Unusual Compression Neuropathies of the Forearm, Part II: Median
advertisement

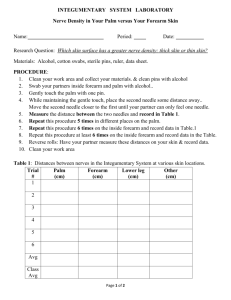
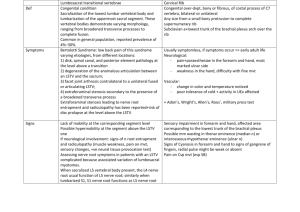
CURRENT CONCEPTS Unusual Compression Neuropathies of the Forearm, Part II: Median Nerve Alan C. Dang, MD, Craig M. Rodner, MD is formed from the terminal divisions of the medial and lateral cords of the brachial plexus, receiving contributions from the roots of the 5th, 6th, 7th, and 8th cervical nerves and the 1st thoracic nerve. It travels through the upper arm medial to the brachial artery, giving off no branches to muscles above the elbow, with the possible exception of a distinct fascicular bundle that may leave the parent nerve to innervate the pronator teres. In the distal aspect of the upper arm proximal and medial to the medial epicondyle, a supracondylar process, with its attached ligament of Struthers, represents a possible site of median nerve compression. The brachial artery may accompany the median nerve deep to the ligament of Struthers, or be superficial to it (Fig. 1). In marsupials, the median nerve actually travels through a supracondylar foramen in this area of the distal humerus. Although no such foramen exists in humans, approximately 0.6% to 2.7% of us have a residual supracondylar process with a vestigial fibrous band connected to it that inserts into the medial epicondyle.1–3 This fibrous band, known today as the ligament of Struthers, was interestingly first recognized by Tiede- T HE MEDIAN NERVE From the Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT. Received for publication September 22, 2009; accepted in revised form October 17, 2009. No benefits in any form have been received or will be received related directly or indirectly to the subject of this article. Corresponding author: Craig M. Rodner, MD, Department of Orthopaedic Surgery, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT 06034-4037; e-mail: rodner@uchc.edu. 0363-5023/09/34A10-0028$36.00/0 doi:10.1016/j.jhsa.2009.10.017 mann in 18223; Struthers was the first person to describe median nerve entrapment by this structure in 1848.4 As it travels across the elbow and enters the forearm, the median nerve passes under the bicipital aponeurosis or lacertus fibrosus into the antecubital region, medial to both the biceps tendon and brachial artery, and volar to the brachialis (Fig. 2). The median nerve then passes between the 2 heads of the pronator teres, deep to the humeral head and superficial to the ulnar head; although rarely the ulnar head may be absent.5 After this, the nerve travels deep to the proximal fibrous arch of the flexor digitorum superficialis (FDS) (Fig. 3) before continuing its course through the forearm between the FDS and the flexor digitorum profundus (FDP). In this area, approximately 4 cm distal to the medial epicondyle or 5 to 8 cm distal to the lateral epicondyle, the anterior interosseous nerve (AIN) courses off of the main trunk of the median nerve to innervate the flexor pollicis longus (FPL), FDP to the index and middle fingers, and the pronator quadratus (Fig. 4).6 At approximately 4 to 5 cm proximal to the wrist crease, the palmar cutaneous branch of the median nerve branches off to supply sensory innervation to the radial palm.7 The median nerve ultimately continues through the carpal tunnel, where, of course, it is at greatest risk for compression. Although there are several possible areas for median nerve compression proximal to the carpal tunnel, including by the ligament of Struthers, the bicipital bursa, anomalous arteries, and anomalous muscles (such as Gantzer’s muscle, an accessory FPL muscle),8,9 pronator syndrome and AIN syndrome remain the 2 most frequently referenced compression neuropathies of the median nerve in the forearm. © Published by Elsevier, Inc. on behalf of the ASSH. 䉬 1915 Current Concepts We have previously discussed compression neuropathies of the radial nerve in the forearm. In the second half of this 2-part review, we will now turn our attention to 2 compression neuropathies affecting the proximal median nerve, before its entry through the carpal tunnel: (1) pronator syndrome and (2) anterior interosseous nerve syndrome. (J Hand Surg 2009;34A:1915–1920. © 2009 Published by Elsevier Inc. on behalf of the American Society for Surgery of the Hand.) Key words Pronator syndrome, anterior interosseous syndrome. 1916 RADIAL NERVE COMPRESSION FIGURE 3: Schematic of the median the nerve as it passes beneath the proximal fibrous arch of the flexor digitorum superficialis in the forearm. FIGURE 1: Schematic of the median nerve above the elbow as it travels medial to the brachial artery. The artery may be superficial to the ligament of Struthers (as shown here) or accompany the median nerve deep to it. FIGURE 4: Schematic of the AIN as it branches off of the main trunk of the median nerve deep to the flexor digitorum superficialis. Current Concepts FIGURE 2: Schematic of the median nerve as it enters the forearm, deep to the bicipital aponeurosis, and medial to both the biceps tendon and brachial artery. PRONATOR SYNDROME (PS) Pronator syndrome commonly refers to compression of the median nerve as it passes between the 2 heads of the pronator teres muscle or under the proximal edge of the proximal FDS arch. Symptoms usually have an insidious onset and typically are not diagnosed as part of an overall clinical syndrome for months to years.10 –12 PS typically presents with aching pain in the proximal, volar forearm with paresthesias radiating into the thumb, index finger, middle finger, and the radial half of the ring finger, similar to the sensory alterations of carpal tunnel syndrome (CTS). These symptoms are often made worse by repetitive pronosupination movements. As originally described by Seyffarth in 1951,13 PS is actually a somewhat misleading term because it actually refers to compression of the median nerve at more anatomic sites than just the pronator teres. Discriminating clinically between PS and CTS can be difficult because of their shared symptoms in the median nerve–innervated radial 3½ digits and pain in the volar wrist and forearm. However, several discriminating factors can aid in the differential diagnosis. Because the palmar cutaneous branch of the median nerve arises 4 to 5 cm proximal to the transverse carpal ligament,7 a patient presenting with CTS-like symp- JHS 䉬 Vol A, December RADIAL NERVE COMPRESSION 1917 toms in addition to decreased sensation over the thenar eminence should be evaluated for a more proximal lesion (ie, a cervical radiculopathy, brachial plexopathy, or a more proximal compression of the median nerve). Unlike patients with CTS, individuals with PS should not have a Tinel sign over the wrist, nor should their symptoms be provoked with wrist flexion. For this reason, unlike CTS, PS does not characteristically produce nocturnal symptoms.10 In patients with PS, a helpful examination maneuver is to resist the patient’s pronation of his or her forearm in a neutral position. If pain or parasthesias are reproduced during this maneuver as the elbow is extended, the clinician should suspect entrapment of the median nerve at the level of pronator teres.14 If resisted contraction of the FDS to the middle finger reproduces symptoms, median nerve compression at the level of the fibrous arch between the heads of the FDS might be suspected.14 If symptoms are elicited by resisted flexion of the forearm in full supination, compression at the more proximal level of the lacertus fibrosus might be considered.15 Electrodiagnostic studies can be useful in the diagnosis of PS in that they may exclude other sites of nerve compression or help identify a double-crush syndrome.16 AIN SYNDROME The first description of an AIN neuropathy can be attributed to Duchenne de Boulogne, who reported an isolated palsy of the FPL in 1872.20 In 1952, Kiloh and Nevin described in detail the clinical manifestations of FIGURE 5: A characteristic physical examination finding in AIN syndrome is that a patient will be unable to flex his thumb interphalangeal joint and index finger distal interphalangeal joint to make an “OK” sign, as this patient can. an isolated compression of the AIN.21 Because the AIN is a motor-only nerve innervating the deep muscles of the forearm (FPL, FDP to the index and middle fingers, and pronator quadratus), a patient with a complete AIN palsy would present with no motor function to all 3 of these muscles. Patients with incomplete palsies or with Martin-Gruber anastomoses (in which axons of the AIN may, for example, cross over to innervate the hypothenar muscles)22 may present differently. In addition, the clinician must consider that the FDP to the middle finger may not always be exclusively innervated by the median nerve, so intact middle finger distal interphalangeal joint flexion does not unto itself exclude AIN syndrome as a potential diagnosis. Patients with AIN syndrome most commonly recognize weakness or absence of FPL function. Although no sensory loss occurs, pain may be present in the forearm along the course of the nerve. A characteristic physical examination finding is a patient’s inability to make an “OK” sign when asked by the examiner to flex his thumb interphalangeal joint and index finger distal interphalangeal joint (Fig. 5). In patients with mild AIN JHS 䉬 Vol A, December Current Concepts Management Surgery is usually not necessary to treat PS. Not surprisingly, first-line treatments such as the avoidance of aggravating activities, rest of the extremity, and nonsteroidal anti-inflammatory medication are frequently successful in alleviating symptoms. Conservative management has been shown to be effective in 50% to 70% of patients.11,17 Corticosteroids have also been shown to be efficacious.18 When a space-occupying lesion is present or a several-month course of nonsurgical treatment fails, surgery may be indicated.19 The surgical approach used for decompression of the median nerve in the forearm will be discussed in more detail in the next section on AIN syndrome. The success rate with surgery in the treatment of PS approaches 90% in the literature,10,11,17 although there remains no consensus on how long to pursue nonsurgical treatment before surgical intervention; and yet again, no randomized clinical trials exist comparing surgery with conservative management. 1918 RADIAL NERVE COMPRESSION FIGURE 6: A patient with AIN syndrome may be unable to pinch a sheet of paper between his thumb interphalangeal joint and index finger distal interphalangeal joint, and may compensate by using a more adaptive grip in which these joints remain extended. Current Concepts compression, subtle weakness of these muscles may be the only clinical finding. Such weakness of the FPL and index finger FDP may be uncovered by asking the patient to pinch a sheet of paper between his thumb and index finger using only the fingertips and then trying to pull the paper away. A patient with AIN syndrome may be unable to hold on to the sheet of paper with just his fingertips and may compensate by using a more adaptive grip in which the interphalangeal joint of the thumb and distal interphalangeal joint of the index finger remain extended (Fig. 6). A noncompressive neuropathy, such as a brachial neuritis,23 may mimic the clinical manifestations of an AIN neuropathy and must be considered in the differential diagnosis. A sudden onset of symptoms associated with a viral prodrome suggests the diagnosis of such a viral neuritis (Parsonage-Turner syndrome)23 instead of a compression neuropathy. It is also important to consider rupture of the FPL tendon in the differential diagnosis, which may occur in patients with rheumatoid arthritis. To exclude this diagnosis, the wrist should be passively flexed and extended to confirm that the patient has an intact tenodesis effect. If the tendons are intact, passive wrist extension brings the thumb interphalangeal joint and index finger distal interphalangeal joint into a relatively flexed position compared with when the wrist is passively flexed. Electrodiagnostic studies are an important element in the workup of AIN syndrome because they confirm the diagnosis and objectively assess the severity of the neuropathy. Electromyography is often helpful in ruling out more proximal lesions as a cause of the symptoms, as well as distinguishing AIN syndrome from a flexor tendon rupture in patients with severe rheumatoid disease who have such limited wrist motion that determination of an intact tenodesis effect is impossible. Imaging studies, such as magnetic resonance imaging (MRI), are not commonly used in the diagnosis of AIN syndrome, although there is literature describing the MRI findings associated with AIN syndrome in which increased signal intensity can be seen in the AINinnervated muscles on T2-weighted, fat-saturated images or short inversion time inversion recovery sequences.24,25 MRI may actually provide a theoretical advantage of increased sensitivity over electrodiagnostic studies in that abnormal findings after nerve injury are detectable earlier with MRI (alterations in signal intensity can be seen as early as 4 days after injury) than they are with electromyography (which requires 2 to 3 weeks).26 In clinical practice, this theoretical advantage is unlikely to affect the treatment course. Management Once the diagnosis of AIN syndrome is made, treatment should begin nonsurgically with the typical regimen of rest, splinting, and observation. Because most patients with AIN syndrome seem to improve without any surgical intervention,27,28 observation for a period of several months has been suggested before decompression.8 For those patients who have a space-occupying mass in the area, or who fail a several-month course of nonsurgical treatment, surgical decompression has been recommended. As we saw to be the case with compression neuropathies of the radial nerve, there is a paucity of high-quality literature supporting the appropriate duration of conservative treatment in this condition as well. The surgical approach for patients with PS or AIN syndrome is performed through a lazy-S–type incision that begins with an exploration of the median nerve proximal to the antecubital flexion crease, as this allows for identification of the median nerve proper and exposure of the ligament of Struthers if need be. Of course, JHS 䉬 Vol A, December RADIAL NERVE COMPRESSION Controversy There is controversy surrounding the treatment of PS and AIN syndrome in that it is extremely difficult to glean from the literature when surgical intervention is appropriate. Because the natural history of PS and AIN syndrome is not well delineated and no randomized, controlled trials exist comparing conservative and surgical treatments, it is difficult to make evidence-based recommendations on the timing of surgical intervention. For AIN syndrome, Spinner recommended surgical exploration after 12 weeks of persistent symptoms or a persistent abnormality on electrodiagnostic studies.30 However, spontaneous recovery has been seen even as long as 1 year after the onset of symptoms.27,31–34 In Miller-Breslow et al.’s series of 10 patients with AIN syndrome, 8 who were treated by observation alone had signs of spontaneous recovery within 6 months and went on to a full recovery by 1 year.27 Nakano and colleagues reported on 2 patients with bilateral AIN palsies, with separate times of onset for each side.28 The first side was treated surgically, whereas the contralateral side was treated nonsugically. Interestingly, all 4 extremities recovered and surgery did not produce an earlier return of function. Stern reported 3 cases of AIN syndrome that failed to respond to nonsurgical treatment after 3 to 5 months, which then went on to a complete resolution of symptoms 5 months after surgical decompression.35 Proponents of surgical decompression point to the case series of Schantz and Riegels-Nielsen who re- ported on 20 patients with AIN syndrome, 15 of whom underwent surgical decompression.36 Satisfactory function after surgery was reported in 11 patients (73%), whereas nonsurgical management had only a 40% rate of recovery. Moreover, 3 of the 5 patients treated nonsurgically were noted as having a persistent palsy at 4-year follow-up. Because a clinical AIN palsy may result from a compression neuropathy of the AIN proper, a compression of the median nerve more proximally, an AIN neuritis, or some combination of the 3, the studies in the literature may in fact be reporting upon patients with different etiologies of AIN dysfunction. Antecedent pain or systemic prodromic symptoms such as fever, malaise, or myalgias are suggestive of more an inflammatory etiology than a compressive one. Since all of Miller- Breslow et al.’s patients reported a prodome of forearm pain, it is possible that at least several of the patients in their study may not have had a true compression neuropathy.27 In cases of AIN neuritis, an extended course of conservative therapy is warranted, as a spontaneous resolution of symptoms seems to be the norm. In the absence of evidence suggesting a neuritis, most authors still recommend a trial of conservative management of at least 12 weeks,34 although the prognosis for spontaneous recovery in such patients seems to be more guarded. Although compression neuropathies of the forearm, such as those of the median nerve, present far less frequently than those of the wrist, it is essential that clinicians consider these less common entities when evaluating their patients. Once a diagnosis is made, conservative management, including avoidance of aggravating activities, rest, and anti-inflammatory medication, is recommended. If symptoms persist despite these measures, surgery is appropriate and has been shown to be effective. Randomized, controlled trials examining the ideal duration of nonsurgical management and the timing of surgical intervention for PS and AIN syndrome (as well as for compression neuropathies of the radial nerve in the forearm) are warranted. REFERENCES 1. Newman A. The supracondylar process and its fracture. Am J Roentgenol Radium Ther Nucl Med 1969;105:844 – 849. 2. Struthers J. On hereditary supra-condyloid process in man. Lancet 1873;1:231–232. 3. Lonsdale H. A sketch of his life and writings of Robert Knox, the anatomist. London: Macmillan, 1870;249. 4. Struthers J. On a peculiarity of the humerus and humeral artery. Monthly J Med Sci (Edinburgh) 1848;9:264 –267. 5. Dellon A, Mackinnon SE. Musculoaponeurotic variations along the course of the median nerve in the proximal forearm. J Hand Surg 1987;12B:359 –363. JHS 䉬 Vol A, December Current Concepts the surgical approach and extent of proximal exploration can be tailored to the surgeon’s specific areas of preoperative concern. After the median nerve is released proximally, it is dissected free from the overlying lacertus fibrosus,15 the humeral head of the pronator teres, and the proximal fascial edge of the FDS arch. Gantzer’s accessory FPL muscle, if present, should also be released.29 The surgeon should note that nearly all of the median nerve’s branches course off its ulnar side at this level, with the notable exception being the AIN, which branches off the radial side of the nerve. In patients with AIN syndrome, the AIN should be thoroughly decompressed from any overlying tissue and completely visualized as it travels into the distal forearm. As was the case with decompression of the posterior interosseous nerve, meticulous hemostasis is essential during median nerve decompression in the forearm, to minimize a postoperative hematoma. The wound is closed in layers and early active range of motion is allowed. 1919 1920 RADIAL NERVE COMPRESSION 6. North ER, Kaul MP. Compression neuropathies: median. Vol. 1. New York: McGraw-Hill, 1996:1307–1336. 7. Bezerra AJ, Carvalho VC, Nucci A. An anatomical study of the palmar cutaneous branch of the median nerve. Surg Radiol Anat 1986;8:183–188. 8. Lubahn J, Cermak M. Uncommon nerve compression syndromes of the upper extremity. J Am Acad Orthop Surg 1998;6:378 –386. 9. Horak B, Kuz JE. An unusual case of pronator syndrome with ipsilateral supracondylar process and abnormal muscle mass. J Hand Surg 2008;33A:79 – 82. 10. Hartz CR, Linscheid RL, Gramse RR, Daube JR. The pronator teres syndrome: compressive neuropathy of the median nerve. J Bone Joint Surg 1981;63A:885– 890. 11. Johnson RK, Spinner M, Shrewsbury MM. Median nerve entrapment syndrome in the proximal forearm. J Hand Surg 1979;4:48 –51. 12. Werner C, Rosen I, Thorngren KG. Clinical and neurophysiologic characteristics of the pronator syndrome. Clin Orthop 1985;197: 231–236. 13. Seyffarth H. Primary myoses in the M. pronator teres as cause of lesion of the N. medianus (the pronator syndrome). Acta Psychiatr Neurol Scand Suppl 1951;74:251–254. 14. Tetro A, Pichora DR. High median nerve entrapments: an obscure cause of upper extremity pain. Hand Clin 1996;12:691–703. 15. Swiggett R, Ruby LK. Median nerve compression neuropathy by the lacertus fibrosus: report of three cases. J Hand Surg 1986;11A:700 – 703. 16. Rehak DC. Pronator syndrome. Clin Sports Med 2001;20:531–540. 17. Tsai TM, Syed SA. A transverse skin incision approach for decompression of pronator teres syndrome. J Hand Surg 1994;19B:40 – 42. 18. Morris H, Peters BH. Pronator syndrome: clinical and electrophysiological features in seven cases. J Neurol Neurosurg Psychiatry 1976;39:461– 464. 19. Spinner M, Spencer PS. Nerve compression lesions of the upper extremity: a clinical and experimental review. Clin Orthop Relat Res 1974:46 – 67. 20. Duchenne de Boulogne GBA. De l’électrisation localisée. Vol. 1. 3rd ed. Paris: J.-B. Baillière, 1872:1120 21. Kiloh LG, Nevin S. Isolated neuritis of the anterior interosseous nerve. Br Med J 1952;1:850 – 851. 22. Rodriguez-Niedenfuhr M, Vazquez T, Parkin I, Logan B, Sanudo JR. Martin-Gruber. Anastomosis revisited. Clin Anat 2002;15:129 –134. 23. Parsonage MJ, Aldren I, Turner JW. Neuralgic amyotrophy (paralytic brachial neuritis) with special reference to prognosis. Lancet 1957;ii:209 –212. 24. Dunn AJ, Salonen DC, Anastakis DJ. MR imaging findings of anterior interosseous nerve lesions. Skeletal Radiol 2007;36:1155– 1162. 25. Grainger AJ, Campbell RS, Stothard J. Anterior interosseous nerve syndrome: appearance at MR imaging in three cases. Radiology 1998;208:381–384. 26. West GA, Haynor DR, Goodkin R, Tsuruda JS, Bronstein AD, Kraft G, et al. Magnetic resonance imaging signal changes in denervated muscles after peripheral nerve injury. Neurosurgery 1994;35:1077– 1085; discussion, 85– 86. 27. Miller-Breslow A, Terrono A, Millender LH. Nonoperative treatment of anterior interosseous nerve paralysis. J Hand Surg 1990; 15A:493– 496. 28. Nakano KK, Lundergran C, Okihiro MM. Anterior interosseous nerve syndromes: diagnostic methods and alternative treatments. Arch Neurol 1977;34:477– 480. 29. Tsai P, Steinberg DR. Median and radial nerve compression about the elbow. J Bone Joint Surg 2008;90A:420 – 428. 30. Spinner M. Injuries to the major branches of peripheral nerves of the forearm. Philadelphia: WB Saunders, 1978:160 –227. 31. Seror P. Anterior interosseous nerve lesions: clinical and electrophysiological features. J Bone Joint Surg 1996;78B:238 –241. 32. Seror P. [Anterior interosseous nerve lesions revisited in 2004]. Rev Med Liege 2004;59(Suppl 1):58 – 66. 33. Sood MK, Burke FD. Anterior interosseous nerve palsy: a review of 16 cases. J Hand Surg 1997;22B:64 – 68. 34. Sunderland S. Nerves and nerve injuries. 2nd ed. Edinburgh: Churchill Livingstone, 1978:695– 696. 35. Stern MB. The anterior interosseous nerve syndrome (the KilohNevin syndrome): report and follow-up study of three cases. Clin Orthop Relat Res 1984;187:223–227. 36. Schantz K, Riegels-Nielsen P. The anterior interosseous nerve syndrome. J Hand Surg 1992;17B:510 –512. Current Concepts JHS 䉬 Vol A, December