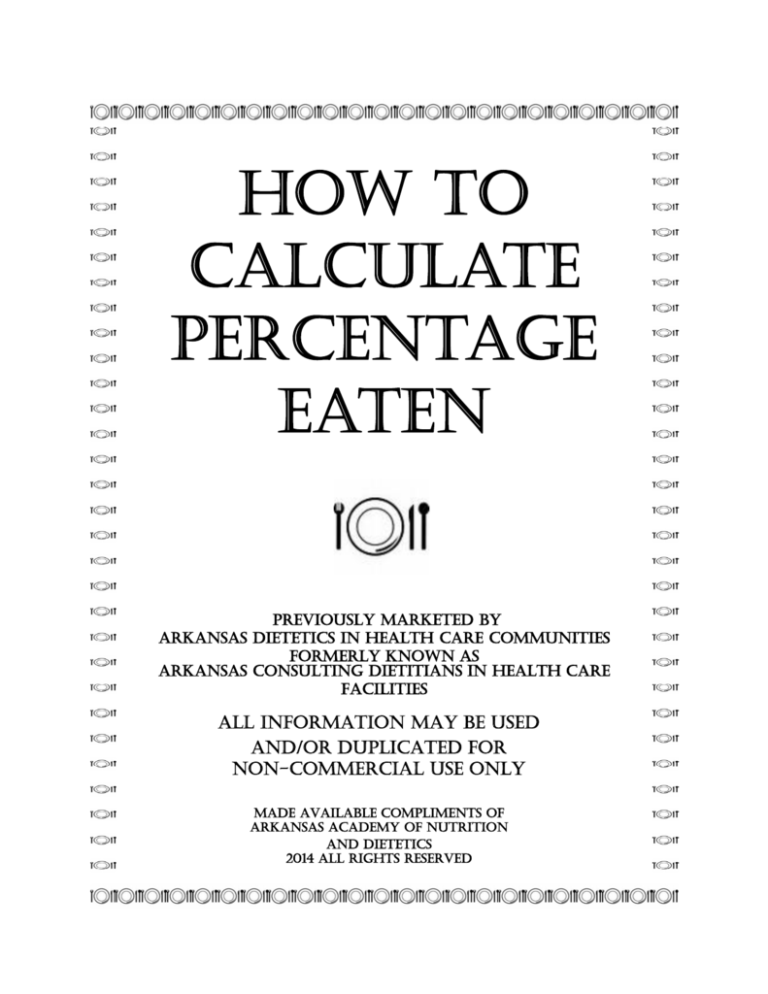
HOW TO
CALCULATE
PERCENTAGE
EATEN
previously marketed by
arkansas dietetics in health care communities
formerly known as
ARKANSAS CONSULTING DIETITIANS IN HEALTH CARE
FACILITIES
all information may be used
and/or duplicated for
non-commercial use only
made available compliments of
arkansas academy of nutrition
and dietetics
2014 all rights reserved
2
3
HERE IS HOW!
STEP 1: COUNT THE NUMBER OF SERVINGS ON THE TRAY. (See chart on next page
for items to count.)
TOTAL SERVINGS COUNTED
ITEM
COUNTED
Coffee
No
0
Milk
Yes
+1 = 1
Chicken
Yes
+1= 2
Potato Salad
Yes
+1 = 3
Baked Beans
Yes
+1 = 4
Bread
Yes
+1 = 5
Pie
Yes
+1 = 6
Tomato Garnish
No
+0 = 6 Total Servings Counted
STEP 2:
ESTIMATE AND ADD THE TOTAL SERVINGS EATEN OF ITEMS
COUNTED:
ITEM
COUNTED
Coffee
No
TOTAL SERVINGS COUNTED
0
Milk
1/2 serving
1/2 serving +
Chicken
1/4 serving
1/4 serving = 3/4 serving +
Potato Salad
1/2 serving
1/2 serving = 1 1/4 servings +
Baked Beans
0 serving
0 serving = 1 1/4 servings +
Bread
1 serving
1 serving = 2 1/4 servings +
Pie
Tomato Garnish
1/4 serving
1/4 serving = 2 1/2 servings eaten
No
STEP 3: ROUND SERVINGS EATEN TO NEARSEST 1/2 SERVING. (There is no need to
Answer: 2 1/2 SERVINGS EATEN
round in this example.)
STEP 4: REFER TO THE CHART ON THE FOLLOWIING PAGE TO CHANGE TOTAL
NUMBER OF SERVINGS EATEN TO PERCENTAGE. LOCATE THE TOTAL NUMBER OF
SERVINGS EATEN (STEP 3: 2 1/2) ALONG THE TOP OF THE CHART.
LOCATE THE TOTAL NUMBER OF SERVINGS COUNTED (STEP 1: 6) ALONG THE SIDE
OF THE CHART. THE PERCENTAGE EATEN WILL BE FOUND WERE THE TWO
POINTS MEET. (42%)
4
Author grants permission for use of copyrighted material for educational & non-commercial use only.
A credit line of "Compliments of Arkansas Academy of Nutrition and Dietetics" must be used. 2014 All Rights Reserved
5
INSERVICE
Title: Why & How to Calculate Percentage Eaten of Meal Trays Served to the Elderly
in Long Term Care Facilities Using a Method Endorsed by the Arkansas CD-HCF
Suggested Materials:
Reference Chart from Arkansas CD-HCF on How To Calculate Percentage Eaten
Copies of Post Test (included in this material)
Case Examples (included in this material) and/or Sample Trays of Meals Eaten
Key In-service Material (from this booklet) Outlined on a Flip Chart
Target Audience: All Nursing Staff, Food & Nutrition Staff
Learning Objectives: Upon completion of the in-service the participant will be able to
1. Identify common causes of weight loss
2. Identify effects of protein-calorie undernutrition which result in weight loss
3. Demonstrate accurate calculation of percentage consumption of sample trays
Method: Discussion/Activities/Post Test
I. Discussion
Summary of topics to be covered:
The “WHY”
A. Our goals and responsibility to the residents of long term care
facilities.
B. Why do we monitor weight and determine percentage eaten?
C. What causes weight loss in older persons?
D. What happens to body composition with weight loss and gain cycles?
E. What is the effect of weight loss (protein-energy) undernutrition in
older persons?
F. Prevention-(an ounce of prevention is worth a pound of cure.)
The “HOW TO”
G. How to accurately calculate percentage eaten using this method
endorsed by the Arkansas CD-HCF.
H. Commonly asked questions when calculating percentage eaten using
this method.
6
A. Our goals and responsibility to the residents of long term care facilities
Our goal and responsibility as care givers is to ensure that residents achieve highest
levels of functioning possible (Quality of Care) and maintain their sense of
individuality (Quality of Life).1
This should include meeting the nutritional needs of residents, as well as, maintaining
their health and dignity which represents their quality of life. 4, 1
From a nutrition perspective this would mean that caregivers must ensure that
residents maintain optimal food and fluid intakes while at the same time maintaining
and/or preserving their lean muscle mass.
B. Why is weight monitored and percentage eaten determined?
1. A major indicator of nutritional status is a resident’s weight history and/or changes.
2. Percentage of food eaten must be accurately determined in order to answer
questions K4c (Leave 25% or more of food uneaten at most meals) and K6a (Code the
proportion of total calories the resident received through parenteral or tube feeding in
the last 7 days) on the Minimum Data Set Version 2.0, which is required to be
completed in long term care facilities by the Omnibus Budget Reconciliation Act of
1987 (OBRA '87) 1 Questions found to be inaccurate when audited may impact
reimbursement rates.
To evaluate the effectiveness of nutrition intervention of a resident’s nutritional status,
dietitians use information taken from food intakes in long-term-care settings. The
Omnibus Senate Reconciliation Act of 1987 (OBRA) mandates that these figures be
used when completing the Minimum Data Set. OBRA guidelines require a physical
and health reassessment of a resident if he or she eats 75% or less of most meals.
These records are also included in the governmental monitoring process used by state
inspectors. 5
3. Monitoring meal consumption provides the quickest indicator or trigger to alert
staff of a potential problem which may result in decreased nutritional status and/or
weight.
A study of 72 non-severely diseased elderly concluded that food intake is a strong
predictor of survival even in moderately diseased elderly patients, suggesting possible
low cost interventions. 2
Although the nutrient requirements of this population are not yet well understood,
nutrition care is recognized as an important factor in improving longevity and quality
of life. 1
7
4. Weight loss corresponds to increased morbidity and mortality.
The first National Health & Nutrition Examination Survey found that female subjects
from 45 to 74 had increased mortality with weight loss even if severely overweight;
however, weight loss of 5% - 15% decreased mortality in severely overweight men
(BMI >29).3
Those in institutional care are at a higher nutritional risk than others. Involuntary
weight loss is damaging to the health and welfare of older people, especially those
living in a nursing facility. 11, 3 Frail older adults are at an increased risk of developing
malnutrition and its consequences. Even less frail older adults living in the
community are at risk for poor nutrition with studies indicating three percent of men
and six percent of women are underweight.
5. Weight fluctuation of 3+ pounds would indicate that the resident’s hydration status
be considered.1 Dehydration especially in the elderly is associated with significant
morbidity and mortality.4
A common problem in nursing homes is dehydration. It is associated with significant
morbidity and mortality including a higher prevalence of pressure sores, delayed
wound healing, and increased rates of infection. 2
C. What causes weight loss in older persons?
A number of common causes are included in the mnemonic MEALS-ON-WHEELS 7
M edication effects
E motional problems, especially depression
A norexia nervosa, Alcoholism
L ate-life paranoia
S wallowing disorders
O ral factors (e.g., poorly fitting dentures, caries)
N o money (poverty)
W andering and other dementia-related behavior
H yperthyroidism, hypothyroidism, hyperparathyroidism, hypoadrenalism
E Enteric problems
E ating problems (e.g., inability to feed self)
L ow-salt, low cholesterol diet
S tones, social problems (e.g., isolation, inability to obtain preferred foods)
Since factors which cause weight loss are SOCIAL, PSYCHOLOGICAL, MEDICAL,
& AGE RELATED, it is critical for the entire interdisciplinary team to work together
to help prevent weight loss.
8
D. What happens to a person’s body composition with weight loss then weight gain?
1. The percentage of the weight loss that is muscle versus fat will vary with the type of
diet whether the loss was planned or unplanned. (Record this on flip chart to reference.)
“Obese clients who lose weight due to a stress response typically lose lean body mass
and retain their fat reserves. It is imperative to recognize that the energy and protein
needs of stressed older adults are higher than those of healthy individuals.” 11
Percent of Weight Loss
Lean Body Mass
Fat
68 %
32 %
Ketogenic Diets
< 1000 Kcal/day
65 %
35 %
Mixed Food Diets
< 1000 Kcal/day
40 %
60 %
Mixed Food Diets
> 1000 Kcal/day
32 %
68 %
Mixed Food Diets + Mild Exercise
> 1000 Kcal/day
21 %
79 %
Starvation OR Fasting
2. Weight gained back after initial loss will be a greater percentage of fat to lean than
what was initially lost unless the weight gain is done in conjunction with high-intensity
resistance training.6 This is why it is so critical for the interdisciplinary care team to
prevent weight loss before it happens.
“Various studies have demonstrated a strong correlation between weight loss and
morbidity and mortality. One study showed that nursing home patients had a
significantly higher mortality rate in the six months after losing 10 percent of their
body weight, irrespective of diagnoses or cause of death.” 7
3. It is encouraging that older individuals both healthy and frail including those up to
100 years of age, have been shown to respond to high-intensity resistance training with
both muscle hypertrophy and marked increases in strength. 7
Exercise can help make up for some of the adverse changes in body composition that
can occur with aging. Resistive, weight-bearing aerobic exercise has shown to stabilize
or increase bone mass in pre-and postmenopausal women and older men. 6
9
E. What is the effect of protein-energy undernutrition (weight loss) in older persons? (Record
this on flip chart to reference.)
Some effects include: 9
Anemia
decreased cognition
edema
falls
hip fractures
immune dysfunction
infections
muscle loss
osteoporosis
pressure sores
In institutionalized older adults, weight loss may be a result of both emotional and
physical conditions. Increased mortality has been associated with unintentional weight
loss and protein-energy malnutrition. Pressure ulcers and a decreased resistance to
infection can also be seen with unintentional weight loss. 1
F. Prevention - An ounce of prevention is worth a pound of cure.
1. The effects of protein-calorie undernutrition translate into decreased ability of the
elderly to accomplish their Activities of Daily Living (ADLs) which in turn creates
increased work loads for the caregivers. Weight loss is usually detrimental not only for
the older individual who experiences it, but also for the caregiver (due to increased
work load, complexity of care, and cost.)
2. Once an elderly individual becomes malnourished, it takes more aggressive nutrition
therapies to bring the nutritional status of the individual up than it does in younger
individuals.8
Studies with older adults have shown that they are less likely to “make up” for
inadequate food and fluid intake at one meal by eating more at later meals. 1
3. The quickest indicator of proper nutritional intake is to monitor percentage of meal
consumption. For the consumption records to be an effective audit tool, they must
accurately reflect actual food intake.
Therefore, an easy to use system which provides consistent accurate results must be
used to be effective and insure proper reimbursement. A study has shown the tray
diagram or pie chart used by some facilities produced unreliable figures.9
One needs to estimate resident food intake in order to identify residents who are not
eating well. 2
10
Monitoring the amount of food left on one’s plate can be a valuable tool to determine
the actual amount of food consumed. Measuring reduced plate waste can help indicate
the acceptability of food items offered and show the actual amount of food consumed,
leading to menu modifications if necessary. 8, 10
4. Observed intake of less than 75% consumed as recorded on Dietary Intake Records
requires more in-depth monitoring or assessment and review by the interdisciplinary
care plan team. Substitutes for items not eaten should be offered when less than 75%
of a meal is consumed.
5. Federal and state regulations may require recording consumptions for specific periods
of time.
G. How to accurately calculate percentage eaten using this method endorsed by
Arkansas CD-HCF. (Copyright 1994 Nancy Storms-Walsh)
1. Count the number of servings on the tray (do not count garnishes, coffee, tea, water,
condiments, milkshakes or canned supplements if they are not part of the planned
menu).
2. Estimate the total servings eaten by adding up the amount eaten of each serving counted. Example: 1/2
meat + 1/4 starchy veg + 0 veg + 3/4 milk + 3/4 fruit +
1/2 bread = 2 3/4 servings eaten.
3. Round total servings eaten down to the nearest 1/2 serving. Example: 2 3/4 servings
rounded down = 2 1/2 servings eaten
4. To change the total number of servings eaten to percentage eaten, you will need to
refer to the “How To Calculate Percentage Eaten” chart or pocket reference cards from
Arkansas CD-HCF. Find the total number of servings eaten (step 3) along the top of the
chart. Locate the total number of servings counted (step 1) along the side of the chart.
The point at which the rows intersect will note the percentage consumed. Example: 2
1/2 servings eaten / 6 total servings counted = 42% eaten.
5. Record the percentage eaten for each resident on the appropriate meal record form.
6. If a milkshake or canned supplement has been included on the meal Tray, but is not
part of the diet as specified on the menu, the percentage consumption must be charted
separately from the rest of the meal consumed. Documentation of snacks and
supplements must always be recorded independent of the meals.
11
H. Commonly asked questions concerning how to calculate percentage eaten using this
method.
1. How does one calculate for double portions of items served? What if the person
calculating the percentage eaten is not aware that they were served double portions?
Answer: One can only calculate the percentage eaten to the best of their knowledge. It
is not a big concern because the double servings if counted for example as 1/2 serving
eaten of 1 item counted or 1 serving eaten of 2 items counted will cause the percentage
to vary only a few percentage points. This is still more accurate than “guessing."
2. What constitutes a “serving” of something?
Answer: A good “rule of thumb” would be to cup your hands together. If the serving
size looks as if it would almost fill your cupped hands (approx. 1/2 cup), it is counted as
a serving. Example: 1 orange slice vs. 1/2 cup orange sections. The pureed consistency
diets would be an exception to this. Example: 1 cup fresh lettuce salad will puree down
to less than 1/4 cup.
3. How do I know if the milkshake or supplement on a resident’s tray is on the menu?
Answer: If a food item is part of the menu, you would see all residents on that same
diet receiving that particular item unless they had a dislike for it. Most facilities do not
include milkshakes or supplements as part of the menu. When in doubt, it is best to ask
the Dietary Manager or Dietitian.
II. Activities
12
Complete these sample exercises to demonstrate the use of the “How to Calculate Percentage
Eaten” chart from the Arkansas CD-HCF. Practice with actual plated samples if possible.
Exercise #1
MEAL
ITEMS ON TRAY
RESIDENT #1
RESIDENT #2
RESIDENT #3
CONSUMED
CONSUMED
CONSUMED
_____________________________________________________________________________________
BREAKFAST ORANGE JUICE
1/2
ALL
NONE
TOAST
NONE
1/2
3/4
EGGS
ALL
NONE
1/2
CEREAL
1/2
ALL
1/2
MILK
3/4
3/4
1/2
COFFEE
ALL
ALL
ALL
STEP 1
Determine the total number of servings to count
for each resident.
___________
___________
___________
STEP 2
Determine the total number of servings eaten for
each resident.
___________
___________
___________
STEP 3
Round the total number of servings eaten down to
the nearest 1/2 serving.
___________
___________
___________
__________%
__________%
__________%
STEP 4
Refer to the chart and find the number of servings
eaten across the top of the chart (step 3) and the total
number of servings counted (step 1) along the side of
the chart.
Determine the percentage eaten where these two
lines intersect.
13
Exercise # 2
MEAL
ITEMS ON TRAY
RESIDENT #1
RESIDENT #2
RESIDENT #3
CONSUMED
CONSUMED
CONSUMED
_____________________________________________________________________________________
LUNCH
MEAT
1/2
ALL
NONE
VEGETABLE
NONE
1/2
3/4
POTATO
ALL
NONE
1/2
BREAD
1/2
ALL
NONE
FRUIT
3/4
3/4
1/2
1/2
1/2
ALL
DESSERT
ALL
ALL
NONE
GARNISH
WATER
1/2
1/2
1/2
COFFEE
ALL
ALL
ALL
SUGAR, CREAMER, SALT, PEPPER
ALL
ALL
ALL
MILKSHAKE (not noted on menu)
1/2
ALL
1/2
STEP 1
Determine the total number of servings to count
for each resident.
___________
___________
___________
STEP 2
Determine the total number of servings eaten for
each resident.
___________
___________
___________
STEP 3
Round the total number of servings eaten down to
the nearest 1/2 serving.
___________
___________
___________
__________%
__________%
__________%
STEP 4
Refer to the chart and find the number of servings
eaten across the top of the chart (step 3) and the total
number of servings counted (step 1) along the side of
the chart.
Determine the percentage eaten where these two
lines intersect.
14
EXERCISE #1 ANSWER KEY---SEE BOTTOM OF PAGE
MEAL
ITEMS ON TRAY
RESIDENT #1
RESIDENT #2
RESIDENT #3
CONSUMED
CONSUMED
CONSUMED
_____________________________________________________________________________________
BREAKFAST ORANGE JUICE
1/2
ALL
NONE
TOAST
NONE
1/2
3/4
ALL
NONE
1/2
EGGS
1/2
ALL
1/2
CEREAL
MILK
3/4
3/4
1/2
COFFEE
ALL
ALL
ALL
STEP 1
Determine the total number of servings to count
for each resident.
____5______
_____5_____
_____5_____
STEP 2
Determine the total number of servings eaten for
each resident.
___2 3/4 ___
____3 1/4 ___
____1 3/4 __
STEP 3
Round the total number of servings eaten down to
the nearest 1/2 serving.
____2 1/2 __
____3______
____1 1/2 __
____50____%
____60____%
____30____%
STEP 4
Refer to the chart and find the number of servings
eaten across the top of the chart (step 3) and the total
number of servings counted (step 1 ) along the side of
the chart.
Determine the percentage eaten where these two
lines intersect.
ANSWER KEY:
STEP 1: Count the following items: orange juice, toast, eggs, cereal, & milk = 5 servings counted
STEP 2: Resident #1 = 1/2 + 0 + 1 + 1/2 + 3/4 = 2 3/4 servings eaten
Resident #2 = 1 + 1/2 + 0 + 1 + 3/4 = 3 1/4 servings eaten
Resident #3 = 0 + 3/4 + 1/2 + 1/2 + 1/2 = 2 1/4 servings eaten
STEP 3: Resident # 1 = 2 1/2 servings eaten (rounded down to the nearest 1/2)
Resident # 2 = 3 servings eaten (rounded down to the nearest 1/2)
Resident # 3 = 2 servings eaten (rounded down to nearest 1/2)
STEP 4: Resident # 1 = 2 1/2 servings eaten out of 5 servings on the tray = 50%
Resident # 2 = 3 servings eaten out of 5 servings on the tray = 60%
Resident # 3 = 2 servings eaten out of 5 servings on the tray = 40%
15
EXERCISE #2 ANSWER KEY----SEE BOTTOM OF PAGE
MEAL
ITEMS ON TRAY
RESIDENT #1
RESIDENT #2
RESIDENT #3
CONSUMED
CONSUMED
CONSUMED
_____________________________________________________________________________________
LUNCH
MEAT
1/2
ALL
NONE
VEGETABLE
NONE
1/2
3/4
POTATO
ALL
NONE
1/2
BREAD
1/2
ALL
NONE
FRUIT
3/4
3/4
1/2
1/2
1/2
ALL
DESSERT
ALL
ALL
NONE
GARNISH
WATER
1/2
1/2
1/2
COFFEE
ALL
ALL
ALL
SUGAR, CREAMER, SALT, PEPPER
ALL
ALL
ALL
MILKSHAKE (not noted on menu)
1/2
ALL
1/2
STEP 1
Determine the total number of servings to count
for each resident.
____6______
____6______
____6______
STEP 2
Determine the total number of servings eaten for
each resident.
____3 1/4 __
____3 3/4 ___
____2 1/2___
STEP 3
Round the total number of servings eaten down to
the nearest 1/2 serving.
____3______
____3 1/2___
____2 1/2___
____50____%
____58____%
____42____%
STEP 4
Refer to the chart and find the number of servings
eaten across the top of the chart (step 3) and the total
number of servings counted (step 1) along the side of
the chart.
Determine the percentage eaten where these two
lines intersect.
ANSWER KEY:
STEP 1: Count the following items: meat, vegetable, potato, bread, fruit, dessert = 6 servings counted
STEP 2: Resident #1 = 1/2 + 0 + 1 + 1/2 + 3/4 + 1/2 = 3 1/4 servings eaten
Resident #2 = 1 + 1/2 + 0 + 1 + 3/4 + 1/2 = 3 3/4 servings eaten
Resident #3 = 0 + 3/4 + 1/2 + 0 + 1/2 + 1 = 2 3/4 servings eaten
STEP 3: Resident # 1 = 3 servings eaten ( rounded down to the nearest 1/2)
Resident # 2 = 3 1/2 servings eaten ( rounded down to the nearest 1/2)
Resident # 3 = 2 1/2 servings eaten ( rounded down to nearest 1/2)
STEP 4: Resident # 1 = 3 servings eaten out of 6 servings on the tray = 50%
Resident # 2 = 3 1/2 servings eaten out of 6 servings on the tray = 58%
Resident # 3 = 2 1/2 servings eaten out of 6 servings on the tray = 42%
16
III. Post Test
1. T_____
F_____ Dietary is the only department which needs to be concerned about
weight loss.
2. T_____
F_____ Weight loss can be related to increased illness and death.
3. T_____
F_____ An individual who loses and gains weight repeatedly will have less
muscle than they did prior to losing weight. (Assuming that resistance
training or weight bearing exercises have not been done.)
4. T_____
F_____ An individual’s nutritional status will not have an impact on their
ability to accomplish their Activities of Daily Living (ADLs).
5. T_____
F_____ The fastest indicator of adequate nutritional intake is percentage
of meal consumption.
6. T_____
F_____ A milkshake or supplement on the meal tray is always counted as
part of the meal.
7. Which of the following food intakes will preserve the greatest amount of muscle with the
loss of weight?
a. Starvation or fasting
b. Mixed food diets less than 1000 Calories
c. Mixed food diets more than 1000 Calories
d. Mixed food diets more than 1000 Calories plus mild exercise
8. The mnemonic MEALS-ON-WHEELS is used to identify some common causes of weight
loss in the elderly. List 5 of these causes.
M ______________
E ______________
A ______________
L ______________
S ______________
O ______________
N ______________
W ______________
H ______________
E ______________
E ______________
L ______________
S ______________
17
III. Post Test
ANSWER KEY
1. T_____
F__X___ Dietary is the only department which needs to be concerned about
weight loss.
2. T__X__
F______ Weight loss can be related to increased illness and death.
3. T__X__
F______ An individual who loses and gains weight repeatedly will have less
muscle than they did prior to losing weight. (Assuming that
resistance training or weight bearing exercises have not been done.)
4. T_____
F__X___ An individual’s nutritional status will not have an impact on their
ability to accomplish their Activities of Daily Living (ADLs).
5. T__X__
F_____ The fastest indicator of adequate nutritional intake is percentage
of meal consumption.
6. T_____
F__X__ A milkshake or supplement on the meal tray is always counted as
part of the meal.
7. Which of the following food intakes will preserve the greatest amount of muscle with the
loss of weight?
a. Starvation or fasting
b. Mixed food diets less than 1000 Calories
c. Mixed food diets more than 1000 Calories
d. Mixed food diets more than 1000 Calories plus mild exercise
8. The mnemonic MEALS-ON-WHEELS is used to identify some common causes of
weight loss in the elderly. List 5 of these causes.
M _edications___
E _motions (depression)
A _norexia, alcoholism
L _ate life paranoia___
S _wallowing problems
O _ral Problems
N _o Money
W _andering_____
H _yper(para)thyroidism,
E _ntry problems
E _ating problems
L _ow-salt, low chol diet
S _hopping problems__
18
References
1. American Dietetic Association. (2002). Position of the American Dietetic Association:
Liberalized diets or older adults in long-term care. Journal of the American Dietetic
Association, 102(9), 1317-1323.
2. Andrews, Y.N., Castellanos, V.H. (2003). Development of a method for estimation of food
and fluid intakes by nursing assistants in long-term care facilities: A pilot study. Journal
of the American Dietetic Association, 103(7), 873-877.
3. Booth, J., Leadbetter, A., Francis, M., Tolson, D. (2005). Implementing a best practice state
ment in nutrition for frail older people: part 1. Nursing older people, 6(10), 26-28.
4. Castellanos, V.H. (2004). Food and nutrition in nursing homes. Food and Nutrition for
Healthier Aging, 65-71.
5. Castellanos, V.H., Andrews, Y.N. (2002). Inherent flaws in a method of estimating meal in
take commonly used in long-term-care facilities. Journal of the American Dietetic
Association, 102(6), 826-830.
6. Chernoff, R. (Ed.). (2006). Geriatric nutrition: The health professional’s handbook (3rd ed.).
Judbury, MA: Jones and Bartlett.
7. Huffman, G.B. (2002). Evaluating and treating unintentional weight loss in the elderly.
American Family Physician, 65(4), 640-650.
8. Kandiah, J. Stinnett, L., Lutton, D. (2006). Visual plate waste in hospitalized patients:
Length of stay and diet order. Journal of the American dietetic Association, 106(10),
1663-1666.
9. Lewko, M., Chamseddin, A., Zaky, M., & Birrer, R. (2003). Weight loss in the elderly:
What’s normal and what’s not. Pharmacy and Therapeutics, 28(11), 734-739.
10. Nichols, P.J., Porter, C., Hammond, L., & Arjmandi, B.H. (2002). Food intake may be
determined by plate waste in a retirement living center. Journal of the American Dietetic
Association, 102(8), 1142-1144.
11. Niedert, K.C., & Dorner, B. (Eds.). (2004). Nutrition care of the older adult: A handbook
for dietetics professionals working throughout the continuum of care (2nd ed.).
Chicago, IL: American Dietetic Association.
19
Arkansas Consulting Dietitians in Health Care Facilities
Project Chart Committee Members & Contributors
Kim Dowell, M.A., R.D., L.D.
Emily Hogue, R.D., L.D.
Jane Long, R.D., L.D., C.F.C.S.
Melissa Shock, PhD, R.D.
Kay Strand, R.D., L.D.
Nancy Storms-Walsh, R.D., L.D.
Marietta Tucker, MEd., R.D., L.D.
Christy Wells, R.D., L. D.
Other Contributors
Margaret Eldred, R.D., L.D.
Beulah Scott, R.D., L.D.
Donald J. Vchulek, CDM, CFPP
2007 Revision Contributors
Melanie Huett, M.S.
Lea Hyland, M.S., R.D., L.D.
Jane Long, R.D., L.D., C.F.C.S.
Nancy Storms-Walsh, R.D., L.D.
2014 How to Calculate Percentage Eaten
All Rights Reserved