longus