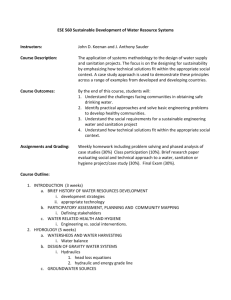
table of contents
advertisement

` EFFECTIVENESS OF SANITATION AND HYGIENE INTERVENTIONS IN CHANGING MOTHERS’ BEHAVIOUR AND IMPROVING CHILD HEALTH IN TURKANA DISTRICT KENYA JOHN GACHUKI KARIUKI DOCTOR OF PHILOSOPHY (Public Health) JOMO KENYATTA UNIVERSITY OF AGRICULTURE AND TECHNOLOGY 2013 ` Effectiveness of sanitation and hygiene interventions in changing mothers’ behaviour and improving child health in Turkana District, Kenya. John Gachuki Kariuki A thesis submitted in partial fulfilment for the degree of Doctor of Philosophy in Public Health in the Jomo Kenyatta University of Agriculture and Technology 2013 DECLARATION This thesis is my original work and has not been presented for a degree in any other university or institution. Signature……………………… John Gachuki Kariuki Date……………………. DECLARATION BY SUPERVISORS This thesis has been submitted for examination with our approval as University Supervisors. Signature……………………… Prof. Japhet K. Magambo (Ph.D) JKUAT, Kenya. Date……………………. Signature……………………… Prof. Francis M. Njeruh (Ph.D) JKUAT, Kenya. Date……………………. Signature……………………… Dr. Samuel Kariuki (Ph.D) KEMRI, Kenya. Date……………………. Signature……………………… Date……………………. Dr. Eric M. Muchiri (Ph.D) Ministry of Public Health and Sanitation, Kenya. ii DEDICATION The work is dedicated to my wife Margaret, children (Kenneth, Lysbeth, Ann and Peter) and to all Public Health Practitioners worldwide. iii ACKNOWLEDGEMENT I wish to extend my acknowledgments to various persons and institutions for the contributions they made towards completion of this work. First, I thank the Ministry of Public Health and Sanitation through the Chief Public Health Officer for accepting to pay my tuition fees and the Directorate of Personnel Management (DPM) for granting me course approval and study leave. Secondly, I thank my four supervisors, Prof. Japhet K. Magambo, Prof. Francis M. Njeruh, Dr. Samuel Kariuki and Dr. Eric M. Muchiri, for finding time and according me good supervision, during our many meetings and discussions throughout the study period, and for coming to the field to oversee my field research. Thirdly, I thank the United Nations Children’s Fund (UNICEF) Kenya Country office through Eng. Fredrick Donde for their financial and logistical support for the field work. I also thank Mr. Bore and acknowledge the support from the National Bureau of Statistics for identification, mapping and listing of population study clusters. Equally, I cannot forget to acknowledge Dr. Joseph Karemi; the Medical Officer of Health Turkana District, and Dr. Eric J. Ahomo; the Medical Superintendent Lodwar District hospital who allowed to me to use their facilities, and their staff; namely Innocent Munyefu Sifuna, Chrysantus Ahindukha Lirhunde, Alfred Ikenyi Emanman, iv Scholastica L . Ekorot, Julia A. Akorilem and Daniel Esimit, who assisted in the field work. In addition, I also wish to thank Dr. Samuel Kariuki of Kenya Medical Research Institute (KEMRI) and their staff Ayub Ongechi and Peter Mbogo for assisting in laboratory analysis of study specimen. Finally I am greatly indebted to the heads of the house-holds who allowed me access to their compounds to conduct general hygiene and sanitation inspection, interview mothers of children less than five years of age, from whom I collected stool specimens from their children and water samples from their storage containers for microbiological test. v TABLE OF CONTENTS DECLARATION ......................................................................................................................... ii DEDICATION ............................................................................................................................ iii ACKNOWLEDGEMENT ......................................................................................................... iv TABLE OF CONTENTS ........................................................................................................... vi LIST OF TABLES ..................................................................................................................... ix LIST OF FIGURES .................................................................................................................... x LIST OF APPENDICES ............................................................................................................ xi LIST OF ABBREVIATIONS AND ACRONYMS................................................................. xii OPERATIONAL DEFINITIONS ........................................................................................... xiv ABSTRACT ............................................................................................................................... xv CHAPTER ONE .......................................................................................................................... 1 1.0 INTRODUCTION ........................................................................................................... 1 1.1 Background ................................................................................................................... 1 1.2 Problem Statement ........................................................................................................ 2 1.3 Study Justification ......................................................................................................... 5 1.4 Study Questions............................................................................................................. 7 1.5 Objectives ...................................................................................................................... 8 1.6 Hypotheses .................................................................................................................... 9 1.7 Theoretical Framework: precede-proceed model ........................................................ 10 CHAPTER TWO....................................................................................................................... 14 2.0 LITERATURE REVIEW ............................................................................................. 14 2.1 Global concern on water and sanitation impacts on health ......................................... 14 2.2 Disease burden due to environmental hygiene and sanitation ..................................... 17 vi 2.3 Notable environmental hygiene and sanitation interventions...................................... 20 2.4 Effectiveness of WASH interventions in Reducing Diarrhoea Morbidity .................. 29 2.5 Role of advocacy as a software approach in hygiene and sanitation promotion ......... 33 CHAPTER THREE .................................................................................................................. 35 3.0 METHODS AND MATERIALS .................................................................................. 35 3.1 Study Area ................................................................................................................... 35 3.2 Study population ......................................................................................................... 35 3.3 Inclusion/Exclusion criteria ......................................................................................... 35 3.4 Ethical Issues ............................................................................................................... 35 3.5 Study design ................................................................................................................ 36 3.6 Sample size determination........................................................................................... 37 3.7 Population Sampling Procedure .................................................................................. 38 3.8 Data collection methods .............................................................................................. 39 3.9 Data Management and analysis ................................................................................... 45 3.10 Study Limitations ........................................................................................................ 46 CHAPTER FOUR ..................................................................................................................... 47 4.0 RESULTS ....................................................................................................................... 47 4.1 General overview ........................................................................................................ 47 4.2 Key Demographic Variables ....................................................................................... 47 4.3 Knowledge and Practices of Sanitation and Hygiene Before and After Intervention . 54 4.4 Change in Health Outcome as Measured by Surrogate Parameters ............................ 61 4.5 Linkages between mother’s behaviour and targeted health improvement indicators.. 68 CHAPTER FIVE ....................................................................................................................... 77 5.0 DISCUSSION, CONCLUSION AND RECOMMENDATIONS .............................. 77 vii 5.1 Discussion ................................................................................................................... 77 5.2 Conclusions ................................................................................................................. 87 5.3 Recommendations ....................................................................................................... 89 REFERENCES .......................................................................................................................... 91 APPENDICES ......................................................................................................................... 102 viii LIST OF TABLES Table 1: Reason for not having toilet facility (2007 and 2008) .............................................. 54 Table 2: Cross-tabulation of whether latrine is important in 2007 and in 2008 ..................... 55 Table 3: Knowledge on diseases associated with drinking unsafe water ............................... 56 Table 4: Change in hand washing prevalence (2007 and 2008) ............................................. 57 Table 5: Change in hand washing in 2007 and 2008, grouped by age group ......................... 58 Table 6: Presence of soap in the house in 2007 and 2008, grouped by education level ........ 58 Table 7: Drinking water storage in 2007 and 2008, grouped by Division ............................ 59 Table 8: Way of disposing off children faeces ...................................................................... 60 Table 9: Chlorine Level in 2007 and in 2008 ........................................................................ 62 Table 10: Paired Samples Statistics on faecal coliforms per 100 ml sample ......................... 63 Table 11: Cross-tabulation on child diarrhoea at baseline and endline .................................. 65 Table 12: Ova and Cyst and Bacterial and parasitic pathogens in stool ................................. 68 Table 13: Association between FC change and modifiable risk factors............................... 70 Table 14: Association of microbes in children stool and mother’s behaviour ....................... 73 Table 15: Classification between microbes in children stool and mothers behaviour............ 74 Table 16: Modifiable behaviour and diarrhoea in children aged less than 5 Years ............... 75 Table 17: Association between sanitation and hygiene promotion in children ...................... 76 ix LIST OF FIGURES Figure 1: Theoretical framework based on PRECEDE-PROCEDE model ........................ 13 Figure 2: Effectiveness of WASH Interventions to reduce diarrhoea ............................... 32 Figure 3: Distribution of Respondents by Division............................................................ 48 Figure 4: Age distribution of study respondents ................................................................ 49 Figure 5: Respondent’s Age Distribution by Division ....................................................... 50 Figure 6: Highest Education Level of the Respondent....................................................... 51 Figure 7: Distribution of Respondent’s Level of Education by Division ........................... 52 Figure 8: Distribution of Latrine Type by Division ........................................................... 53 Figure 9: Distribution of knowledge on latrine importance (2007 and 2008) .................... 55 Figure 10: Contamination of compound with faecal matter ................................................. 61 Figure 11: Diarrhoea in children in the last one month prior and after the intervention ...... 64 Figure 12: Microbes in Stool specimens from Children Aged Less Than 5 Yrs ................ 66 Figure 13: Diarrhoea related microbes in children at baseline and endline ......................... 67 Figure 14: Change in faecal coliform count between 2007 and 2008 ................................... 69 Figure 15: Normal probability plots of residuals .................................................................. 71 Figure 16: Histogram on dispersion of residuals................................................................... 72 x LIST OF APPENDICES Appendix 1: HOUSEHOLD QUESTIONNAIRE................................................102 Appendix 2: WATER SAMPLING AND REPORT FORM................................118 Appendix 3: MAP OF STUDY AREA.................................................................122 Appendix 4: ETHICS AND RESEARCH CLEARANCE....................................123 Appendix 5: PUBLISHED PAPERS....................................................................126 xi LIST OF ABBREVIATIONS AND ACRONYMS ADB African Development Bank APD Administration, Planning and development ASAL Arid and Semi-Arid Lands BC Before Christ CBOs Community Based Organisations CBS Central Bureau of Statistics Cspro Census for population processing DALYS Disability Adjusted Life Years DFID Department For International Development DHS Demographic and Health Survey DPD Diethyl-p-phenylenediamine EA Enumeration Area GOK Government of Kenya IRC International water and Sanitation research Centre JKUAT Jomo Kenyatta University of Agriculture and Technology JMP Joint Monitoring Programme KEMRI Kenya Medical Research Institute. KNBS Kenya National Bureau of Statistics MDG Millennium Development Goals NGOs None Governmental Organisations xii OECD Organization for Economic Co-operation and Development PHAST Participatory Hygiene and Sanitation Transformation PPS Probability Proportion to Size PSU Primary Sampling Unit SPSS Statistical Package for SS Social Scientist TNTC Too numerous to count TOT Training of trainers UK United Kingdom UNESCO United Nations Educational, Scientific and Cultural Organisation UN-HABITAT United Nations Human Settlement programme UNICEF United Nation Children Fund WASH Water Sanitation and Hygiene WEDC Water Engineering Development Centre WHO World Health Organisation WSP Water and sanitation Program WSSC Water Supply and Sanitation Collaborative centre XLD Xylose Lysine Dextrose xiii OPERATIONAL DEFINITIONS Basic Sanitation - Refers to the management of human faeces at the household level. This terminology is used as an indicator for measuring targets of the Millennium Development Goal on sanitation. Household - The basic residential unit in which economic production, consumption, inheritance, child rearing, and shelter are organized and carried out. This may be synonymous with family. Hygiene -The practice of keeping oneself and surrounding environment clean. Open defecation –Indiscriminate disposal of human waste that allows access by flies and provides conducive environment for transmission of pathogens to human. Sanitation -Generally refers to the provision of facilities and services for the safe disposal of human urine and faeces. Shared facility –Any hygiene and/or sanitation utility used by more than one household xiv ABSTRACT It has been established that lack of access to safe drinking water together with inadequate sanitation and hygiene is globally an overwhelming contributor to approximately 4 billion cases of illness annually. In developing countries, diarrhoea accounts for nearly 1.6 million deaths of children aged less than five years, which is approximately 15% in all deaths for this population age group. Poor sanitation and hygiene are among the main factors associated with diarrhoea, worm infestation, eye and skin infections. This study was set out to test the extent to which sanitation and hygiene promotion influenced mothers and children’s health in Turkana District of Kenya. A longitudinal/cohort design incorporating clustered, stratified and random sampling methods was employed to select a sample of 300 mothers and their children aged less than five years at baseline (2007). Interventions undertaken included capacity building and empowerment approach to trigger communities to demand hygiene and sanitation facilities. A post-intervention survey with the same baseline participants was carried out in 2008. Interviews, laboratory analysis and spot observations/inspection were used to collect study data on demographics, socio-economic status, waste disposal parameters and testing faecal coliform count in drinking water as well as diarrhoea related microbes in children stool. Data were entered into the computer and analyzed using SPSS for frequencies, descriptive and multivariate analysis. xv After intervention, the results showed there was significant change in sanitation and hygiene parameters. Household ownership of traditional pit latrine increased from 45.5% in 2007 to 63.6% in 2008 (χ²=4.43, P=0.035). For hand washing practice, those who washed hands regularly hand in Turkana District increased from 73.5% to 91.3% (χ²=9.34, P=0.053). Similarly, improvements in hand washing practice were observed to increase by age group with those aged 36 and 45 years increasing significantly from 66.7% in 2007 to 88.9% in 2008 (χ²=10.01, P=0.04). In addition, presence of soap in households increased significantly from 65.4% to 77.9% (χ²=3.87, P=0.049) within the population with no formal education. he mean faecal coliforms in drinking water reduced from 88 faecal coliform units in 2007 to 30.2 faecal coliform units in 2008 (P=0.005) in Kakuma Division, 91 to 17.3 faecal coliforms units (P=0.003) in Lodwar Central, and from 63.8 to 23.6 units (P=0.006) in Lokichogio Division. Overall, community health outcomes before and after the intervention were significantly improved, with comparative reduction in faecal coliform count in drinking water ranging from 40.2% to 73.7% (P=0.003 to P=0.006) across the three Divisions within Turkana District. Similarly, diarrhoea related microbes in children’s stool reduced by 13% (P=0.003) while diarrhoea prevalence in children aged less than five years reduced from 43.7% in 2007 to 30.7% in 2008 (P=001). Promotion of hygiene and good sanitation practices in the study area improved mother’s hygiene behaviour and child’s health with an associative strength of about 40% (Rsquare of 39.6%, P=0.048). These associated gains were strongly related to age of the xvi mother (P=0.015), presence of latrine (P=0.038), and reasons given at baseline for not having latrine (P=0.005). On the other hand, multivariate analysis showed that diarrhoea related microbes presence or absence could be predicted with an overall precision of 92.7% with core determinants/predictors being mothers education level (P=0.033), toilet presence (P=0.022), distance to latrine (P=0.004), source of drinking water (P=0.019), treatment of drinking water at point of use (P=0.013), and storage methods of drinking water (P=0.067). In addition, the main risk factors associated with diarrhea in children aged less than five years after intervention (2008) were strongly linked to behavioural characteristics; namely if the child had diarrhoea at baseline (P=0.029), mother’s education (P=0.011), latrine availability (P=0.029, latrine structure (P=0.002) and chlorine level in the drinking water after the intervention (P=0.054). In conclusion therefore, it is evident that promotion of improved sanitation and hygiene using community participatory approaches such as Participatory Hygiene and Sanitation Transformation (PHAST) in the context of community led total sanitation (CLTS) led to significant reduction of diarrhoea prevalence in children aged less than five years and its application should therefore be up-scaled in disadvantaged communities. xvii CHAPTER ONE 1.0 INTRODUCTION 1.1 Background Turkana District has three international borders; Ethiopia to the East, South Sudan to the North, and Uganda to the West. Nationally, it borders Samburu, Baringo and West Pokot Districts. It is the largest District in Kenya, covering an area of 77,000 square kilometres; and constitutes about 42% of the Rift Valley Province. It is dry and semi arid, with less than one-third of the land mass being arable. Its population is about 860,000 people (KNBS, 2009). The topographical features include mountain ranges to the west, open plains in the middle, and several seasonal rivers and Lake Turkana to the east. Lake Turkana is the largest and most saline of the Rift Valley lakes. Turkana District is classified as arid and semi-land (ASAL) and experiences prolonged spells of inadequate water supply and limited access. As result, people walk long distances to collect water from rivers and streams. In areas where water exists, it is likely to be contaminated due to common use by both humans and animals. The scarcity and low quality of water influences the level of health status in many households owing to poor sanitation and hygiene practices, especially those related to excreta disposal and hand washing. 1 Children especially under the age of 5 years mostly in developing countries suffer mostly from diarrhoea, where every episode reduces calorie and nutrient uptake, reducing growth and development for those affected. Lack of access to safe drinking water and inadequate sanitation and hygiene practices are overwhelmingly associated with 1.8 million deaths globally and cause approximately 4 billion cases of illness annually (World Health Organization, 2007). 1.2 Problem Statement Diarrhoeal diseases continue to be responsible for childhood mortality and morbidity, primarily in developing Countries, although in the last several decades a significant reduction on deaths from diarrhoeal diseases has been observed (Ahmed et al., 1994). Despite advances in case management of diarrhoeal diseases, the diseases are a major cause of morbidity and mortality among young children in developing countries (Bern et al., 1992., Murray et al., 1994). In developing countries, diarrhoea accounts for the deaths of nearly 1.6 million children aged less than five years annually or almost 15% of all deaths in this segment of the population (World Health Organization, 2003). Sanitation and human health are closely connected as lack of appropriate hygiene policies and disposal of human excreta can lead to transmission and spread of diseases that cause diarrhoea. Contaminated water and indiscriminate disposal of faecal matter account for 5.7% of diarrhoea amongst children. Poor sanitation and hygiene has been associated with diarrhoea, worm infestation, and eye and skin infections. Out of all the sanitation and hygiene related 2 diseases, diarrhoea disease is the most deadly especially for children (Pruss, et al., 2008). The burden of illness for children under five years of age that arises from diarrhoeal diseases linked to inadequate water, sanitation and hygiene is up to 240 times higher in Africa than in high income Nations (Pruss et al., 2002). It is estimated that 94% of these diarrhoeal cases are preventable through modification of the environment, including interventions to increase the availability of clean water and improvement in sanitation and hygiene (Ustun and Corvalan, 2006). Improvement in environmental sanitation has significant positive impact on environmentally related diseases such as malaria, diarrhoea, skin and eye infections and the overall dignity and well-being of the populations (Harvey and Reed, 2004). Improved access to safe water supply is attributable to reduction of diarrhoea incidences by about one fifth and the number of deaths due to diarrhoea by more than half (Black and Fawcett,2008a). In many developing countries, inadequate sanitation is associated with several public health problems and several infectious, faecal-oral -related diseases such as cholera and diarrhoea. Over 2.2 million people die each year with more than 70% being children under five years of age from diarrhoea related diseases (Black and Fawcett, 2008b). In Turkana District, several outbreaks of cholera and diarrhoea diseases have previously been reported according to Ministry of Health weekly disease outbreak reports, in May 3 2006 there was cholera outbreak in Kakuma Division of Turkana District, with 53 cases and 2 deaths (GOK, 2006). According to (GOK, 2005) there was cholera outbreak in Turkana District with a total of 370 cases and 7 deaths. During this period, infant mortality rate in Turkana District was 170 per 1000 live births and child mortality rate was 220 per 1000 live births. These rates are twice higher than the national average 78/1000 and 114/1000 respectively (KDHS, 2001). The purpose of this study therefore is to evaluate hygiene and sanitation interventions in Turkana in reference to their impacts on mother’s behaviour and children health. 4 1.3 Study Justification Access to safe water and sanitation stimulates changes in hygiene behaviour, hence a key reason for investing in hygiene and sanitation services. Starting at household level, people are most likely at risk of contamination especially where they spend most of their time. Health benefits are accrued to families who have latrines even where neighbours do not; additional benefits then accrue as coverage extends to the whole neighbourhood (IRC and WEDC, 2002). Improved sanitation and hygiene are critical for improvement of child health through reduction of diarrhoea, worm infestation, eye and skin infections. According to WHO reports, more than three million children die from diarrhoea each year, and over 500 million children are infected with common worms, approximately six million people become blind due to trachoma as a result of poor access to safe water, sanitation and hygiene (Shordt and Caincross, 2004). Several studies have shown that improved sanitation and hygiene promotion significantly reduce sanitation and hygiene related diseases. Unfortunately, very few studies have been conducted to assess the effectiveness of the sanitation and hygiene interventions in reduction of these diseases among under privileged communities in Kenya such as those of Turkana District. In recent past, several projects on improvement of hygiene and sanitation have been initiated in Turkana District by the Government, NGOs, CBOs and other organizations. However, it has been difficult to evaluate and demonstrate the effectiveness of these 5 interventions because of lack of baseline information. Majority of these projects in Turkana District do not target sanitation and hygiene practices and the prevalence of related diseases among children aged under five years but largely focus on the processes and the direct outputs of the projects with little regard to actual impact on the burden of the diarrhoea diseases. As a result, this has contributed greatly to the poor health indicators in the District and especially among the under fives hence the need for this study which covers both baseline and end-line data. The results of this study will be useful to the District health managers and other public health practitioners in the area of sanitation and hygiene, particularly in formulating appropriate policies and strategies to address the problem of poor sanitation and hygiene. 6 1.4 Study Questions 1.4.1 Was there any change in knowledge on sanitation and hygiene among mothers after the interventions? 1.4.2 Did the interventions have any effect on mothers sanitation and hygiene behaviour and practices? 1.4.3 What was the effect of the interventions on the prevalence of microbials in drinking water at the point of use after? 1.4.4 What was the effect of the interventions on the diarrhoea prevalence among children aged less than five years? 1.4.5 What was the effectiveness of hygiene and sanitation interventions in changing mother’s hygiene behaviour and improving child health in Turkana District? 7 1.5 Objectives 1.5.1 Broad Objective The aim of the study was to determine the effectiveness of sanitation and hygiene interventions in changing mothers’ behaviour and practices and improving child health in Turkana District. 1.5.2 Specific objectives 1.5.2.1 To assess change in sanitation and hygiene knowledge of mothers after the interventions. 1.5.2.2 To determine the changes in sanitation and hygiene behaviour and practices of mothers after the hygiene and sanitation interventions. 1.5.2.3 To determine the change in prevalence of microorganisms in drinking water at the point of use after hygiene and sanitation interventions. 1.5.2.4 To determine the change in diarrhoea prevalence among children aged less than five years after hygiene and sanitation interventions. 1.5.2.5 To determine the effectiveness of hygiene and sanitation interventions in changing mother’s hygiene behaviour and improving child health in Turkana District. 8 1.6 Hypotheses Null hypotheses: 1.6.1 Sanitation and hygiene interventions have no effect in changing mother’s knowledge in sanitation and hygiene before and after the intervention. 1.6.2 Sanitation and hygiene promotion has no effect in changing mother’s behaviour and practices after the interventions. 1.6.3 Sanitation and hygiene interventions have no effect in changing faecal coliform count in drinking water at the point of use before and after the intervention. 1.6.4 Sanitation and hygiene interventions have no effect in changing diarrhoea prevalence among children aged less than five years before and after the intervention. 1.6.5 Sanitation and hygiene promotion has no effect on changing mother’s hygiene behaviour and improving child health in Turkana District. 9 1.7 Theoretical Framework: precede-proceed model The study applied excerpts of the Precede-Proceed model which is a framework that has been used widely by health program planners, policy makers, and evaluators to analyze the situation and design a health program efficiently. This model is multidimensional, founded in the social/behavioural sciences, epidemiology, administration and education constructs. As such, the model recognizes that health outcomes and health behaviours have multiple causations which must be evaluated in order to assure appropriate intervention. This planning model was initiated as a cost-benefit evaluation framework (Green, L.W. 1974). It provides a comprehensive structure for assessing health and quality of life needs and for designing, implementing, and evaluating health promotion and other public health programs to meet those needs. The most fundamental assumption of the model is the active participation of its intended audience – that is, the participants will take an active part in defining their own problems, establishing their goals, and developing their solutions. In the case of this study participants engagement was ensured therefore this fundamental assumption was met. The PRECEDE model is a framework for the process of systematic development and evaluation of health education programs. An underlying premise of this model is that health education is dependent on voluntary cooperation and participation of the client in a process which allows personal determination of behavioural practices; and that the degree of change in knowledge and health practice is directly related to the degree of active participation of the client. Therefore, in this model, appropriate health education is 10 considered to be the intervention for a properly diagnosed problem in a target population (Green, 1992).The model can be applied in a variety of settings such as school health education, patient education, community health education, and direct patient care settings. PROCEED was added to the framework later in recognition of the emergence of and need for health promotion interventions that go beyond traditional educational approaches to changing unhealthy behaviours. The administrative diagnosis is the final planning steps to "precede" implementation. From there "proceed" to promote the plan or policy, regulate the environment, and organize the resources and services, as required by the plan or policy. The components of PROCEED take the practitioner beyond educational interventions to the political, managerial, and economic actions necessary to make social systems environments more conducive to healthful lifestyles and a more complete state of physical, mental and social well-being for all. The purpose of the PRECEDE/PROCEED model is to direct initial attention to outcomes rather than inputs. This forces planners to begin the planning from the outcome point of view. In other words, you as a program planner begin with the desired outcome and work backwards to determine what causes it, what precedes the outcome. Intervention is targeted at the preceding factors that result in the outcome. Although the study did not apply all the phases its noteworthy to understand that the PRECEED/PROCEED model has a total of nine phases, namely: social assessment, 11 epidemiological assessment, behavioural and environmental assessment, educational and ecological assessment, administrative and policy assessment, implementation, process evaluation, impact evaluation and finally outcome evaluation. Phase one to five fall under PRECEDE while phase six to nine fall under PROCEED. PRECEDE stage of this model mainly focuses on the situational assessment surrounding a health issue while Proceed focuses on implementation and subsequent evaluation. Phase one and two deal with social and epidemiological assessment. Social assessment deals with identifying the aspects in the community that impact on living healthy and productive lives, from the community’s own perspective or felt needs. Epidemiological assessment involves using epidemiological data to prioritise the health problems identified in the social assessment phase. This study focused on adopted phase three (behavioural and environmental assessment) and four (Educational and Ecological assessment) of the Precede-Proceed model. Phase three involves identifying behavioural and environmental correlates of a health issue. A correlate is here defined as a factor associated with the existence of a particular health problem. This focussed on the existence of behaviours, which have a direct relation with spread of diarrhoeal diseases like poor hygiene practices among others. This phase also focussed on the social environmental issues such as poverty, socio-economic disparities among sociocultural and familial control on behaviour. 12 Phase four focuses on the factors influencing the correlates identified in phase three above. These factors are divided into Predisposing, Reinforcing and Enabling. These factors must be changed in order to initiate and sustain the process of behaviour change. Predisposing factors are the affective and cognitive components of behaviour. These factors can help or hinder a person’s motivation to change. In this study, the researcher conceptualised predisposing factors focused on; knowledge, perception, hygiene and sanitation. Under reinforcing factors, the study focused on community values such as cleanliness which leads to healthier environments. Enabling factors were identifies as access to sanitation services and water. All these factors were conceptualized based on the access to sanitation services/facilities. The Figure 1 depicts the researcher’s concept. Predisposing factors Knowledge Beliefs Practices Behaviour and lifestyle Unsafe excreta disposal practices Negative cultural practices Risk factors for diarrhoea diseases Reinforcing factors Community values Hygiene education Enabling factors Access to sanitation services Access to water Social environment Poverty Education levels Socio-economic differences Figure 1: Theoretical framework based on PRECEDE-PROCEDE model 13 CHAPTER TWO 2.0 LITERATURE REVIEW 2.1 Global concern on water and sanitation impacts on health Water supplies and sanitation were first highlighted on the development agenda about 30 years ago. This was a result of the 1977 United Nations Conference in Mar del Plata, Argentina that recommended proclaiming the 1980s to be the International Drinking Water Supply and Sanitation Decade with the goal of providing every person with access to water of safe quality and adequate quantity, along with basic sanitary facilities, by 1990” (World Water Development Programme, 2003). International water policies and management practices have generally considered water to be a free and renewable resource. Governments in developing countries have often subsidized water supplies, typically in an attempt to achieve social and health benefits for low-income households that comprise a large majority of the rural population (Lammerink, 1998., Whittington, 1998). Furthermore, developing countries have made huge investments in their rural water supplies under the presumption that local communities will be involved in their maintenance and operation. In sub-Saharan Africa, reducing the number of people without access to safe drinking water and basic sanitation has proved to be a significant challenge. The region is lagging behind the rest of the world with respect to achieving the Millennium Development Goal on water supply and sanitation which aims at reducing the proportion of people without access to safe drinking water and 14 basic sanitation by half before 2015. Kenya appears to be on track towards achieving the water MDG while the sanitation aspect is lagging behind (WSP, 2006). Sanitation on the other hand, generally refers to the provision of facilities and services for the safe disposal of human urine and faeces. Inadequate sanitation is a major cause of infectious diseases globally and improving sanitation is known to have a significant beneficial impact on health both at household level and across communities (www.who.int/sanitation/en, 2007). The UNESCO World report for water, (2003) outlines the health effects emanating from poor water and sanitation as follows: Almost half the people in the developing world have one or more of the main diseases or infections associated with inadequate water supply and sanitation: diarrhoea, intestinal helminth infections, dracunculiasis, schistosomiasis, and trachoma. More than half the hospital beds in the world are occupied by people who have these diseases. Eighty eight percent of diarrhoeal diseases, the second leading cause of death in children younger than five years after respiratory illnesses are attributed to unsafe drinking water, inadequate sanitation, and poor hygiene. Diarrhoea morbidity is reduced by around 21% through improved water supply and by around 37% through improved sanitation. Though not well documented, the trauma of watching a child die from a preventable disease such as diarrhoea as does happen in one out of five in the 15 poorest parts of the world can have lasting impacts on the psychological and emotional health of surviving parents and siblings. Six million people worldwide are blind because of trachoma, the leading cause of preventable blindness and more than 150 million people need treatment. Improving access to water and better hygiene can reduce trachoma morbidity by 27%. Intestinal helminths (Ascaris, Trichuris, hookworm) affect hundreds of millions of people; 133 million have high intensity intestinal helminth infections, which often have severe consequences such as cognitive impairment, massive dysentery, or anaemia. Safe drinking water and basic sanitation combined with better hygiene can reduce morbidity from ascariasis, for example, by 29%. Overall, healthy people, as opposed to those sickened by helminthiases, are better able to derive nutritional benefit from food. More than 160 million people are infected with schistosomes, causing tens of thousands of deaths every year, mainly in sub-Saharan Africa. Basic sanitation can reduce schistosomiasis by up to 77%. 16 2.2 Disease burden due to environmental hygiene and sanitation In 400 BC, Hippocrates noted the ecological basis for disease in Airs, Waters, and Places. In assessing the state of health across the globe, Smith et al. (1999) contend that “many of the critical health problems in the world today cannot be solved without major improvement in environmental quality.” A recent update of this analysis “confirms that approximately one-quarter of the global disease burden, and more than one-third of the burden among children, is due to modifiable environmental factors (Ustun & Corvalan 2006). Diarrhoea continues to be one of the leading causes of death and loss of disability adjusted life years in the developing world (Lopez et al., 2001) Estimates from the past four decades indicate that, although there has been a decrease in mortality rates, diarrhoeal disease-related morbidity has remained high (Kosek et al., 2003) Interventions to reduce diarrhoea incidence generally focus on water supply, water quality, sanitation and hygiene for all age groups, as well as breastfeeding, adequate nutrition and immunizations specifically for children less than5 years of age. Although there has been some attempt to utilize large-scale and widely available cross-sectional studies such as the Demographic and Health Surveys (Gunther & Fink, 2010) in many studies, most guidelines and policies relevant to diarrhoea in developing countries, such as those developed by the WHO with reference to household storage or disinfection of water, micronutrient supplementation or use of oral rehydration solution, have been 17 informed by longitudinal intervention trials that are conducted with smaller cohorts followed over time. According to Black and Fawcett (2008c), more than 1.2 billion people worldwide gained access to improved sanitation between 1990 and 2004. However, even with this progress, some 41 percent of the world’s population- an estimated 2.6 billion people, including 980 million children lack access to proper sanitation. Lack of adequate sanitation, poor hygiene and safe portable water are serious global health problems and contribute to deaths of 1.5 million children under the age of five years annually due to diarrhoeal diseases. Although infant and child mortality rates have reduced significantly in most nations in the recent decades, 1.5 to 2 million children still die every year from water and sanitation related diseases (Murray et al., 2001). According to WHO (2008), an estimated 2.2 million children aged less than 5 years die from diarrheal diseases each year. More children are debilitated by illness, pain and discomfort primarily from diarrhoeal diseases, intestinal worms, from various eye and skin diseases and diseases related to insufficient and unsafe water (UNICEF, 2007). According to WHO (2007), 4 billion cases of diarrhoea occur annually, of which 88% are attribute to unsafe water and inadequate sanitation and hygiene. Diarrhoeal diseases also account for 1.8 million deaths every year with, the vast majority being children under five years. World Health Organisation data on the burden of disease shows that, “approximately 3.1% of deaths 18 (1.7million) and 3.7% of disability adjusted life- years (DALYs) or equivalent to 54.2 million sufferings worldwide is attributed to unsafe water and sanitation and hygiene”. In Africa and other developing Countries in South East Asia, 4-8% of all disease burdens are attributable to these factors. Over 99.8% of all the deaths occur in developing countries and 90% are deaths of children (WSSCC and WHO, 2005). Helminthic infections are also important causes of morbidity and mortality in many developing Countries. An estimated 1.5 billion cases of infection with Ascaris lumbricoides, 1,200 million cases of infection with hookworm, 1,049 million cases of infection with Trichuris trichiura, and 200–300 million cases of Schistosomiasis occur worldwide. School age children in developing countries bear the greatest health burden due to helminthic infections, accounting for an estimated 20% of the disability-adjusted life years lost due to infectious diseases in children less than 14 years old (Ezeamama et al., 2005). According to Black and Lanata, (1995a), diarrhoeal diseases, which are frequently transmitted by faecally-contaminated water, continue to be a leading cause of morbidity and mortality among children in developing countries. Improved water supply reduces diarrhoea morbidity by 21%. While improved sanitation reduces diarrhoea morbidity by 37.5% (WHO, 2004). Diarrhoea has been associated with up to 75% of all illnesses in young children. The risk factors include lower socio-economic status, an unclean domestic environment, use of unsafe water, absence of soap (Sharon 19 et al., 1987). Most of the burden of diarrheal disease is thought to be preventable with improvement in sanitation, water quality, and hygiene. However, in rural areas of low income countries it is often prohibitively expensive to provide residents with networked sanitation and water treatment that provide microbiologically and chemically safe water and consistently remove faeces from the environment (Ezzati et al., 2003). In Kenya, World Health Organization estimated that in 2002, 52% of Kenyans did not have access to improved sanitation and in rural areas, 57% of the people lacked sanitation coverage (WHO, 2004). About 11% of all Kenyans used flush toilets. The most common form of sanitation facility was a pit latrine, which was used by nearly 64% of the population, while more than 16% had no facility and defecated in the brush, field or in the open. Apart from those that do not use a latrine, 49% shared their toilet with other households (CBS, 2004). 2.3 Notable environmental hygiene and sanitation interventions There is a striking impact on the reduction of incidence of all cases of diarrhoea, including dysentery and persistent diarrhoea in children less than 5 years arising from water, sanitation and hygiene education interventions. According to a study published by Aziz et al (1990), about 25% of children in the intervention area were experiencing fewer episodes of diarrhoea than those in the control area. Such interventions include general hygiene practices, hand washing, improved access to safe water supply with advocacy being the vehicle of choice. 20 A cost-benefit analysis by Organization for Economic Co-operation and Development Roundtable on Sustainable Development showed that achieving the global MDG target in water and sanitation would bring substantial economic gains from both health and other benefits: each US$1 invested would yield an economic return of between $3 and $34, depending on region. The benefits would include an average global reduction of diarrhoeal episodes of around 10%. If the goal for water and sanitation were met, the health-related costs avoided would reach $7·3 billion per year, and the annual global value of adult working days gained as a result of less illness would be almost $750 million. Improvement in sanitation, hygiene, and water contributes to improved health, generates savings for households and national health budgets, and contributes to poor households' economies through reduced costs and losses of time. Saving time may enable productive activity and school attendance, especially for girls. Investment in water and sanitation whether through development assistance at the national or community levels or by poor households themselves—makes sound economic sense (OECD and ADB, 2004) 21 2.3.1 General Hygiene Practices Improved personal and environmental hygiene reduce infections and reduces the spread of infections (Aiello and Larson, 2002). Thus appropriate hygiene practices are necessary for maintaining good health. The function of hygienic behaviour is to prevent the transmission of the agents of infection. Impact of several environmental sanitation conditions and hygiene practices on occurrence of diarrhoea among children under five years was associated with washing and purifying fruit and vegetables; domestic water reservoir conditions; faeces disposal, presence of vectors in the house and flooding in the lot (Heller et al., 2003). Sanitation and hygiene, given their direct impact on infectious disease, especially diarrhoea, are important for prevention of malnutrition. According to WHO/UNICEF (2010), improved sanitation include use of flush toilet, ventilated pit latrine, pit latrine with slab and compositing toilet whereas unimproved pit latrine are shared toilet facilities, no facilities, pit latrine without a slab and bucket. In their assessment they found out that access to toilet/latrine facility was by 48.3% of the households. Of the 51.7% who did not access a toilet facility, they used the bush, open land, laga or near a river. These results are not significantly different from the 2010 findings in a study done in Marsabit where 44.6% of the households had access to toilet facilities. Of the caregivers, less than half, 42.6% disposed of the child’s stool immediately and hygienically while 38.7% disposed the child’s stool in the bush and 18.7% did not 22 dispose the child’s stool. The unhygienic practices of stool disposal predispose children to diseases such as diarrhoea. Approximately 80 percent of the hospital attendance in Kenya is due to preventable diseases. About 50 percent of these illnesses are water, sanitation, and hygiene related. In 1999 alone, more than 2,500 Kenyans died from diarrhoea and related diseases. Diarrhoea and gastroenteritis were the highest causes of infant hospitalization in 1999. These diseases are a result of poor hygiene and unsanitary living conditions, which could be prevented by instituting appropriate sanitation and hygiene practices (GOK, 2007). 2.3.2 Hand washing Hygiene related practices such as the safe disposal of faecal material and hand washing after contact with faecal material could reduce the rates of intestinal infection considerably (Astier et al., 1997). Hand washing efficacy studies carried out in the form of randomized controlled trials and the outcome interests have shown health related benefits (Luby et al., 2005). Different field friendly methods of evaluations can also now be used. Data on hand washing can be inferred, observed or reported. Observed data is considered the most objective data available for measuring hand washing behaviour. Observations may be conducted using spot checks or continuous observation. Reduced 23 hand contamination has been demonstrated among persons exposed to hand washing promotion or persons specifically instructed to wash hands with a cleansing agent, compared to persons who were not exposed (Hoque et al., 1995). Presumably the level of hand contamination at critical times, such as preparing food or feeding a young child impacts the degree to which pathogens are transmitted at those times. In terms of measuring contamination that is relevant to pathogen transmission, it would necessitate collection of samples at those critical times, after defecation, before eating and food handling. In addition, testing for the presence of and quantification of faecal coliforms including the Escherichia coli on the subject stool using microbiologic test may be considered an inferred data on the overall hygienic practice including, hand washing behaviour (Kaltenthaler and Pinfold, 1995). Hand washing with soap and water can reduce diarrhoeal diseases by 35% or more. Safe disposal of faecal material serves as primarily intervention to prevent faeces from contaminating the environment. It is particularly important to isolate the faeces of people with diarrhoea, most of whom are usually young children. Pit latrines, when used by adults and for the disposal of young children’s faeces can reduce diarrhoea by 36% or more (Astier et al., 1997). A study done in Bangladesh confirmed the importance of hand washing and compound cleanliness in reducing diarrhoeal diseases among mothers with small children. In this study, soap was supplied to sixty five mothers who were encouraged to wash their hands after, defecation before eating and 24 food handling. They were also encouraged to clean children excreta around their homes promptly and then dispose it into pit latrines or bury it properly and then wash their hands with soap and water. A marked decline of diarrhoea was observed (Gracey, 1993). The most effective way of preventing diarrhoeal diseases is to prevent faecal material from getting into the child’s environment by safe disposal of faeces and washing hands with soap once faecal material has contaminated them. Hand-washing interrupts the transmission of disease agents and so can significantly reduce diarrhoea and respiratory infections, as well as skin infections and trachoma. A recent review (Curtis and Cairncross, 2003) suggests that hand-washing with soap, particularly after contact with faeces (post-defecation and after handling a child’s stool), can reduce diarrhoeal incidence by 42-47 percent, while a publication by Rabie and Curtis (2006) suggests a 30 percent reduction in respiratory infections is possible through hand-washing. This remains true even in areas with high faecal contamination and poor sanitation. They further demonstrated effectiveness of hand washing in reducing respiratory infection risk by 16%. A recent study shows that hand washing with soap by birth attendants and mothers significantly increased newborn survival rates by up to 44 per cent (Rhee et al., 2008) 25 Another recent study found that children under 15 years living in households that received hand-washing promotion and soap had half the diarrhoeal rates as children living in control neighborhoods (Luby et al., 2004). Because hand washing can prevent the transmission of a variety of pathogens, it is said to be more effective than the use of any single vaccine in disease prevention. Promoted on a wide-enough scale, hand washing with soap could be thought of as a ‘do-it-yourself’ vaccine. A study by Bowen et al, (2007), suggests that hand washing promotion in schools can play a role in reducing absenteeism among primary school children. In China, for example, promotion and distribution of soap in primary schools resulted in 54 per cent fewer days of absence among students compared to schools without such an intervention. Habits are ingrained and sustained behaviours, often developed in childhood. Research has shown that once people anywhere acquire ingrained and habitual behaviours, they are not easily lost. The task for hand-washing promotion is not to achieve a single handwashing event, but to instil a routine and sustained habit that happens automatically with every contaminating event. While habits are often learned at an early age, there are opportunities for change, especially at life-changing events. Many mothers report that hand hygiene did not become important to them until a baby was born and that if midwives or others involved with peri-natal care recommended hand washing with soap, it would likely take hold. 26 Another life-changing event for many mothers is moving to the husband’s home after marriage and learning the habits of the new household. Drivers are innate and learned modules in the brain that motivate particular behaviours. They come in the form of emotions and the feelings that people report when carrying out particular behaviours. Discovering drivers is the key to successful promotion of hand washing. As with risk practices, determining drivers can be difficult because they may be buried in the subconscious where as much as 95 percent of human thought takes place (Zaltman, 2003. There may be perceptions of shame or embarrassment in reporting them, for example, using soap to heighten sexual attractiveness. Notably, hand washing success is attributable to high level of political commitment, state or Division level action and community mobilization by village level authorities. 2.3.3 Improved access to safe water supply A silent humanitarian crisis kills some 3900 children every day and thwarts progress towards all the Millennium Development Goals (MDGs), especially in Africa and Asia. The root of this unrelenting catastrophe lies in these plain, grim facts: four of every ten people in the world do not have access to even a simple pit latrine; and nearly two in ten have no source of safe drinking water (WHO, 2004) Presence of improved sanitation and hygiene practices, supplemented with satisfactory supply of water is essential for improved life with tangible benefits to health. Access to safe drinking water is essential to health. As a basic human right and a component of 27 effective policy for health protection, investments in the water supply and sanitation can yield a net economic gain (UN-HABITAT, 2003). Knowledge on disease transmission suggests that 100% of infections caused by soiltransmitted helminthes can be prevented by adequate water, sanitation and hygiene (WHO, 2007). Evidence indicates that lack of safe water increases the prevalence of microbial hazards and continues to be a primary concern in both developing and developed Countries. A report by WHO (2006) indicated that the greatest disease causing microbial risk is associated with ingestion of water contaminated with human or animal (including bird) faeces. Faeces are a major source of pathogenic bacteria, viruses, protozoa and helminthes and faecal derived pathogens form principal concern in setting health-based targets for microbial safety. Microbial contamination of drinking water contributes to disease outbreaks and to emergence of diseases in developed and developing Countries. Control of waterborne diseases is an important element of public health policy and objective of water supplies (WleChevallier and Kwock-Keug, 2004). According to WHO analysis, faecal indicator bacteria provide a sensitive measure of pollution of drinking water supplies. Verification of the microbial quality of drinking water includes testing for Escherichia coli as an indicator of faecal pollution. E. coli provides conclusive evidence of recent faecal pollution. In practice, testing for thermo tolerant coliform bacteria can be acceptable alternative in many circumstances (WHO, 2006). 28 In Kenya, Access to safe water was estimated at 89.7% in urban areas and 43.5% in rural areas, or a national average of about 57% (as reported in the 2000 Multiple Indicator Cluster Survey). In addition, about 81% of the population had access to safe sanitary means, with 94.8% in urban areas and 76.6% in the rural areas. The World Bank’s 2004 Water and Sanitation Country Assessment had put the coverage at 49% for water supply (urban 86% and rural 31%) and 86% for sanitation (urban 96% and rural 81%). Among the main synergies between the water and sanitation sector (WSS) sector and other MDGs were reduced incidence of water-borne diseases, empowerment of women and girls through savings on time and energy especially in provision of water, improvement in the living conditions in slum areas, business opportunities in the envisaged private sector participation (especially for women entrepreneurs in water and sanitation service delivery), and higher retention of girls in school due to improved provision of water and sanitation facilities (CBS, 2003) 2.4 Effectiveness of WASH interventions in Reducing Diarrhoea Morbidity Diarrhoeal diseases, which are frequently transmitted by faecally-contaminated water, continue to be a leading cause of morbidity and mortality among children in developing countries (Black and Lanata, 1995b). According to WHO 2004 fact sheets, 1.8 million people die every year from diarrhoeal diseases (including cholera) of which 90% are children under 5, mostly in developing countries. Accordingly, 88% of diarrhoeal disease is attributed to unsafe water supply and inadequate sanitation and hygiene. For 29 a while now, it has been widely accepted that water supplies and sanitation, though necessary for the prevention of diarrhoeal diseases in young children, are not sufficient by themselves unless they are accompanied by changes in domestic hygiene behaviour (Mertens et al., 1992., Cairncross, 1990).In the lancet Series on Maternal and Child Under nutrition Bhutta et al (2008) states that of several disease prevention strategies that reduce the burden of infections (and hence affect nutritional status), hygiene interventions (hand washing, water quality treatment, sanitation and hygiene) are among the core interventions to affect nutritional status. Previous studies have reported the results of interventions to reduce illness through improvements in drinking water, sanitation facilities, and hygiene practices in less developed countries. One of the initial systematic review and meta-analysis (Lorna et al., 2005) comparing the evidence of the relative effectiveness of these interventions reported that all the interventions studied were found to significantly reduce the risks of diarrhoeal illness. The relative risk estimates from the overall meta-analyses ranged between 0·63 and 0·75. The results showed that multiple interventions (consisting of combined water, sanitation and hygiene measures) were not more effective than interventions with a single focus. A meta-analyses by Curtis and Cairncross (2003) examined the impact of hand-washing on diarrhoea risk and found a reduced risk of 50 per cent (Aiello et al., 2008), a reduced risk of gastrointestinal illness of 34 per cent across 12 studies conducted in developing 30 countries and also found a reduced diarrhoea risk of one-third across five randomizedcontrolled trials (RCTs) in developing countries. A recent meta-analysis (Waddington et al., 2009) has combined the results of various analyses and reviews conducted in the recent past and have pooled the respective results. The results confirm the conclusion of earlier reviews that the three most effective interventions to reduce diarrhoea morbidity in children under 5 are hand washing with soap (37%), improved sanitation (34%) and point of use (POU) water treatment (29%). One reason for the relatively low effectiveness of source water treatment interventions (21% in the chart below) is the risk of microbiological contamination of drinking water during collection and storage in the home (Clasen et al., 2006). A systematic meta-analysis of 22 studies measuring bacteria counts for sources of water supplies and stored water in the home concluded that approximately half of the included studies identified significant contamination of water after collection (Wright et al., 2004). According to Luby et al.(2007) and colleagues who studied hand washing behaviour in 347 households from 50 villages across rural Bangladesh. The researchers compared a non-intervention control group with communities that were part of a large hand washing, hygiene/sanitation, and water quality improvement programme — Sanitation, Hygiene Education and Water Supply in Bangladesh (SHEWA-B), organised and supported by the Bangladesh Government, UNICEF, and the UK’s Department for 31 International Development (DFID,1998). The following are the results of their study. The following are the results of their study showing Reduction in diarrhoea morbidity in children aged <5 years as per intervention Source: (Waddington et al., 2009) Figure 2: Effectiveness of WASH Interventions to reduce diarrhoea morbidity in children aged less than 5 yrs They concluded that washing of hands with soap, or simply rinsing hands without soap prior to preparation of food can reduce the occurrence of diarrhoea in children. 32 2.5 Role of advocacy as a software approach in hygiene and sanitation promotion The World Health Organisation and the United Nations Children Fund Joint Monitoring Programme (JMP) for water and sanitation estimate that despite the huge efforts to increase access to sanitation, over 700 million people are forced to defecate in the open (WHO/UNICEF-JMP, 2008). Furthermore, a recent assessment of the existing evidence suggest that poor sanitation may be linked to as much as a quarter of all the under five deaths (Cumming, 2008). Advocacy and promotion on sanitation and hygiene contributes to a significant increase in access to sanitary means of excreta disposal and reduced disease burden, (Bajracharya, 2003). A study in Mpande and Bukalimo villages in Uganda reported an increase in construction of traditional latrines by 80.9% and 87.8% respectively after intervention (Narathius et al., 1994). Multi- level efforts such as media, planning workshops, training sessions and house-tohouse visits by village authorities and health officials raised greater awareness of sanitation and hygiene issues and led to construction of latrines on a self-help basis (Bajracharya, 2003). The study underscores the importance of advocacy, health education and promotion in improvement of hygiene practice (Gilman et al., 1993, Bajracharya 2003). 33 Hygienic behaviour in some cases is determined by beliefs that run counter to biomedical knowledge. In urban Karachi, Pakistan, for instance, infant diarrhoea was frequently considered to be related to teething or weather and thus was considered a normal event (Quareshi and Lobo, 1994). In 2003, UN-HABITAT identified a range of behaviours that could facilitate transmission of diarrhoea diseases including cholera and taeniasis. Therefore, knowledge on transmission routes of diarrhoea diseases and sources of infections was found to reduce oral-faecal infections (Halvorson, 2004). 34 CHAPTER THREE 3.0 METHODS AND MATERIALS 3.1 Study Area The study was conducted in Lokichoggio, Kakuma and Central Divisions of Turkana District. The three Divisions were purposively selected as the Ministry of Health and UNICEF had planned to implement a sanitation and hygiene programme in these areas. A map of the referenced areas is provided in appendix 4. 3.2 Study population The study participants were mothers living in the three Divisions who had children aged less than five years. 3.3 Inclusion/Exclusion criteria A household with children of five years of age and below, mothers living in the selected Divisions who consented to participate in the study after having being identified using the randomized selection. Any person who did not meet the criteria was not involved in the study. 3.4 Ethical Issues Prior to data collection, clearance was obtained from the National Council for Science and Technology, Ethics and Research Review Committee of Ministry of Health. The District Medical Officer of Health in Turkana District (appendix 5) was also informed and permission sought. The purpose of the study was explained to the participants in the Turkana language before seeking their consent. Participants were treated with respect 35 and dignity and informed of their rights to withdraw at any stage of the interview. The participants were assured that all the information given would be kept confidential and used only for the purpose of the study and no names were required. All the participants were informed that there was no unforeseen risk, pain or discomfort to be occasioned participation in the study and neither the relatives nor partners would suffer the same. Community leaders were consulted in the whole process of data collection and to further involve the communities. Respondents were informed that there was no direct benefit to be accrued and there was no money to be paid for participating in the study. However, their participation would generate knowledge which could be used for the general benefit of the public and especially their community. 3.5 Study design The study adopted a longitudinal/cohort design. This design was chosen because a control or comparison condition could not be found neither was it desirable. For each participating household, baseline measures were taken two months before the interventions and end line measures taken two months to the end of the one year interventions. The intervention entailed distribution of 6,150 water filters and PUR sachets to 10,000 households for home based water treatment and development of the capacities of 36 women as duty bearers to create awareness, knowledge and demand for the water filters and ensure that safe water is used in households to reduce environmental risks to children health. TOTs were trained on Participatory Hygiene and Sanitation Transformation (PHAST) coupled with Community Led Total Sanitation (CLTS) combined with animated video. Upon completion of the training, the TOTs were given the PHAST training tools to enable them carry out sensitization at household levels. They used audio-visual shows blended with CLTS to ignite community dialogue among the people. The process also involved the production of culture-specific participatory training tools and videos tailored with appropriate messages. 3.6 Sample size determination The formula by Lemeshow et al., (1990) used in WHO health related studies was employed to determine the required sample size for this study. n=/2 P (1-P) P1 (1- P1 ) P2 (1- P2 )2 (P1-P2) 2 Where; n = Population sample P= P1 P2 ; Pooled proportion of disease (diarrhoea) 2 /2 = 1.96 ; Significance level, 0.05 = 95 % CL =1.28 ; Study power 1-P= Proportion without disease 37 P1= Baseline diarrhoea prevalence, where from previous studies it is estimated at 25% P2 = Post intervention diarrhoea prevalence estimated at 12.5%, assuming that the intervention will reduce diarrhoea prevalence by 50%. This gave a minimum sample size of approximately 140. Considering a maximum design effect of 2, this gave a sample size of (1402) = 280.This was approximated to 300. 3.7 Population Sampling Procedure A comprehensive sampling frame was required from where the sample would be drawn. In this study the Primary Sampling Unit (PSU) was the Central Bureau of Statistics (CBS) Enumeration Area (EA)1, which was taken as cluster. The Eas have maps showing the boundaries and structures as well as total households and population by sex as per the 1999 Housing and Population Census. In order to have updated details and representative sampling frame, a listing exercise was done. The listing involved updating the number of households, numbering the structures and updating the age composition of the household. After the listing exercise, the sampling interval for the Division was then determined and a filter done to include in the sample only the households with women having children less than 5 years of age. A total of 30 clusters in all the 3 Divisions were selected for study using the systematic Probability Proportional to Size (SPPS) sampling method. 1 For ease of carrying out the 1999 Housing and population Census, CBS created small non-overlapping units called Enumeration Areas (EAs), from each of the sub location, which were defined according to a specified measure of size (MoS). 38 3.8 Data collection methods 3.8.1 Field Questionnaire Research assistants were recruited with consideration given to those who had completed twelve years of formal education and were conversant in English and Turkana language. Research assistants were given a two day’s training on the data collection tools and pre-tested a few questions. Results of the pre-testing exercise were discussed and corrections incorporated in the questionnaire. A household survey was carried out before and after interventions based on a structured household questionnaire and observations. The spot checks were made on structural elements around the homesteads to determine hand washing behaviours particularly use of soap during hand-washing. The key indicators used to determine hand-washing behaviour among: respondents were; dedicated hand washing station, use of soap for washing hands, proportion of respondents who reported washing of their hands during the critical junctures and percent of care givers who reported washing hands with soap during most times that hands are washed. These indicators were used to collect information on hygienic behaviour and practices. On gauging changes in knowledge, structured questions were asked on two parameters; importance of latrine use and knowledge of diseases associated with use of contaminated water prior and after the intervention. Correct response was treated to mean that the person was knowledgeable on the subject matter. 39 3.8.2 Laboratory specimen processing 1. Water Quality Assessment Procedure Water samples were taken at the point of use in the households for further examination in the laboratory for chlorine level and presence or absence of faecal coliforms. The levels of chlorine were detected using DPD complex tablets. The DPD tablets dissociated if any chlorine compounds were present in the sample. The samples were analysed for chlorine levels using calorimetric machine from which the chlorine optical density (OD) in the sample was taken and recorded. The calorimeter was calibrated using pure water with zero traces of chlorine and chlorine level of less than 0.2 mg/l was regarded as low and in-effective while chlorine levels of more than 0.2 mg/l was regarded as effective in protecting the water from bacterial contamination. Bacterial contamination was detected by presence or absence of faecal coliforms using Filter Membrane Technique. One hundred millilitres (100 ml) of water sample was filtered through a membrane filter embedded with media. The membrane was then cultured on a pad of sterile selective broth containing an indicator. After incubation, the number of coliforms colonies was counted. This gave approximate number of E.coli in One hundred millilitres (100 ml) of water. Detailed description of Filter Membrane Technique is as outlined in the next sub-section below. Water microbiological assessment Procedure using Filter Membrane Technique 40 Water microbiological analysis was done by determining the Total Coliforms(TC) and Escherichia coli(EC) by Membrane Filtration using a simultaneous detection technique(MI Medium) as described by Brenner et al 1993.This is a method that describes a sensitive and differential membrane filter (MF) medium using MI agar or MI broth for the simultaneous detection and enumeration of both total coliforms (TC) and Escherichia coli (E. coli) in water samples in 24 hours on the basis of their specific enzyme activities. Two enzyme substrates, the fluorogen 4-Methylumbelliferyl–βDgalactopyranoside (MUGal) and a chromogen Indoxyl- β –D-glucuronide (IBDG), are included in the medium to detect the enzymes β-galactosidase and β –glucuronidase respectively produced by TC and E. coli, respectively. Briefly, 100ml of Water samples were collected in sterile polypropylene sample containers with leak proof lids and filtered through a 47-mm, 0.45-µm pore size cellulose ester membrane filter that retains the bacteria present in the sample. The filter was then placed on an absorbent pad saturated with 2-3mL of MI broth and the plate incubated at 35°C for up to 24 hours. The bacterial colonies that grow on the plate were inspected for the presence of blue color from the breakdown of IBDG by the E. coli enzyme β –glucuronidase and fluorescence under longwave ultraviolet light (366 nm) from the breakdown of MUGal by the TC enzyme β –galactosidase. The total E.coli and TC counts Per ml of the water sample was then determined according to the guidelines of the Microbiology Manual described by Bordner et al 1978. 41 Stool microbiological analysis The mothers and guardians were requested to collect stool specimen from their children aged less than five years for analysis. Laboratory investigations for sanitation and hygiene related diseases were carried out. The stool specimens were examined for presence or absence of diarrhoea causing agents such as E.coli, Salmonella and Shigella, through procedure and techniques described by Cheesbrough (2000). On arrival in the laboratory, the stool samples collected from the field were examined carefully and noted the consistency of the specimens, including the following; the colour of the stool, whether the stool was formed or semi- formed, uniformed or fluid and the contents (i.e. blood, mucus or pus) Stool microscopy for ova and cysts All stool samples were tested for the presence or absence of intestinal helminths and protozoa using direct faecal smears (saline and iodine mount preparation) as described Cheesbrough (2000). Briefly, the stool samples were appropriately labelled in order to match with laboratory number of the subjects. A drop of saline was put on the center of the left half slide and a drop of iodine was placed in the center of the right half of the slide; then with an applicator stick, a small portion of the faeces (approx. 2g) which is about the size of the match stick head was added to the drop of iodide, and mix with the faeces to form a suspension ;then this was covered with a cover slip, after which the preparation were 42 examined using the ×10 objective or if needed for identification by using higher power in a systematic manner so that the entire area is observed. When organisms were seen, one may switch to a higher magnification to see a more detailed morphology of the object in question. Stool Culture, isolation and identification of pathogens Processing of stool specimens The isolation of enteric pathogens was done as described by Ewing and Edwards (1986). Briefly, stool specimens were cultured for salmonella Shigella and E. Coli spp in Xylose lysine dextrose (XLD), Salmonella shigella medium (SS) and MacConkey agar (Difco Laboratories, Detroit, Mich.). Stool culture for vibrio spp was done on Thisulphite citrate bile salts agar(TCBS) medium. Enrichment for Shigella,salmonella and E.coli was performed by culturing the specimens into selenite F broth (Oxoid, UK) while that for vibrio was done on Alkaline peptone water(APW). All the inoculated culture media were incubated at 37°C for 24 hours. The selenite F broth and APW were then sub cultured onto SS,XLD and MacConkey agar plates and TCBS respectively and incubated as described above. The agar plates were examined colonies presenting as non lactose fermenters and non hydrogen actose (H2S) gas producers. These characteristics are used to distinguish 43 e.coli,salmonella and Shigella spp from each other. The actose fermenters colonies from TCBS were selected as suspect vibrio spp. Identification of pathogens Biotyping with test tube media Biochemical identification of the enteric bacterial pathogens was done using Triple sugar iron agar (Oxoid, UK),Lysine indole motility medium(Oxoid, UK),Simmons citrate (Oxoid, UK),Methyl Red-Vogues Proskeur medium(MR-VP)(Oxoid, UK) and Urea agar (Oxoid, UK).The tests were performed as described in the clinical microbiology procedures handbook (Isenberg,1992). In addition string test and catalase test were performed for identification of vibrio cholera spp. The identity of the respective pathogens was done based on their specific reactions in the above biochemical media as shown in the chart (Appendix 3). Biochemical identification by serotyping The identity of the pathogens was confirmed by serotyping the colonies using the genius/type specific antisera (Oxoid, UK) according to manufacturer instructions. 44 3.9 Data Management and analysis The quantitative data was entered into SPSS version 17.0. Frequencies were run and then data cleaning was done. For qualitative data, the tapes were transcribed then content analysis (identifying, coding, and categorizing the primary patterns in the data) was then done. Actual analysis involved calculation of case prevalence, independence tests and goodness of fit using χ2 test and associations using regression lines; these tests are as detailed below; For those variables with nominal or ordinal scale, the chi-square goodness of fit test was applied to ascertain the significance of any observed changes between 2007 (baseline) and 2008 (post-intervention). The null hypothesis for this test is that there was no difference in the observed proportions within the two periods (similar). For tables with two rows and two columns, Pearson chi-square, the likelihood-ratio chisquare, Fisher’s Exact test, and Yates’ corrected Chi-square (continuity correction) were applied. For 2 × 2 tables, Fisher’s Exact Test was computed when a table that does not result from missing rows or columns in a larger table has a cell with an expected frequency of less than 5. Yates’ corrected chi-square was computed for all other 2×2 tables. For tables with any number of rows and columns, it is understood that when both table variables are quantitative, Chi-square yields the linear-by-linear association test. 45 For variables with continuous data, Student’s t-test was used to compare sample means by calculating Student’s t and display the two-tailed probability of the difference between the means. Overall measurement of association between the independent variable (core outcome) namely, chlorine level in mg/l and faecal coli forms in 100mls with key dependent variables (modifiable risks targeted during intervention was ascertained through logistic regression modeling. 3.10 Study Limitations From literature, it is indicated that evaluation of handwashing practices should best be observed, however, this was not possible in this study since the population is sparsely distributed and therefore self-reported information was gathered. There could also have been Hawthorns effect due to the fact that the households had been visited at baseline and a repeat survey was done at end line (within 1 year). In addition, Turkana District is an ASAL area and water is scarce, limiting water availability for hand washing. 46 CHAPTER FOUR 4.0 RESULTS 4.1 General overview A total of 300 respondents interviewed at baseline (2007) were followed up and reinterviewed at end-line (2008). All of them were mothers with children aged less than five years as stated in the inclusion criteria. Their demographic and distribution characteristics are as outlined in subsequent sub-sections. 4.2 Key Demographic Variables This sub-section covers the core demographic variables relevant to this study. Figure 3 shows the overall distribution of respondents across the three Divisions of Turkana District: - 4.2.1 Distribution of Respondents by Division Notably, Lodwar Central Division had the highest proportion of respondents at 46.7% (n=140) whereas Kakuma and Lokichogio had equal proportion of respondents each at 26.7% (n=80). 47 Figure 3: Distribution of Respondents by Division The respondent distribution was proportional to the population density in each of the three Divisions. 48 4.2.2 Distribution of Respondents by Age High proportion of respondents (36.3%) were aged between 26 and 35 years, followed by those aged between 14 and 25 years (26.3%) and the rest were aged above 36 year. The age distribution of the respondents is as shown in Figure 4. Figure 4: Age distribution of study respondents Overall, respondents aged between 26-35 years formed the majority of the sampled population in all the three Divisions except in Kakuma where those aged over 46 years formed a slightly higher proportion (24%). Figure 5 shows age distribution of respondents across the three Divisions. 49 Respondent's age distribution by Division 100% > 46 yrs 36-45 yrs 26-35 yrs 14-25 yrs 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Kakuma Lodwar Central Lokichogio Figure 5: Respondent’s Age Distribution by Division Notably, the observed differences in age distribution of respondents across the three Divisions were significant (P=0.003). This shows that there is potential of masking inter-divisional differences and confounding if data segregation by Division and age group is not considered during analysis. 4.2.3 Education level of Respondents Regarding education level of the respondents, out of the 300 interviewees, the highest proportion (43%) had primary level education followed by those with no education (35%) whereas 22% had post-primary education. This is depicted in Figure 6: - 50 Figure 6: Highest Education Level of the Respondent In addition, the proportions on education level were however different across the Divisions. For Kakuma, majority 39 (49%) had primary education, 24 (30%) had no education, while 17 (21%) had post-primary education. For Lodwar central, majority 67 (48%) had primary education, 50 (36%) had no education, while 23 (16%) had postprimary education. For Lokichogio, majority 31 (39%) had no formal education, 26 (33%) had post-primary education, while 23 (29%) had primary education. This is as shown in Figure 7: - 51 Distribution of Respondent’s Level of Education by Division 100% 80% 60% 40% 20% 0% Kakuma No Formal Education Lodwar Central Primary Lokichogio Post-primary Figure 7: Distribution of Respondent’s Level of Education by Division These observed differences in distribution of education level of respondents across the three Divisions were significant (P=0.017), hence not attributable to chance. This shows that there is potential of masking inter-regional differences and confounding if data segregation by Division and level of education is not considered during analysis. 4.2.4 Latrine Distribution by Division Latrine structure and distribution across the three Divisions was only checked at baseline and classified as either temporary or permanent based on material used for the super-structure. Out of the 243 (81%) of households with latrine, it was noted that majority (54.7%) were temporary. Within the Divisions, Lokichogio had the highest proportion of temporary latrines at 58% (39), followed by Lodwar central having 56% 52 (67) and then Kakuma with 48% (27). The alternative proportions represent permanent latrine structures as shown in Figure 8: - Distribution of Latrine Type by Division 100% Proportion (%) 80% 27 67 39 53 28 Lodw ar Central Lokichogio 60% 40% 20% 29 0% Kakuma Permanent Temporary Figure 8: Distribution of Latrine Type by Division Notably, the observed differences in distribution of latrine structure by Division were not statistically significant (P=0.51). The study also sought to highlight the factors that affect provision of toilets at household level. For those households without toilet facilities at baseline (19%), the main reasons for not having a toilet in the household level were geophysical and economic constraints to construct (51.7%) followed by availability of a bush hence pointed that they did not need one (48.3%). The trend and reasons did not change after 53 the intervention (P=0.242) as geophysical and affordability was still identified as the main set back to having a toilet in the households. This is as detailed in Table 1: - Table 1: Reason for not having toilet facility (2007 and 2008) Reasons for no toilet facility at baseline (2007) geophysical and economic constraints Do not need one Total Reasons for no toilet facility after intervention (2008) geophysical & economic Do not need constraint one Total 36.4% (104) 15.4% (44) 51.7% (148) (30.8%) 88 67% (192) 17.5% (50) 48.3% (138) 32.9% (94) 100% (286) X 2=1.368; P=0.242 4.3 Knowledge and Practices of Sanitation and Hygiene Before and After Intervention This part considered changes in latrine management, drinking water handling methods and hand-washing practices among mothers before and after the intervention. 4.3.1 Change in Knowledge of latrine importance There was a slight increase in the proportion of population that regarded latrines as important from 70% in 2007 to 80.2% in 2008. This noted change was not of statistical significance (χ2 =1.196 P=0.274). The breakdown in Table 2; 54 Table 2: Cross-tabulation of whether latrine is important in 2007 and in 2008 2007 2008 χ2 P-value Is latrine important Count (% of Total) Count (% of Total) Yes 205 (70%) 235 (80.2%) 1.196 0.274 No 88 (30%) 58 (19.8%) Regarding change in latrine importance, those who associated latrine with reduction in diseases increased from 44.3% to 62.3%. The study expectation was that respondents would associate latrines with disease prevention which was the focus of sanitation promotion. The noted change was of no statistical significant (χ2 =8.588, P=0.476) and details are as outlined in the Figure 9: - Figure 9: Distribution of knowledge on latrine importance (2007 and 2008) Regarding change in knowledge on diseases associated with drinking contaminated water, it was noted that knowledge on typhoid increased from 8.7% in 2007 to 44.2%, 55 cholera from 27.3% to 37.7%. More over that of general diarrhoeal diseases reduced from 20.3% to 6.1% owing to the enhanced awareness that diarrhoea diseases are not necessarily due to unsafe water but to general hygiene and sanitation factors including hand washing with soap. The overall change was however not statistically significant (P=18.7, χ2=.768), details are as shown in Table 3: - Table 3: Knowledge on diseases associated with drinking unsafe water Disease associated with unsafe water (2008) Typhoid Diseases Typhoid associated with unsafe water Cholera (2007) Total 4.3.2 Cholera 10 (4.3%) 6 (2.6%) 28 (12.1%) intestin al worms Diarrhoea Malaria 1 1 (0.4%) (0.4%) URTI 1 (0.4%) 24 2 6 (2.6%) 1 (0.4%) (10.4%) (0.9%) 1 (0.4%) HIV/AI DS Total 0 20 (8.7%) 1 1 63 (27.3%) (0.4%) (0.4%) intestinal worms 33 (14.3%) 23 (10%) 2 3 (1.3%) (0.9%) 3 (1.3%) 1 2 (0.4%) (0.9%) Diarrhoe a 22 (9.5%) 20 (8.7%) 1 1 (0.4%) (0.4%) 2 (0.9%) 1 (0.4%) 0 47 (20.3%) Malaria 9 (3.9%) 14 (6.1%) 3 3 (1.3%) (1.3%) 4 (1.7%) 1 (0.4%) 0 34 (14.7%) 102 (44.2%) 67 (29%) 87 9 14 (6.1%) 11 (4.8%) 5 3 (37.7%) (3.9%) (2.2%) (1.3%) Change in hand washing practice Washing of hands in the three universally accepted critical times, namely; after visiting a toilet, before cooking and before eating was also evaluated. Regarding change in hand washing practice in Turkana District, those who wash hands regularly increased from 73.5% to 91.3%. The detailed distribution is as shown in the Table 4: - 56 231 (100%) Table 4: Change in hand washing prevalence (2007 and 2008) Hand washing frequency 2007 Yes No Not always Total Hand washing frequency 2008 Not No always Total Yes Count Count Count (%) Count (%) (%) (%) 205 (68.8%) 6 (2%) 8(2.7%) 219 (73.5%) 0 14 (4.7%) 3 (1%) 11 (5.7%) (0.0%) 53 (17.8%) 3 (1%) 6 (2%) 62 (20.8%) 272 (91.3%) 9 (3%) 17 (5.7%) 298 (100.0%) On the above observed changes in hand washing in 2007 and 2008, the overall change was slightly significant (χ²=9.34, P=0.053). The results of hand-washing practice by age showed that there were changes across agegroups. The most significant change was observed in age group 36-45 years, whereby the proportions increased from 66.7% to 88.9% (χ2 =10.014, P=0.04). Some improvements were noted in other age groups but were not statistically significant. In age group 14-25 years, the proportion of those who wash hands regularly increased from 83.5% before intervention to 94.9% after intervention (χ2 =0.515, P=0.773). Handwashing practice also improved in age group 26-35 years, with those who wash hands regularly increasing from 76.9% in 2007 to 93.5% in 2008 (χ2 =1.369, P=0.849). In age group above 46 years, the proportion increased from 58.3% to 83.3%. The detailed distribution is as shown in Table 5: - 57 Table 5: Change in hand washing in 2007 and 2008, grouped by age group Washing of hands by age group 14-25yrs Yes (n=79) No Not always 26-35yrs Yes (n=108) No Not always 36-45yrs Yes (n=63) No Not always Over 46yrs Yes (n=48) No Not always 4.3.3 2007 Count (% of Total) n=298 66 (83.5%) 2 (2.5%) 11 (13.9%) 83 (76.9%) 7 (6.5%) 18 (16.7%) 42 (66.7%) 5 (7.9% 16 (25.4%) 28 (58.3%) 3 (6.3%) 17 (35.4%) 2008 Count (% of Total) n=298 75 (94.9%) 0 (0%) 4 (5.1%) 101 (93.5%) 3 (2.8%) 4 (3.7%) 56 (88.9%) 2 (3.2%) 5 (7.9%) 40 (83.3%) 4 (8.3%) 4 (8.3%) χ2 0.515 Pvalue 0.773 1.369 0.849 10.014 0.04 4.105 0.392 Change in presence of hand washing practice Presence of hand washing soap in the house was used as a proxy indicator to handwashing practices. It was observed that within respondents with no education, soap presence increased from about 65% to 78%, those with primary education increased from about 58% to 69% while hand washing soap presence in households among those with post-primary education increased from about 68% to 81%. This is as shown in Table 6: Table 6: Presence of soap in the house in 2007 and 2008, grouped by education level Presence hand washing soap No education Primary Post-primary Yes No Yes No Yes No 2007 Count (% of Total) 68 (65.4%) 36 (34.6%) 74 (57.8%) 54 (42.2%) 44 (67.7%) 21 (32.3%) 58 2008 Count (% of Total) 81 (77.9%) 23 (22.1%) 89 (69.5%) 39 (30.5%) 53 (81.5%) 12 (18.5%) χ2 P-value 3.871 0.049 0.031 0.860 0.359 0.549 The changes on presence of soap in house in 2007 and 2008 observed above shows that those with no education was significant (χ²=3.87, P=0.049) hence not likely to have been by chance whereas that of those with primary or post primary education might be attributed to chance error (P>0.05). 4.3.4 Change in storage of drinking water practices Regarding storage of drinking water practices, in Kakuma Division, those who kept drinking water from closed containers increased from 35.5% to 80.5%. In Lodwar Central, they increased from 37.7% to 77.5% while in Lokichogio, they increased from 39.5% to 80.3%. The detailed distribution is as shown in Table 8: - Table 7: Drinking water storage in 2007 and 2008, grouped by Division 2007 Count (% of Storage of water for drinking Total) open container 49 (64.5%) Kakuma closed 27 (35.5%) container Lodwar Central open container 86 (62.3%) closed 52 (37.7%) container open container 46 (60.5%) Lokichogio closed 30 (39.5%) container 2008 Count (% of Total) 15 (19.7%) 61 (80.3%) χ2 P-value 1.967 0.161 31 (22.5%) 107 (77.5%) 0.953 0.329 15 (19.7%) 61 (80.3%) 1.503 0.220 The changes noted above in drinking water storage were not statistically significant (P>0.05), hence may be attributable to chance error. 59 4.3.5 Change in handling and disposal of children faeces The study also assessed methods of disposal of children faeces by observations and interviews. At baseline, 61.8% (173) of the respondents disposed their children faeces in the open by crudely throwing it in the compound or in the nearby bush. After the intervention, open disposal of children faeces by the mothers decreased significantly to 43.2% (121). Very few mothers buried or covered the faeces with soil at baseline (38.2%), however the practice changed significantly after intervention with 56.8% of the mothers covering the faeces of their children with soil. This is as detailed in Table 9: - Table 8: Way of disposing off children faeces Way of disposing off Leave it in the yard faeces (2007) and do nothing Bury it Total Way of disposing off faeces (2008) Leave it in the yard and do nothing Bury it 25% (70) 36.8% (103) Total 61.8% (173) 18.2% (51) 20% (56) 43.2% (121) 56.8% (159) 38.2% (107) 100% (280) The study also assessed faecal contamination within the compound mainly through spot observations. There was some non-statistically significance improvement against indiscriminate disposal of faeces in the compound after the intervention. Prior to the intervention, it was observed that 131 (43.7%) of the compounds were littered with faeces compared to 95 (31.7%) after intervention. This is as detailed in Figure 10: 60 Figure 10: Contamination of compound with faecal matter 4.4 Change in Health Outcome as Measured by Surrogate Parameters The results in this section detail the observed changes in the quality of drinking water at the point of use as measured by chlorine level, faecal coliform counts, changes in faecal oral transmitted diseases, changes in microbes in stool of children aged below five years. 4.4.1 Chlorine level and Faecal Coliform Count before and after intervention As an indicator and measure to reduced risk of ill health, residual chlorine test was carried out in households that claimed to be treating their water or consuming treated water. Chlorine level of less than 0.2 mg/l as cut off was regarded low and in-effective against harmful microbes; levels of chlorine of more than 0.2 mg/l in water were regarded effective in protection against bacterial contamination. Overall, there was marginal change in proportion of households whose drinking water had residual chlorine of more than 0.2 mg/l; in Kakuma, the proportion of households whose drinking water had residual chlorine of more than 0.2 mg/l increased from 12.9% in 61 2007 to 22.6 in 2008. Similar marginal changes were noted for Lodwar Central and Lokichogio Divisions as shown in Table 10: - Table 9: Chlorine Level in 2007 and in 2008 Chlorine Level Kakuma >0.2 mg/l <0.2 mg/l Lodwar Central >0.2 mg/l <0.2 mg/l Lokichogio >0.2 mg/l <0.2 mg/l 2007 Count (% of Total) 8(12.9%) 54 (87.1%) 10(15.6%) 54 (84.4%) 10(16.1%) 52 (83.9%) 2008 Count (% of Total) 14(22.6%) 48 (77.4%) 9(14.1%) 55 (85.9%) 11(17.7%) 51 (82.3%) χ2 P-value 2.679 0.102 0.162 0.687 0.042 0.838 The proportion of households which had water with chlorine levels above 0.2 mg/l marginally increased though the changes recorded were not statistically significant. These observations are consistent with field expectations since there were no direct interventions targeting increased chlorine use. This was by design so as to avoid possible confounding effects on faecal coliform count arising from the known effects of chlorine in reducing diarrhoea related diseases as compared to changing mothers’ behaviour. Regarding observed changes in faecal coliform counts per 100 ml sample, there were significant variations between 2007 and 2008. The reduction in mean faecal coliform counts was notable in all divisions; in Kakuma, mean faecal coliforms per 100 ml sample reduced from 72.6 to 26.2 colony units, similar results were recorded in Lodwar 62 Central where the number reduced from 83.7 to 22.6 units, while in Lokichogio Division, the number reduced from 51.6 to 22.6 units. This is as shown the Table 11: - Table 10: Paired Samples Statistics on faecal coliforms per 100 ml sample, grouped by Division Division faecal coliforms in 100 Kakuma mls in baseline faecal coliforms in 100 mls in post intervention Lodwar Central faecal coliforms in 100 mls in baseline faecal coliforms in 100 mls in post intervention faecal coliforms in 100 Lokichogio mls in baseline faecal coliforms in 100 mls in post intervention 95% CI Sig. Std. N Mean Deviation Lower Upper (2-tailed) 62 72.58 102.9 46.44 98.72 0.005 49 26.18 24.9 61 83.75 113.1 79 22.59 21.5 17.79 27.40 60 51.62 68.4 33.94 69.29 0.006 39 22.59 16.7 17.16 28.02 19.02 33.35 54.78 112.73 0.003 The table above shows that there were significant differences in proportion of sample with faecal coliform count at baseline (2007) and after intervention (2008). 63 4.4.2 Diarrhoea prevalence in children aged less than 5 years (before and after intervention) The overall prevalence of diarrhea among children a month before the study reduced from 43.7% in 2007 to 30.7% in 2008. This is shown in Figure 11 below: Figure 11: Diarrhoea in children in the last one month prior and after the intervention (2007-2008) There was consistent reduction in diarrhoea among children as reported by mothers and by level of education of mothers. Children of mothers with no education reported about 10% reduction in diarrhea (42.9% in 2007 to 35 (33.3%) in 2008, those of mothers with primary education reducing from 48 (37.2%) in 2007 to 41 (31.8%) in 2008, while those of mothers with post-primary education reducing from 38 (57.6%) in 2007 to 16 (24.2%) in 2008. This is detailed in the Table 12: - 64 Table 11: Cross-tabulation on child diarrhoea 1 month prior to study baseline (2007) and diarrhoea 1 month prior to study end-line (2008) by Education level of the respondent Did child have diarrhea 1 month prior to study No education No Yes Primary No Yes Post-primary No Yes 2007 Count (% of Total) 60 (57.1% 45 (42.9% 81 (62.8% 48 (37.2% 28 (42.4% 38 (57.6% 2008 Count (% of Total) 70 (66.7%) 35 (33.3%) 88 (68.2%) 41 (31.8%) 50 (75.8%) 16 (24.2%) χ2 P-value 0 1 0.01 0.920 4.846 0.028 As depicted in Table 15 above, the noted reduction in prevalence of diarrhoea increased with education. The observed changes where only statistically significant for the children of mothers with post-primary education (χ²=4.85, P=0.028). 65 4.4.3 Diarrhoea related microbes in children stool before and after intervention A total of 230 stool specimens from children aged less than five years were examined at baseline and one year thereafter (end-line). From the 230 stool samples examined, the proportion of children from whom infectious pathogens of Proteus spp. was isolated, reduced from 30 (16%) to 16 (7%), E. coli reduced from 125 (54%) to 95 (41%) while salmonella spp. increased from 6 (1%) to 19 (8%). Specimen outside from children aged more than five years where excluded, they increased from 18 (8%) to 62 (27%). The detailed distribution of the microbes is as shown in Figure 12: - 60% 2007 Proportion (%) 50% 2008 40% 30% 20% 10% itr o ba ct er te r C te ro b ac sp En Sh ig e lla la el Sa lm on p. sp p. li Eco el la si Kl eb sp p. s Pr ot eu N o gr ow th 0% Microbes in children stool Figure 12: Distribution of Microbes in Stool specimens from Children Aged Less Than 5 Years at baseline and End line 66 Overall, prevalence of diarrhoea related microbes in children aged less than five years reduced from 91.3% in 2007 to 78.3% after intervention (2008); this is as depicted in Figure 13: - Figure 13: Diarrhoea related microbes in children stool at baseline and endline (20072008) However, it is clear from the statistics that there was no significant change in diarrhoea related microbes in children stool before and after intervention (χ2 =47.32, P=0.5). 4.4.4 Prevalence of Bacterial and Parasitic organisms in children aged less than 5 years The prevalence of bacterial and parasitic organisms from the stool of children aged less than five years was assessed through laboratory examination of stool samples in the laboratory. The results of the findings were as shown Table 13; 67 Table 12: Ova and Cyst and Bacterial and parasitic pathogens in stool Ova and Cyst in stool A Lumbricoides E histolytica trophozoite Giardia lamblia Trophozoite T. trichuris No Cyst/Ova Salmonella Shigella Total 2007 2008 Frequency (%) 10(3.5) 23(8.1) 10(3.5) 1(0.4) 224(78.6) 15(5.3) 2(0.7) 285 (100) Frequency (%) Chisquare 6(2.1) 12(4.1) 1(0.4) 0 262(90.03) 3(1.0) 7(2.4) 291 (100) Pvalue 0.1 0.25 0.35 0.74 0.62 0.85 4.1 8 2.78 0.04 0.005 0.096 From the 285 and 291 stool samples examined at baseline and after intervention respectively, potential infectious pathogen was isolated from 61 (21%) of the children at baseline and 29 (10%) of the children after intervention. Bacterial pathogens were isolated from 17 (6.0%) of the children at the baseline study and 10 (3.4%) of the children after intervention. Parasitic pathogens were isolated from 34 (15.5%) of the children at baseline and 19 (6.6%) of the children after intervention. 4.5 Linkages between mother’s improvement indicators behaviour and targeted health 4.5.1 Relationship between mother’s behavioural factors and Faecal coliform Count After establishing the significant variables related to health promotion role in improving mothers and children health, it was necessary to explore the statistical strengths of such variables in influencing the said outcome. This sub-section applies multivariate analysis 68 to explain the nature of such independent variables and quantifies their strengths in influencing the expected health outcome (dependent variable). To achieve this, regression models were applied. As shown in Figure 14, 65.7% of the population did not have faecal coliform in their drinking water samples. Figure 14: Change in faecal coliform count between 2007 and 2008 For comparative change (2007 and 2008), 20.1% of the households had faecal coliform reduction while 14.3% had FC increase and the rest had no report for various reasons including many children not able to produce stool. Out of the 91 respondents who 69 reported change in faecal coliform count per 100 ml of drinking water, majority (10.7%) had FC reductions of more than 50 units as compared to 10% with FC increase of 1 to 25 units per 100 ml drinking water sample. For 91 respondents who reported change in faecal coliform count per 100 ml of drinking water, the nature and strength of association with previously noted modifiable behavioural variables was explored through linear regression modelling. Notably, the resulting model had an R-square of 39.6% (P=0.048). This means that about 40% of the observed change in faecal coliform count per 100 ml of drinking water could be explained or attributed to the observed change in mothers behaviour. The specific modifiable risk factors under mothers behaviour are as summarized in Table 14: Table 13: Resulting model Coefficients on association between FC change and modifiable behavioural risk factors Unstandardized Standardized 95% Confidence Dependent Variable: Coefficients Coefficients Interval for B Faecal Coliform count Std. Lower Upper per 100ml (change) B Error Beta t Sig. Bound Bound (Constant) 1.724 1.043 1.653 .112 -.439 3.887 Age of the respondent 0.612 .233 0.412 2.624 .015 0.128 1.096 Reasons for no toilet 0.749 .241 0.508 3.107 .005 0.249 1.248 facility (2007) Do you have a toilet -1.662 .751 -.365 .038 -3.220 -.103 facility (2007) 2.211 Resulting model: Y=1.7 + 0.41X1 +0.0.51X2 - 0.36X3 Where; Y=FC count/100ml (change), X1= age of Respondent, X2= reason for no toilet in 2007, X3=Presence of toilet facility in 2007 70 Indicatively, the faecal coliform count can be determined (predicted) using key risk factors which are namely; age of Respondent (P=0.015), reason for no toilet in 2007 (P=0.005), and presence of toilet facility in 2007 (P=0.038). The resulting model was highly suitable as shown by the test of residuals represented by the histogram and normal probability plots shown in Figure 15: - Figure 15: Normal probability plots of residuals 71 The model as depicted above indicates that the observed residual probabilities are highly correlated to those resulting from the model hence an indication of model goodfit to the observed data as shown in Figure 16: - Figure 16: Histogram on dispersion of residuals As an indicator of model appropriateness, the residuals (un accounted variability by the model) are randomly distributed hence fit in a normal distribution curve as shown above. 72 4.5.2 Relationship between mother’s behavioural and related factors and diarrhoea microbes in children stool From a multi-variate regression using forward stepwise removal (likelihood ratio), the association between the noted reduction of diarrhoea related microbes in children stool of 91.3% in 2007 to 78.3% after intervention (2008) is based on the modifiable risk factors outlined in Table 15: - Table 14: Association between microbes in children stool, mother’s behaviour and related factors Variables in the Equation 95% C.I. for EXP(B) B S.E. Sig. Exp(B) Lower Upper Age -0.54 0.45 0.227 0.58 0.24 1.40 Education 1.95 0.91 1.17 41.92 0.033 7.02 Toilet’08 -4.29 1.88 0.00 0.54 0.022 0.01 Distance’08 3.39 1.17 295.60 0.004 29.71 2.99 Water sources; 0.019 Sources(Open 7.28 2.34 144253.71 0.002 1456.0 14.70 well) 6 Sources(spring) -.12 1.27 0.01 1 0.928 0.89 0.07 10.66 Sources(river) 2.82 1.34 4.40 1 0.036 16.71 1.20 232.32 Treatment’08 3.31 1.34 6.13 1 0.013 27.40 1.99 376.87 Storage’08 -2.44 1.33 3.35 1 0.067 0.09 0.01 1.19 Constant -32.98 8182.10 0.00 1 0.997 0.00 Resulting model: Y= -32.98 -0.54X1+1.95X2 –4.29X3 +3.39X4 +(coeff. of applicable water source) Wal d 1.46 4.56 5.22 8.37 9.91 9.65 d f 1 1 1 1 3 1 Where; Y= Microbe in stool in 2008 (Reclassified), X1= age of Respondent, X2= education level of respondent, X3=Presence of toilet facility in 2008, X4=distance from toilet facility in 2008 The driving factors to diarrhoea related microbes in children stool could thus be linked strongly to mothers behavioural characteristics; namely mother’s education, toilet 73 availability, distance to toilet, source of drinking water, treatment of drinking water and storage of the drinking water. The strength of the model as judged by its ability to classify correctly whether the respondent’s child stool has diarrhoeal related microbe or not is judged from its overall positive predictive value (PPV) which in this case was 92.7% as shown in Table 16: Table 15: Classification table on the association between microbes in children stool and mothers behaviour Predicted Microbe in (Reclassified) stool in 2008 Diarrhoeal No growth/Not Percentage related microbes applicable Correct Observed Microbe in stool in Diarrhoeal related microbes 65 2008 No growth/Not applicable 4 (Reclassified) Overall Percentage 2 97.0 11 73.3 92.7 The above table shows that the microbes in stool prediction model was able to correctly predict 97% of the samples with diarrhoeal related microbes (sensitivity) and 73.3% of samples without diarrhoeal related microbes (specificity) with an overall PPV of 92.7%. 74 4.5.3 Association between modifiable behavioural and related factors and diarrhoea prevalence in children aged less than 5 yrs From binary logistic regression using forward stepwise removal (likelihood ratio),the association between the noted diarrhoea prevalence reduction from 43.7% (in 2007) to 30.7% after intervention (2008) in children aged less than five years is based on the modifiable risk factors outlined in Table 17: Table 16: Association between modifiable behavioural and related factors and diarrhoea in children aged less than 5 Years Variables in the equation/predictors Diarrh2007 education structure Latrine08 clorine08 Constant B 2.247 -1.770 3.959 3.322 -6.759 -5.147 S.E. 1.029 .698 1.267 1.587 3.507 2.602 Wald 4.770 6.429 9.765 4.381 3.713 3.914 df 1 1 1 1 1 1 Sig. 0.029 0.011 0.002 0.036 0.054 0.048 Exp(B) 9.459 .170 52.416 27.719 .001 .006 95% EXP(B) Lower 1.259 .043 4.375 1.235 .000 C.I.for Upper 71.049 .669 627.952 621.926 1.123 Resulting model: Y= -5.15 + 2.25X1 -1.77X2 + 3.96X3 + 3.32X4 -6.76X5 Where; Y=FC count/100ml (change), X1= Diarrhrea prevalence in 2007, X2= education level of respondent, X3=latrine structure X4=Latrine presence in 2008, X5=latrine Chlorine level in 2008 The risk factors for diarrhea in children aged less than five years after intervention (2008) are mainly behavioural characteristics; namely if the child had diarrhoea at baseline (2007), mother’s education, latrine availability, latrine structure and chlorine level in the drinking water after the intervention (2008). 75 The strength of the associative model as judged by its ability to classify correctly whether children aged less than five years suffered from diarrhoea episode or not is judged from its overall positive predictive value (PPV) which in this case was 77.8% as shown in Table 18: Table 17: Classification table on the association between sanitation and hygiene promotion and diarrhoea in children aged less than 5 Years Predicted Observed Did child have diarrhoea 1 month prior to study (2008) Percentage No Yes Correct Step 5 Did child have diarrhoea 1 No 17 6 73.9 month prior to study (2008) Yes 4 18 81.8 Overall Percentage 77.8 a. The cut value is 0.5 The table above shows that the diarrhoea predictive model was able to predict73.9% of the non-diarrhoeal (specificity) related samples correctly and 81.8% of the diarrhoea samples (sensitivity) correctly with an overall PPV of 77.8%. 76 CHAPTER FIVE 5.0 DISCUSSION, CONCLUSION AND RECOMMENDATIONS 5.1 Discussion The function of hygienic behaviour is to prevent the transmission of the agents of infection. In a previous study, effects of improved environmental sanitation conditions and hygiene practices on preventing occurrence of diarrhoea among children under five years included washing and purifying fruits and vegetables; domestic water reservoir conditions; faeces disposal, presence of vectors in the house and flooding in the lot (Heller et al., 2003). This study compares with that of Heller et al., 2003. The study intervention was to change mothers sanitation and hygiene behaviour and practices to impact on improving children health in Turkana District. The targeted behaviour and practices included: House hold water treatment and safe storage, Hand washing with soap, Provision and use of latrine and safe disposal of children faecal matter. These interventions were targeting mothers of children under five years of age whose outcome was envisioned to be reduction of diarrhoeal among children under five years in the study area. Two approaches were used to deliver the interventions; Community led total sanitation (CLTS) and Participatory hygiene and sanitation transformation (PHAST). 77 This part of the report delve into the possible reasons in support of key findings on mother’s behaviour and influence on the health of children aged less than five years in Turkana District and possibly other areas of similar socio-economic constraints. This was by comparing the findings with previous studies undertaken elsewhere. 5.1.1 Changing community sanitation and hygiene knowledge and practices Inadequate sanitation is a major cause of infectious diseases globally and improving sanitation is known to have a significant beneficial impact on health both at household level and across communities. Provision of latrines as a measure to prevent communicable disease cannot thus be over emphasized and one of the interventions for this study was provision of basic latrines under the community total led sanitation (CLTS). The communities’ knowledge on importance of latrines in this regard seems not to have increased significantly as expected with a significant number giving privacy as the priority reason for use of latrine 33.7% of the respondents compared to 62.3% who associated latrines with disease prevention. Socio-cultural and contextual factors such as, low socioeconomic status, low education levels, social instability and gender disparities can lead communities to compromise in hygiene and sanitation issues. Turkana District has acute water shortage and many communities in the District experience the negative effects associated with this inadequacy. This scenario has greatly led to the deterioration of sanitation and hygiene services leading to poor health and physical devastation. As Van Wijk-Sijbesma (1998) asserts, participation of women in health interventions in water scarce areas can bring distinct 78 benefits to water sanitation and hygiene as a whole. Therefore, in an effort to improve health status in a more sustainable way in this study a number of interventions were designed and evaluated targeting women. In this study, majority of the respondents were middle aged mothers of between 26 to 35 years (36.3%) and the highest proportion of them had primary school level education (43%). For this study, various gains were recorded between the baseline (2007) and postintervention (2008). Amongst the gains were that baseline findings established that majority of the respondents disposed their children’s waste in the open, but that changed significantly after the intervention. Specifically, latrine coverage by type changed significantly, with the number of traditional pit latrine household ownership increasing from 45.5% to 63.6% as opposed to ventilated improved pit latrine household ownership that fell from 54.5% to 36.4% (χ²=4.43, P=0.035). In a similar study undertaken to determine whether a large 3-year hygiene promotion programme in Bobo-Dioulasso, Burkina Faso was effective in changing behaviours associated with the spread of diarrhoeal diseases, some notable gains included safe disposal of children’s stools, that increased from 80% at pre-intervention (1995) to 84% post (1998). There was reduced prevalence of diarrhoea and improved general health status of children aged less than five years. 79 The observed health gains are associated with differences in community involvement and the participatory approach adopted. The Turkana study interventional approach involved Participatory Hygiene and Sanitation Transformation (PHAST) that integrated the principles of Community Led Total Sanitation (CLTS). CLTS basically trigger communities into demanding hygiene and sanitation facilities. The key challenge in implementation of effective sanitation and hygiene is the up-scaling in the local communities and domesticating the tools to suit the local conditions. As reported by Kamal Kar (2003), in India, use of PHAST is highly effective when integrated with CLTS programs that seek to create a sense of disgust and shame against open excreta disposal. However, there are many challenges in implementation of effective sanitation and hygiene interventions especially up-scaling it in local communities and domesticating the tools to suit local conditions in resource poor areas. This study had similar challenges in that there were varying socio-economic strata of the beneficiary community. Specifically, there are several socioeconomic and cultural cross cutting factors which affect the availability and the type of the toilets within the households. Lack of money to purchase the hardware was the main reason for not having a toilet. Responsive approaches allow communities in different socio-economic groups to express their social, economic and environmental demands; though incentives to sanitation, hygiene, value and honour should be viewed in commensurate to the community’s development status. 80 In the developing world today, diarrheal diseases are amongst the leading causes of child mortality and it has been shown that the simple act of washing hands with soap can decrease diarrhea risk by almost half. A study on hand washing practice conducted in Korea noted that out of the 942 students who participated there was a 30.3% increase in hand washing an improvement of one carried out one year earlier. (Jae-Hyun Park et al., 2010). In Turkana, targeted interventions recorded significant gains in the habit of hand washing practice. In Lodwar Central, those who wash hands regularly increased from 85.5% to 89.9% (χ²=10.85, P=0.028). In Lokichogio Division, the proportions increased from 77.5% to 93.8% (χ²=15.56, P=0.004) whereas in Kakuma Division, hand washing practice increased from 48.8% to 91.3% (χ²=7.28, P=0.122). These results show that targeted interventions aimed at increasing hand washing practice should be encouraged across all communities irrespective of their socio-economic strata. In addition, presence of soap in households changed between 2007 and 2008 with that of those with no education increasing from 65.4% to 77.9% (χ²=3.87, P=0.049). These finding are comparable to those of the Bobo-Dioulasso, Burkina Faso study that noted presence of soap increased hand-washing with soap during critical times such as after cleaning a child’s bottom, which rose from 13% to 31% (Sidibe and Curtis, 2002). Similarly, the proportion of mothers who washed their hands with soap after using the latrine increased from 1% to 17%. However, it is also notable that both the Burkina Faso study and Turkana study checked on hand-washing during critical times including before eating any meal. 81 The promotion of hygienic behaviour especially hand washing has been identified as a public health intervention likely to have considerable impact in the reduction of diarrhoeal diseases in young children in developing Countries (McLennan, 2000). While washing hands at critical times is accepted as an effective intervention against diarrhoeal disease, evidence is also now growing for its effectiveness against respiratory infections (Cairncross, 2003). Based on the results of the Turkana study, up-scaling of hand washing with soap practice is highly recommended, especially using the germ theory to promote healthy behaviour. This study reveals that hand washing practice increased exponentially with age. Significant improvements was observed in the age group between 36 and 45 years of age with increase from 66.7% in 2007 to 88.9% in 2008 ((χ²=10.01, P=0.04). This observation had protective effect especially among the child bearing group for their own hygiene and that of their small children. These results compares well with other studies by the World Bank, Water and Sanitation programme in Cambodia which have shown that health improvement can be easily registered in resource constraint communities by applying different approaches and solutions (WSP, 2002). Although the results of the post intervention measures showed that there was increase in hand washing, sustainability of the activities is unpredictable in the event of prolonged drought leading to inadequate water. 82 5.1.2 Changing community health outcome measures The effectiveness of interventions like the ones noted above is usually measured by changes in behaviours, on the assumption that change in behaviour will usually be reflected in reduced morbidity and mortality (Curtis, 2003). The question of whether health education and hygiene promotion actually leads to reduction in disease burden in the community has always elicited mixed results. A paper on the experience of Bawku West District in Ghana noted that despite many efforts by both government and nongovernmental organizations in providing water and sanitation infrastructure, health education and hygiene promotion, little had been achieved in reduction of water and sanitation related diseases or improvement in hygiene behaviours. Mixed results noted in the approach above is first to establish whether there was any significant change in community related behavioural variables as well as health outcomes after the intervention. Contrary to the above observations, the Turkana study demonstrated significant changes in behaviour related variables including decrease in faecal coliform count in drinking water, and diarrhoea related microbes in children stool as biological proxy indicators of community health outcomes. Chlorine levels measured to control for possible confounding effects did not have significant differences before and after intervention. The differences between the Turkana study and that of Ghana may have arisen from the approaches employed. It may also be attributed to varying pre-existing levels of hygiene in the two districts besides differences in cultural and socio-economic 83 status. Community behaviour change is a function of many and complex variable combination and it is also possible that the two areas were totally different in many aspects. In the study, the mean chlorine level was found to be the same in 2007 and 2008 (no significant difference) whereas mean faecal coliforms per 100ml drinking water sample varied significantly between 2007 and 2008. In Kakuma, mean faecal coliform count reduced significantly from 88 to 30.2 units (P=0.005), while in Lodwar Central, the coliform count reduced significantly from 91 to 17.3 units (P=0.003), and in Lokichogio Division, the coliform count reduced significantly from 63.8 to 23.6 units (P=0.006). For diarrhoeal related microbes in children stool, this study established that there was a reduction from 91.3% in 2007 to 78.3% after intervention. However, this study did not find any previous related publications measuring drinking water faecal coliform count nor diarrhoea related microbes in children stool before and after intervention in the same population hence difficulties in providing direct comparative findings. 84 5.1.3 Effectiveness of hygiene and sanitation interventions in changing mother’s hygiene behaviour and improving child health Although hygiene promotion is a tenet of many health programmes, doubts remain about its effectiveness. A previous review of over 500 articles on health education in developing countries that were published in 1987 found only three with satisfactory evidence of behaviour change or an impact on health. According to this study, the reduction noted above in coliform count resulted from improvements in mother’s behaviour and was strongly associated with an R-square of 39.6%. The three key influencing variables included; age of the mother (P=0.015), presence of latrine (P=0.038), and reasons given at baseline for not having latrine (P=0.005). This means that the three identified variables explain about 40% of the observed relationships between coliform count and mother’s behaviour. This shows that any hygiene and sanitation promotion intervention should target women of mid-age parenthood between 26 to 35 years and should include all possible means to increase latrine ownership as well as change community perception on latrine ownership amongst other interventions since these factors contributes about 40% of faecal contamination of drinking water. On the other hand, this study also established with high certainty (positive predictive value of 92.7%, P<0.0001) that certain mother’s behavioural risk factors are key predictors of presence or absence of diarrhoea related microbes in children aged less than five years. 85 They are namely; mothers education level (P=0.033), toilet presence (P=0.022), distance to latrine (P=0.004), source of drinking water (P=0.019), treatment of drinking water (P=0.013) and drinking water storage (P=0.067). As previously noted, there are no comparative studies to date. Ultimately, diarrhoea prevalence in children aged less than five years was found to be highly linked to mother’s behavioural characteristics; namely, 1. If the child had diarrhoea at baseline (2007), it was highly likely that the same child would have diarrhoea at end line (after one year of intervention); 2. Mother’s education, a factor that was not expected to change over the period of intervention; 3. Latrine availability and latrine structure which were core areas of intervention, hence shows that there was marked differences between those who had a latrine facility as compared to those who did not have the facility; 4. Chlorine level, indicating that though the chlorine levels did not change significantly between baseline and end line, there was protective effect against child diarrhoea for those who used chlorinated water. The above four variables are hence core modifiable factors in any hygiene and sanitation promotion project. 86 5.2 Conclusions This study found that most mothers in Turkana District were within 26 and 35 years age bracket and belonged to low socio-economic and education levels. This is a common phenomenon in many other communities and therefore the study results are likely to apply beyond Turkana District. Sanitation and hygiene promotion based on the approach of PHAST was highly effective in changing sanitation and hygiene behaviour and practices of mothers when integrated to Community Led Total Sanitation (CLTS) programs that seek to create a sense of disgust and shame against open excreta disposal. The specific gains included increased latrine coverage by type, that changed significantly with the number of traditional pit latrine household ownership increasing by 18.1%, change in hand washing practice achieved a high of 42.5% in Kakuma Division with an overall 22% increase within the age group 36 to 45 years, presence of soap in households increased by 12.5% within the group who had no education. There was overall significant improvement in community health outcomes before and after the intervention with comparative reduction in faecal coliform count in drinking water ranging from 40.2% to 73.7%. Similarly, diarrhoea related microbes in children stool reduced by 13%. Hygiene and sanitation interventions were found to improve in changing mother’s hygiene behaviour and improving child health by reducing faecal coliform count by 87 about 40% with age of the mother, presence of latrine and reasons given at baseline for not having latrine being the key determinants. On the other hand, diarrhoea related microbes presence or absence could be predicted with an overall 92.7% (97% for the diarrhoeal related samples and 73% for those with no microbes correctly identified by modeling) precision using core determinants/predictors as mothers education level, toilet presence, distance to latrine (P=0.004), source of drinking water, treatment of drinking water and drinking water storage container. The results of the study confirms the first hypothesis that Sanitation and hygiene interventions have no effect in changing mother’s knowledge in sanitation and hygiene before and after the intervention (p=0. 476). The second hypothesis has been rejected after the results showed significant changes in handing washing practice Lokichogio p=0.004 and Central Lodwar p= 0.028. The third hypothesis has also been rejected as Sanitation and hygiene interventions was seen to have effect in changing faecal coliform count in drinking water at the point of use before and after the intervention with a p value of < 0.0005. The fifth and sixth hypothesis were also rejected based on the fact that their was reduction in diarrhoeal among children less than five years before and after the intervention Ultimately, it was strongly established that any hygiene and sanitation promotion project should consider diarrhoea at baseline, mother’s education, latrine availability and structure and use of chlorine as the core predictors and modifiable factors against childhood diarrhoea. 88 5.3 Recommendations 1. Skills training and enhancement at the household level within the community – The study found that the community comprises of individuals of low socio-economic status and it would be appropriate to enhance their skills in human excreta disposal and household water treatment. Post intervention measures showed general improvement on excreta management and this should be scaled up or replicated in other communities. 1 Interventions aimed at improving sanitation and hygiene in communities should always include targeted behaviour change interventions -Adopt and upscale community based participatory approaches as used in this study to overcome sanitation and hygiene barriers in resource constrained communities by application of relevant participatory approaches such as CLTS and PHAST. 2 Multiple targeted interventions focused to resolve the barriers to sanitation and hygiene should be implemented - Based on whatever barriers defined by different communities, multiple high impact interventions applied in this study including hand washing with soap, household water treatment and safe storage and improved human waste disposal facilities should be implemented complimentarily. This ensures needs based approach to curbing sanitation and hygiene problems within the communities. 3 Additional targeted research - Based on findings of this study and related previous publications, it is important to undertake a focused research on the 89 economies of scale between application and effectiveness of ‘point of use’ water treatment as compared to public interventions applied in this study, as well as their combined benefits. There is also a need to carry out a more focused knowledge, attitude and practice study which could not be well covered in this research. 90 REFERENCES Ahmed, F., Clemens, J. D., Rao M. R., and Banik, A. K. (1994) Family latrines and paediatric shigellosis in rural Bangladesh: benefit or risk? Int. J.Epidemiol. 23 (4):856-862, 1994. Aiello, A.E and Larson, E.L. (2002) What is the evidence for a causal link between hygiene and infections? The Lancet Infectious Diseases, 2 (2), 103-110. Astier, M., Almedom, Ursula, B. and Lenore, M. (1997) Hygiene Evaluation Procedures: Approaches and methods for Assessing Water and Sanitation-related hygiene practices. International library of for developing Countries, London, United Kingdom. Aziz, K. M. A., Bilqis A., Hoque, K,H., Hasan,Z., Patwary, M. Y., Sharon R. A., Huttly, M., Mujibur, R. and Feachem, R. G. (1990) Reduction in diarrhoeal diseases in children in rural Bangladesh by environmental and behavioural modifications:.Transactions of the Royal Society of Tropical Medicine and Hygiene, 84 (3) 433-438. Bajracharya, D (2003) Myanmar experiences in sanitation and hygiene promotion: lessons learned and future directions. International Journal of Environmental Health Research, 13:141-152. Bern, C., Martines, J.C., de Zoyasa, I. And Glass, R.I. (1992) The magnitude of the global problem of diarrhoeal disease: a ten-year update. Bulletin of the World Health Organisation, 70, 495-509. Brenner, K.P., Rankin, C.C., Roybal,Y.R., Stelma, G.N., Scarpino, P.V.Jr. and Dufour, A.P.(1993) New Medium for the Simultaneous Detection of Total Coliforms and Escherichia coli in Water. Applied and Environmental Microbiology 59: 3534-3544. Environmental Monitoring systems Laboratory, U.S. Environmental Protection Agency, Cincinnati, OHIO 91 Bordner, R., Winter, J. and Scarpino, P. (ed). (1978) Microbiological Methods for Monitoring the Environment: Water and Wastes. EPA-600/8-78-017, Environmental Monitoring Systems Laboratory, U.S. Environmental Protection Agency, Cincinnati, OHIO Bhutta, Z.A., Tahmeed, A., Black, R.E., Cousens, S. Dewey, K., Giugliani, E., Batool, A,. Haider, Kirkwood, B., Morris, S.S., Sachdev, H.P.S., and Meera Shekar,M.(2008) Maternal and Child Undernutrition Study Group (2008): What works Interventions for maternal and child under nutrition and survival, The Lancet Volume 371, Issue 9610, February 2008, Pages 417-440. Black, R.E. and Lanata, C.F. (1995) Epidemiology of diarrhoeal diseases in developing countries. New York, NY: Raven Press, Ltd, 13–36. Black, M. and Fawcett, B. (2008) The last taboo: Opening the door on the global crisis. Earth scan Pub.Lodon.Uk Bowen, A., Huilai, M., Jianming, O., Ward Billhimer, W. Long, E., Mintz, R. Hoekstra, M., and Luby, S. (2007) A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Journal of Tropical Medicine and Hygiene, 76(6), 2007, pp. 1166–1173 Cairncross S. (1990) Health impacts in developing countries: new evidence and new prospects. Water and Environmental Journal, 1990; 4:571–7. (5) Central Bureau of Statistics (2004) Ministry of Planning and National Development and UNICEF, Kenya, multiple indicator cluster survey (MICS) report.Nairobi, Kenya: Central Bureau of Statistics. Central Bureau of Statistics (2003) Ministry of Planning and National Development and UNICEF. (2003) Kenya, multiple indicator cluster survey (MICS) report. Nairobi: Kenya. Central Bureau of Statistics. 92 Cheesbbroug, M. (2000) District Laboratory Practice in Tropical Countries Part 2. UK: Cambridge University Press. Clasen, T., Roberts, I., Rabie T, Schmidt W-P, Cairncross, S. (2006). Interventions to improve water quality for preventing diarrhoea, Issue 3 (Cochrane Review).Oxford: The Cochrane Library. Cumming, O. (2008) Tackling the silent killer: The case for sanitation. London, UK: Water Aid. Curtis, V. (2003) Talking dirty: how to save a million lives. International Journal of Environmental Health Research 13: 73-79. Curtis, V. and Cairncross, S. (2003) Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infectious Disease 3: 275-281. Department for International Development (1998) Guidance manual on water supply and sanitation programmes. London: WELL and London School of Hygiene and Tropical Medicine for DFID. Ezeamama, A.E., Friedman J.F., Acosta L.P., Bellinger D.C., Langdon G.C., Manalo D.L., Olveda R.M., Kurtis J.D., and Stephen T. Mcgarvey S.T.,(2005) Helminth infection and cognitive impairment among Filipino children: American Journal of Tropical Medicine and hygiene 72(5), 2005, pp. 540-548 Ezzati, M., Vander Hoorn, S., Rodgers, A., Lopez, A. D, Mathers, C. D. and Murray, C. J. L.(2003) Comparative Risk assessment Collaborating Group: Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet, Vol. 362, pp. 271–80 93 Fewtrell, L., Kaufmann, R.B., Kay, D. Enanoria, W., Haller, L., and MColford Jr, J. (2005) Review. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis 2005, 5: 42–52. Gilman, R. H., Marquis, G.S., Ventura G. and Campos, M. (1993) Water cost and availability: Key determinants of family hygiene in a Peruvian Shanty Town. American Journal of Public Health 83: 1554-1558. Government of Kenya. Ministry of Finance and Planning (2001) Turkana District Development Plan. 2002-2008. Nairobi. Government of Kenya. Ministry of Health (2005) Weekly epidemiological bulletin. Nairobi: Ministry of Health headquarters. Government of Kenya. Ministry of Health (2006) Weekly epidemiological bulletin. Nairobi: Ministry of Health headquarters. Government of Kenya. Ministry of Health (2007) National Environmental Sanitation and hygiene Policy. Nairobi: Ministry of Health Head quarters. Gracey Michael. (1983) Diarrhoea diseases and Malnutrition. BMJ. Green, L. W. (1992) "Prevention and Health Education." In Maxcy-Rosnau-Last: Public Health and Preventive Medicine, 13th edition, eds. J. M. Last and R. B. Wallace. Norwalk, CT: Appleton & Lange. Gunther, I., Fink, G. Water, Sanitation and Children’s Health: evidence from 172 DHS Surveys (2010): Policy Research Working Paper 5275: The World Bank Development Economics Prospects Group. Harvason, S.J. (2004) Women’s management of the household health environment: Responding to childhood diarrhoea in the Northern Areas, Pakistan: Health Place 10: 43-58. 94 Harvey, P.A and Reed, R.A. (2004). Planning environmental sanitation in programs in emergencies, Water Engineering and development center, UK: Lough bourough University. Heller, L., Colosimo, E.A., Antunes, C.M (2003). Environmental Sanitation Conditions and Health Impact: a case-control study. Rev Soc Bras Med Trop., 36: 41-50 Hoque, B.A., D. Mahalanabis, M.J. Alam and Islam, M.S. (1995). “Post-Defecation Hand washing in Bangladesh: Practice and Efficiency Perspectives.” Public Health 109:15–24. International Water and Research Centre (IRC) and Water Engineering Development Centre (WEDC). (2002). Sanitation Connection Theme: Health and Social. Available internet: www/helpdesk@sanicon.net/ud.html (Accessed 10 June 2010) Jae-Hyun Park, Hae-Kwan Cheong, Dae-Yong Son,Seon-Ung Kim,Chang-Min Ha(2010) Perceptions and behaviours related to hand hygiene for the prevention of H1N1 influenza transmission among Korean university students during the peak pandemic period. BMC Infectious Diseases 2010: 10:222 Kaltenthaler, E.C. and Pinfold, J.V. (1995) Microbiological methods for assessing hand washing practice in hygiene behaviour studies. Journal of tropical medicine and hygiene. 98: 101–6 Kamal Kar. (2005) Practical Guide to Triggering Community-Led Total Sanitation. Brighton, UK: Institute for Development Studies (IDS). Kenya National Bureau of Statistics (2009 Population and Housing Census 2009, Nairobi: Government Printer. Kosek M., Bern C., and Guerrant, R.L. (2003) The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bull World Health Organisation; 81:197–204. 95 Lammerink, M. (1998) Community managed rural water supply: experiences from participatory action research in Kenya, Cameroon, Nepal, Pakistan, Guatemala and Colombia. Community Development Journal, 33(4):342–352 Lemeshow, S. et al. (1990) Adequacy of sample size in health studies. New York: John Wiley & Sons. Lopez, A.D., Mathers, C.D., Ezzati, M., Jamison, D.T., Murray, C.J. (2001) Global and Regional Burden of Disease and Risk Factors, Systematic analysis of population health data. Lancet 2006, 367:1747–57. Luby, S.P., Agboatwalla, M., Feikin, D.R. et al. (2005) Effect of handwashing on child health: a randomised controlled trial. Lancet, 366:225–33. Luby, S.P., Agboatwalla, M., Billhimer, W. and Hoekstra, R.M. (2007) “Field Trial of a Low Cost Method to Evaluate Hand Cleanliness.” Tropical Medicine & International Health, 12:765–71. McLennan, J.D. (2000) Prevention of diarrhoea in a poor District of Santo Domingo, Dominican Republic: practices, knowledge, and barriers. Tropical Medicine & International Health, 5(1): 22-32. Mertens, T. E., Jaffar, S., Fernando, M. A., Cousens, S. N. and Feachem, R. G. (1992) Excreta disposal behaviour and latrine ownership in relation to the risk of childhood diarrhoea in Sri Lanka. International Journal of Epidemiology, 21 (6):1157-1164, 1992. Murray, C.J., Lopez, A.D., Mathers, C.D. and Stein, C. (2001) The Global Burden of Disease 2000 Project: Aims, Methods and Data Sources, Global Programme on Evidence for Health Policy. Discussion paper No. 36. Geneva: World Health Organisation 96 Murray, C. J. L., Lopez, A. D. and Jammison, D. T. (1994) The global burden of disease in 1990: summary results, sensitivity analysis and future directions. Bulletin of the World Health Organization, 72:495–509 Murray, C.J., Lopez, A.D., and Jammison, D.T. (1994). The global burden of diseases in 1990: Summary of results, sensitivity analysis and future directions. Bulletin of the World Health Organization, Geneva. Narathius Asingwire. (1994). Health related behaviours in Bukalimo village and in Mpande/Nakazinga village; RUWASA project. Report available online at http://www.watsanuganda.watsan.net/page/420, accessed on 12th February, 2011. Nunoo, D., Mumuni, O.K., and Awuku, N. N (2009) Ghana. Participatory Hygiene and Sanitation Transformation (PHAST): A Methodology for Sustainable Hygiene and Sanitation Behaviour Change with Experience from The Bawku West District of Ghana Organization for Economic Co-operation and Development /African Development Bank (OECD and ADB) (2004) African Economic Outlook: 2003/04 Prüss Üstün, A., Kay, D., Fewtrell, L., Bartram, J. (2002) Estimating the burden of disease from water, sanitation and hygiene at a global level. Environmental Health Perspectives, 110(5): 537–542. Prüss-Üstün,A. ,Bos, R., Gore,F., Bartram, J. (2008) Safer water – better health. Costs, benefits and sustainability of interventions to protect and promote health. Geneva, Switzerland: World Health Organization. Quareshi, A.F, and Lobo, M.A. (1994) Socio- anthropological determinants and home management in childhood diarrhoea in a squatter settlement of Karachi, Pakistani. Journal of Tropical Pediatrics, vol.40, December 1994: pages 378-380. 97 Rabie, T. and Curtis, V. (2006) Hand washing and risk of respiratory infections: a quantitative systematic review. Tropical and International Health journal 3: 258-267. Rhee, V. Luke, C. M., Subarna, K. K., Joanne, K. Steven, C. L., Gary, L. D. and James M. T. (2008) Maternal and Birth Attendant.Hand Washing and Neonatal Mortality in Southern Nepal Arch Pediatr AdolescMed. 162(7): 603-608. Sanitation.pdf – Accessed March 2010 Sharon, R. A., Huttly, D. B., Betty, R. K., Robert, N. E. and Feachem, R.G. (1987) The epidemiology of acute diarrhoea in a rural community in Imo State, Nigeria.Transactions of the Royal Society of Tropical Medicine and Hygiene, 81, ( 5): 865-870 Shordt, K. and Caincross, S. (2004) Sustainability of hygiene behaviour and the effectiveness of change interventions: Findings and implications for water and sanitation programmmes from a multi – Country research study. Delft, the Netherlands: IRC international water and sanitation centre. Sidibe, M. and Curtis, V. (2002) Water and Sanitation Programme Hygiene Promotion in Burkina Faso and Zimbabwe: New approaches to behaviour change, WSP Field Note 7, August 2002 Smith, K.R., Corvala´n, C.F., Kjellstrom, T. (1999) How much global ill health is attributable to environmental factors? Epidemiology 10:573–84 United Nations Educational, Scientific and Cultural Organisation (2003) UN World Water Development Report: water for people, water for life. Paris, New York, and Oxford: UNESCO and Berghahn Books. 98 United Nations Human Settlement programme (2003) Water and sanitation in the world’s cities, Local action for Global Goals, Nairobi, Kenya: United Nations Human settlement program. United Nations Children Fund, (2007). Progress for children: a world fit for children statistical review, MDG 4: reduce child motality, NewYork 6:18-24 Ustun, A.P. and Corvalan, C. (2006) Preventing Disease through health Environments: Towards an estimate of the environmental burden of disease. Geneva, Switzerland: World Health Organization, Van Wijk-Sijbesma, C. (1998) ‘Gender in Water Resources Management, Water Supply and Sanitation - Roles and Realities Revisited’. The Hague, Netherlands: International Water and Sanitation Centre. Waddington, H., Snilstveit, B., WhiteH. and Fewtrell L. (2009) Water, sanitation and hygiene interventions to combat childhood diarrhoea in developing countries: International initiative for Impact Evaluation(3IE), Synthetic Review 001, Sudan:World Bank. Water and Sanitation Programme (2006) Getting Africa on track to meet the MDGs on water and sanitation: Status overview, Nairobi, Kenya Water and Sanitation Programme (2002) Learning what works for Sanitation: revisiting sanitation success in Cambodia, Water and Sanitation Programme in the Pacific (WSP-EAP), Cambodia./LU%y3rt Water Supply and Sanitation Collaborative Council and World Health Organisation (2005) Sanitation and Hygiene Programme Guidance. WHO, Geneve Switzerland. World Health Organization and UNICEF (2010). Progress on sanitation and drinking water:2010 update. Geneva, Switzerland. 99 WleChevellier, M. and Kwok-Keung, A., (2004) Water treatment and pathogen control: Process efficiency in achieving safe drinking –water. London, UK: WHO, IWA Publishing, World Health Organization (2004) Water, sanitation and hygiene links to health: facts and figures. http://www.who.int/water_sanitation_health/publications/factsfigures04/en/. (Accessed Nov 12, 2011) World Health Organization (2006) Guidelines for drinking water quality. Third edition, volume 1: Recommendations, Geneva: World Health Organization. World Health Organization (2007) Combating water borne diseases at house hold Level, The international network to promote household water Treatment and safe storage. Geneva, Switzerland: World Health Organization. World Health Organization (2004) The Global Burden of Disease: 2004 update. Geneva: World Health Organization. World Health Organization (2003) Shaping the Future. Geneva: World Health Organization. World Health Organization/UNICEF (2008) Report of the WHO/UNICEF Joint Monitoring Programme on water Supply and Sanitation. New York, Geneva: United Nations Children’s Fund and the World Health Organization World Health Organization/United Nations Children's Fund Joint Monitoring Programme on Water Supply and Sanitation (2008) Progress on Drinking Water and Sanitation: special focus on sanitation. New York: UNICEF and Geneva: WHO. World Health Organization/United Nations Children's Fund Joint Monitoring Programme on Water Supply and Sanitation (2008) A snapshot of sanitation and in Africa: A special tabulation for AfricaSan based on preliminary data from WHO/UNICEF Joint Monitoring Programme on Water Supply and Sanitation. New York, USA 100 Wright, J. Gundry, S. and Conroy, R. (2004) Household drinking water in developing countries: a systematic review of microbiological contamination between source and point-ofuse. Tropical Medicine and International Health. volume 9 no 1: pp 106–117 January 2004 Zaltman, J. (2003) How customers think. Essential highlights into the mind of the market.Havard business school press. 101 APPENDICES APPENDIX 1: HOUSEHOLD QUESTIONNAIRE A . GENERAL INFORMATION. District: __________________________Division____________________________________ Location: ________________________ Sub location: ____________________________ __ Village___________________________Household Head Name ________________________ Cluster No___________________________________________________________________ Date of interview (dd/mm/yyyy)__________________________________________________ Time of interview______________________________________________________________ Name of interviewer___________________________________________________________ Ask to speak to the head of the housed hold, if unavailable ask to speak to the mother of the under Five or guardian or caretaker. Introduce your self and purpose of the study . 102 B.HOUSEHOLD BACKGROUND INFORMATION 1.Household head Sex (DO NOT ASK, CIRCLE CORRECT RESPONSE) 1 Male 2.Female 2.How old are you? ( TICK THE CORRECT RANGE FROM THE TABLE BELOW) Age of Household Head Member Age group 14 – 25 26 – 35 36 – 45 Over 46 yrs Male Female REQUEST TO SPEAK TO THE MOTHER OF THE UNDER FIVE IF SHE IS NOT THE HOUSEHOLD HEAD OR THE CARE TAKER/GUARDIAN 3 How old are you? (TICK THE CORRECT AGE RANGE FROM THE TABLE BELOW) Age of mother of the under five, Guardian or care taker Age group 14 – 25 26 – 35 36 – 45 Over 46 yrs Male Female 4.Marital Status Household head Mother Married Single Separated Widowed Divorced 103 Guardian/Caretaker N/A 5.How many people live in this household? (The definition of household is people eating from the same kitchen/pot) _____________________________________ 6.Their Sex and Ages in years of Household members Age group Under 5yrs 5 – 10 11 – 14 15 – 25 > 25 yrs Male Female 7.Highest level of education. Complete the following after probing the responded on education status Household head Mother Under five No education Some Primary Finished Primary Some secondary Finished secondary Some tertiary Completed Cert., Diploma, higher Diploma etc 8.Occupation: 1. Business 3. Farming 5. Fishing 2. Salaried employment 4. Patrolism 6. Other (specify)________________ 9.Tick type of house structures. 1 Permanent House 2 Grass thatched house 104 of Care Taker/ Guardian 3 Semi-Permanent House 4 Manyatta C. SANITATION Now I am going to ask a few questions about sanitation and personal hygiene 10.Do you have a toilet facility in this compound? If Yes > Go to No.14 If No- proceed to no.11 11.Why is there no toilet in this compound? 1.Can’t afford it 2.Soil too loose/Rocky 3.Do not need one 4.Collapsed and full 5.Other (specify)__________________ 12.Where do you go to make a long call (defecate) if you don’t have a latrine at home? 1 2 3 4 5 6. 7. On compound grounds somewhere Behind the house Friend’s house Public latrine Neighbour’s house Bush/field Others (specify)____________________________ 13.Where do you make a short call (Urinate) if you not have a latrine at home? 1 On compound grounds somewhere 2 Behind the house 3 Friend’s house 4 Public latrine 5 Neighbour’s house 6 Bush/field 105 7 Other (specify)____________________________ 14.How many latrines in this compound are currently functioning? (If more than one facility is functioning in the compound address all functioning latrines) 15.Do you share this/these latrine(s) with other household(s)? 1.Yes 2.No 16.How many other households use this/these toilet(s)? ___________Households 17.Approximately how many individuals regularly use this/these toilets?____________ 18.Is there any one in this household, including children, who does not regularly use the latrine? 1.Yes 2.No 19.Who doesn’t regularly use the latrine? 1. Children<2 years 2.Children < 5years 3.Children 5-15 years 4.Female adults 5.Male adults 6.No one uses the latrine 7.Other (specify)_________ 20.Why do these people not use the latrine? (May have to change the answers based on who’s in---) 106 1. 2. 3. 4. 5. 6. 7. Children too small Not at home Not well kept Distance from the compound Fear, dislike Beliefs: customs/ taboos Other (specify)_________________ 21.How do you dispose off the faeces of your child/children under 5 years? 1. Leave it in the yard and do nothing 2. Put in the latrine 3. Bury it 4. Don’t know 5. Other (specify)_________________ 23.How often do you clean your toilet? 1. Once a day 2. Once a week 3. Once a forty night 4. When it is dirty 5. Do not clean at all 24. a) Do you have a refuse pit? 1. Yes 2. No b) If No, where do you dispose your refuse? 1. Open land 2 Toilet 3. Burning D.OBSERVATIONS ON SANITATION 25.Is there evidence of faecal contamination within the compound? 1.Yes 2. No 107 26.a) Can you show me please the type of latrine that you are using? No. of functioning latrines observed around the compound ____________ b) Type of toilet facility in compound. If more than one, determine the newest Flush toilet) 1. Traditional Pit latrine 2. Ventilated Improved Pit Latrine 3. No facility/ bush/field 4. Other (specify)_________________________________ 27.How far is the latrine from the dwelling house? 1. Less than 10 m 2. 10-20 m 3. More than 20 m 28.Conditions of latrine a) Contains concrete slab. 1 Slab present. 2 Slab absent b). Smell 1 No smell 2 smell inside 3 Smell outside latrine c). Cleanliness 1 clean 2 slightly dirty 3 Presence of faeces d). Flies 1 No flies 2 a few flies 3 many flies e). Superstructure 1 No cracks 2 Crack s 3 Visible holes f). Condition of slab 1 No cracks 2 Cracks g). Door 1 door closes completely 3 Pit visible 2 Closes but not completely 3 No door. 8. Others (specify)___________________________________ 30. a) Do you know importance of using a latrine? 1. Yes 2. No b) If yes what are the importance? 1. Privacy 2. Status 3. Prevention of disease 4. Do not know 108 5. Other (specify)________________________________________________ 31.a) Do you know diseases related to using latrine? 1. Yes 2. No b). If yes, name them; 1.Typhoid 5.Malaria 2. Cholera 6.URTI 3. Hook worms 7. HIV/AIDs 4.Diarrhoea 8.other (specify)____________________________________ c) How can we prevent these diseases mentioned above ? 1.use of pit latrine 7.Cover food. 2.wash babies 8.Go to hospital 3.Treat water 9.Traditional healer 4.eat well 10.prayer 5.wash hands 11.other (specify)__________________ E.WATER SOURCES HANDLING, STORAGE AND TREATMENT I am now going to ask you a few questions about your water source and handling practices 32.What sources of water does your family use for cooking, washing, bathing or cleaning throughout the year? (Do not include sources used only for agriculture or animals) (Multiple responses possible) Piped into dwelling Piped into school Public tap (outside school) Open well in compound Open public well Covered well/borehole in compound Covered public well/Borehole Spring – Protected Spring – unprotected River Stream 109 11 12 13 21 22 31 32 33 41 42 Lake Pond/Dam/Earth pan Rainwater/Roof catchments Water Vendor Bottle water No water available Don’t know 43 44 51 61 71 98 99 33.What source of drinking water do you use most frequently during the rainy season? (Choose one) Piped into dwelling Piped into school Public tap (Outside school) Open well in compound Open public well Covered well/Borehole in compound Covered Public well/Borehole Spring – protected Spring – unprotected River/Stream Lake Pond/dam/Earth pan Rainwater/roof catchment Water vendor Bottled water No Water Available Don’t know 11 12 13 21 22 31 32 33 41 42 43 44 51 61 71 98 99 34.Approximately, how long does it take you to get the water from this source and come back? (Do not read. If range, write the middle of range) On premises 110 ____ Minutes ____ Hours (convert to minutes) 35.How much water do members of your family collect/take from this source daily? _____ Litres 36.Approximately how many litres of water does your family use for drinking daily during the rainy season? _____ Litres 37.Is the water you collect from this source sufficient for drinking needs of your family: 1.Always 2.Sometimes 3.Never 38.How frequently is water available from this source during the rainy season? 1.Always available 2.Several Hours per day 3.Once or twice per week 4.Infrequently 39.What did you use this water for? 1.Drinking only 2.Bathing/Hygiene/hand washing/ 3.Washing clothes/cleaning compound 4.Animals/Agriculture 5.Cooking. 6.Other (specify)________________________________________________ 40.Do you have to pay for this source? _____Ksh per ______ Litres (convert to Ksh/Litre) (If answer “jerry can”, determine size) 111 41.What source of drinking water do you use most frequently during the dry season? (choose one) Piped into dwelling Piped into school Public tap (outside school) Open well in compound Open public well Covered well/borehole in compound Covered public well/Borehole Spring – Protected Spring – unprotected River Stream Lake Pond/Dam/Earth pan Rainwater/Roof catchment Water Vendor Bottle water No water available Don’t know 11 12 13 21 22 31 32 33 41 42 43 44 51 61 71 98 99 42.Approximately, how long does it take you to get the water from this source and come back? 1.On premises 2. _____________ Minutes 3. _____________ Hours (convert to minutes) 43.How much water do members of your family collect/take from this source daily? _____________ Litres 44.Is the water you collect from this source sufficient for drinking needs of your family? 1.Always 2.Some time 3.Never 45.How frequently is water available from this source during the dry season? 1.Always available 2.Several Hours per day 3.Once or twice per week 112 4.Infrequently 46.What did you use this water for? 1.Drinking only 2.Bathing/Hygiene/hand washing/ 3.Washing clothes/cleaning compound 4.Animals/Agriculture 5.Others (specify)___________________ 47.Do you have to pay for this source? 1.Yes 2.No 48. How much do you have to pay? _____KSH per ______ Litres (convert to KSH/Litre) (If answer “jerry can”, determine size) 49.Do you consider water from the current source safe for drinking? 1.Yes 1 2.No 2 3.Don’t Know 99 50.a) Do you treat your water to make it safe for drinking? 1.Yes 1 2.No 2 3.Don’t Know 99 b) If yes how do you treat your water? 1.Boiling water 2.Use of household filters 3.Use of waterguard 4.Treating water with PUR 5.Traditional herbs 6.Three pot system 7.SODIS 8.Chlorine based tablets Others(specify)_________ F.HAND WASHING PRACTICES 51. a) Do you often wash your hands? 1.Yes 2.No 113 9. 3.Not Always. b) When do you wash your hands? (Multiple responses possible) 1.Never 2.After visiting latrine/Toilet. 3.Before preparing food 4.Before feeding baby 5.Before eating meal. 6.Every time when I touch something dirty 7Others (Specify)________________________ 52.Can you please show me how you wash your hands? 1.Yes 2.No 3.No water available for hand washing 53. (a) Does the respondent pose the right skills for washing hands? (Observe) (Tick the steps below. if the respondent follows all steps then mark yes if not then mark No) 1.Yes 2.No. 1. Wets hands 2. Lathers with soap 3. Rubs hands, wrists, palms and in between fingers 4. Rubs for at least 10 seconds 5. Cleans dirt under finger nails 6. Air dries hands or uses a clean cloth 7. Use of sufficient water (1 cup or more) 54.a) Is there a hand washing facility? 1.Yes 2. No b) If yes, which type? i) Tilting can ii) Leak tins iii) Stand pipe iv) Basin v) Sufuria 55.Is there soap at this location? 1.Yes 114 2.No 56.Do you have soap in the house? 1.Yes 2.No 57.Can I see your drinking water storage container? (Confirm presence and circle one. If unable to see container confirm type orally) 1.Ordinary clay pot 2.Plastic jerry can 3.Plastic or metal bucket 4.Container with narrow mouth and tap 5.Superdrum/tank 6.Other, specify _________________________________ 58.Does this container have a lid or cap? (Confirm by observation) 1.Yes 2.No 59.Can you please retrieve a small bit of water for me? (Observe). 1.Dip into container 2.Pour directly from container 3.Tap 60.Test free chlorine if they said they have treated current drinking water 1.Presence of Chlorine 2.Absence of Chlorine 3.Insufficient water for testing 61. a) Do you know some diseases associated with drinking contaminated water? 1. Yes 2. No b) If yes, name them; 1.Typhoid 5.Malaria 2.Cholera 6.URTI 3.Intestinal warms 7.HIV/AIDs 4.Diarrhoea 8.Others (specify)_________________________ c) How can we prevent these diseases mentioned above? 1.Boiling water 2.Use of household filters 3.Use of water guard 4.Treating water with PUR 115 5.Go to Hospital 6.Traditional healer 7.Others(specify)___________________ 62.Who collects water for the family? 1. Men 2. Women 3. Children 63 a) How is water stored in the household container/Covered (Observe) 1.Open container 2. b) How do you draw water from the container? 1 Dipping 2 Pouring 3.Tapping c) Do you keep the container for drawing water? 1.On the floor. 2.Container with handle 3.In the cupboard 4.No special place G:Diseases: 63. What diseases have the under five suffered for the last six months (1Record 2. History) 1. Malaria 2. Intestinal worms 3. T.B 4. Scabies 5. Eye diseases. 6. Diarrhoea 7. Respiratory infections 8. HIV/AIDs 9.Measles 10.Others 64. What disease is/are the under five suffering from at the time of the visit? (By signs, symptoms and observation) 1. Fever 2. Coughing 3. Measles 4. Scabies 5. Eye diseases. 6. Diarrhoea 7. Respiratory infections 8. No disease. 9. Others specify______________________________ 65. Do you know the cause of the disease you have mentioned? 1. Yes 2. No 116 66. If sick where do you go for treatment? 1.Hospital/Health Facility 2..Buy medicines in the shops 3.Traditional healers. 4.Prayer. 5.Traditional beliefs ..... END..... THANK THE RESPONDENT 117 APPENDIX 2: WATER SAMPLING AND REPORT FORM For laboratory testing, please take a sample of water from the container where households store drinking water. Household number Sample number Mg/L chlorine level Faecal coliform Total coliform Count (%) Count (%) 118 Water culture results APPENDIX 3: Biochemical reaction of Enterobacteriaceae, Aeromonas and pleisomonas after 18-24 hours incubation at 350C. TSI agar LIM medium OrgaSlun Gas H2S Lys Mot Ind MR VP S.C Ure Ox nism t/Bu s tt *Escd +/ - d d + + - - - - + + - + - + - + d - /+ - - + + + - + + - /+ - - + + + - + + - /+ + + + + + - - - - heri / + chia Cit. d freu / + ndii C. + dive + rsus C. + amal+ oneti cus Edw adsi + 119 ella tard a E. + /+ + + + + + - - - - /+ - + - - d + + - - d - d - - + - d d - - - - - - + - - - - /+ - + - + - + + + - hosh + inae Kleb + siell + a pneu moni ae K. d ozae / + nae K. d rhin / + oscl ero mati s K. + 120 oxyt + oca Hafnd ia + - + + - d d d - - /+ - - + - - + + - - /+ - - + d d + + - - /+ - + + - - + + - - /+ - + + - d + + + - / + alvei Ente + roba + cter cloa cae E. + saka + zakii E. + aero + gene s E. + gerg + ovia e 121 E. d d - - d d d d d d - /d - + + - - + + d - /- - d + - d + + - - /d - d + - d d + - - /d - - + - d + + - - d + - + + + - d + - aggl / + ome rans Serr + atia + mar cesc ens S. + mani+ roru bra S. + lique+ facie ns S. + plym + uthic a Prot d 122 eus / + vulg aris P. d + + - + - + d + + - /d - - + + + - - + - + - - + + + - + - - - - - + + + - + - - d - - + + + - + + - mira / + bilis Mor gane + lla mor gani i Prov d iden / + cia alkal ifaci ens P. d stua / + rtii P. d 123 rettg / + eri * + /- - - - d + - - + - /- - - - - + - - + - /d - - - + d d - + - /d - - - + d d - + - Yers + inia ente roco litic a Y. - pseu + dotu berc ulosi s Y. + inter + medi a Y. + fred + eriks enii 124 Y. - / - - - d + - /- - - - d + - - - - /d - - - - + - - - - /d - - - + + - - - - +/ +/ - + - +/ - - krist + ense nii * - Shig + ella in gene ral * S. flex + neri 6 * S. boyd + ii 13 & 14 Sal - // / + / +/ mon + ella 125 *S. - /+ + + + - + - + - - /- +// + +/ - + - - - - /+ -// - + - + - - - - /+ -// d + - + - - - - /+ d + + - + - d - - chol + erae suis in gene ral * S. typh + i * S. para + typh iA * S. send + ai * S. chol + erae suis 126 * S. - /+ - - + - + - - - - /+ - + + - + - - - - /+ - + + - + - - - - /d d + - - + - - - - /+ - d + + + + d - + typh + isuis * S. abor + tuse qui * S. abor + tuso vis * S. galli + nar um * + Aero+ mon as hydr ophi la 127 * A. + /+ - d + + + + d - + /- - - + + + - d - + /- - + + + + - - - + /- - + + + + - - - + *: Enteropathogenic In TSI medium - -/+, ferment glucose only; +/+ ferment glucose, and lactose or sucrose or both; d/+ ferment glucose and fermentation of lactose or glucose shows different reactions; Gas, gas from glucose(TSI). sobr + ia A. + cavi + ae *Ple isom + onas shig elloi des (Vib rio + para hae moly ticus ) Keys: 128 Lys. – lysine decarboxylase; Mot.- motility; Ind. – indole(LIM); MR, - methyl red; VP, - Voges-proskauer; S.C, - citrate; Ure, - urease; Ox, - cytochrome oxidase; -, negative; +, positive; d, different reactions; +/, rarely negative; -//, rarely positive. APPENDIX 3: MAP OF STUDY AREA APPENDIX 4: ETHICS AND RESEARCH CLEARANCE APPENDIX 5: PUBLISHED PAPERS 129 130 131