Clinical problem of cyanosis - Wk 1-2
advertisement
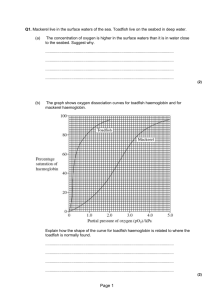
Clinical problem of cyanosis 1.Develop hypotheses to explain the clinical sign of cyanosis Clinical/Physical Sign Cyanosis is a clinical sign characterized by a blue colour of the mucous membranes, nail beds, and skin. It results from the presence of deoxygenated haemoglobin in the blood at a concentration of at least 0.5 g per mL. Cyanosis is usually undetectable until the oxygen saturation of hemoglobin falls below 80% Note: Colour of the Blood Haemoglobin that is fully saturated with oxygen is bright red, while haemoglobin that has lost one or more oxygen molecules (deoxygenated haemoglobin) is darker in appearance. When it has lost most of its oxygen, haemoglobin becomes deep purple in colour. As the blood passes through the tissues it gives up its oxygen and the proportion of deoxygenated haemoglobin increases. CAUSES OF CENTRAL CYANOSIS A Systemic Excess of Deoxygenated Haemoglobin can occur at various stages in the circulation. At the Lungs (Pulmonary) There is a problem with the gas exchange in the lungs and the Oxygen contained within the lung alveoli is not attaching to the Haemoglobin in the blood contained within the lung capillaries. Important note: the clinical sign is an excess of deoxygenated haemoglobin (central cyanosis) but the underlying problem is decreased arterial haemoglobin oxygen saturation At the Heart (Cyanotic Congenital Heart Defects) There is a structural problem with the heart or around the heart in the great vessels that is not allowing the functional distribution of the blood. Basically, somehow the deoxygenated haemoglobin in the systemic venous system is finding its way into the systemic arterial system. Important note: the clinical sign is an excess of deoxygenated haemoglobin (central cyanosis) but the underlying problem is decreased arterial haemoglobin oxygen saturation In the Blood itself 2 forms of haematological problems are associated with central cyanosis. Structural issues with haemoglobin will cause failure to bind oxygen (Methemoglobinaemia). Whilst an excess of RBCs will provide excess unneeded and unused haemoglobin which will be blue/dark purple (Polycythemia) CAUSES OF PERIPHERAL CYANOSIS A Local Excess of Deoxygenated Haemoglobin or Peripheral cyanosis reflects poor perfusion of the peripheries caused by vasoconstriction, reduced cardiac output, or vascular occlusion (It may also be caused by central cyanosis). It may be widespread or may affect only one extremity; however, it doesn’t affect mucous membranes. Typically, peripheral cyanosis appears on exposed areas, such as the fingers, nail beds, feet. Poor Perfusion of the peripheries caused by numerous interrelated factors Low temperatures (Cold Baby) Low cardiac output Shock Sepsis DVT Painted fingernails Eating Blue Lollies 2. Understand the underlying pathophysiology of cyanosis. RESPIRATORY CAUSES (There are more than listed here) Obstruction to the intake of oxygen – Structural (Not enough air can get to the alveoli) Acute Laryngotracheitis Blast Lung Injury Chronic Bronchial Asthma Chronic Bronchitis COPD (Chronic Obstructive Pulmonary Disease) Emphysema Foreign Body (common with children; peanuts) Tension Pneumothorax Decreased oxygen absorption of oxygen – as in conditions with alveolar-capillary block Sarcoidosis Pulmonary Fibrosis Pneumonia Pulmonary Oedema Proteinosis Lung Cancer Decreased Perfusion of the Lung Pulmonary Embolism Pulmonary Vascular Shunts (arteriovenous fistulas) Pulmonary Hemangiomas CARDIOVASCULAR CAUSES Left-to-Right Shunts – Lungs-to-Lungs Shunts – Blood that is returning to the heart from the lungs is recirculated back to the lungs without going to the rest of the body. If the blood was going from the left side of the heart to the right side of the heart then the deoxygenated blood is not getting pumped around the body and there would be no sign of central cyanosis. Therefore L – R shunts are called acyanotic. However, Most of the time there is never a complete Left to right movement of blood and cyanotic symptoms can develop later in life. (cause cyanosis several months or years after birth) Atrial septal defects o ASD is an abnormal opening in the atrial septum that allows communication of blood between the left and right atria. (It is usually asymptomatic until adulthood) Ventricular septal defects o Incomplete closure of the ventricular septum allowing free communication and thus a shunt from L to R ventricles. (It may produce problems from birth or may not be recognized until later in life) (Only about 30% of cases exist in isolation; most present with associated structural defects) Patent or persistent ductus arteriosus (PDA) o PDA results when the ductus arteriosus remains open after birth (the ductus arteriosus is the passage from the pulmonary trunk to the aorta which bypasses the lungs in the foetus) 90% of PDAs occur in isolation.. Atrioventricular septal defects (AVSD) o Abnormal development of the Atrioventricular canal resulting in incomplete closure of the AV septum and inadequate formation of the tricuspid and mitral valves. This can be complete or partial: in the complete form all four cardiac chambers communicate (1/3 of patients with the complete form have Downs Syndrome) Right-to-Left Shunts – Body-to-Body Shunts – Blood that is returning to the heart from the body is recirculated directly back to the body without going to the lungs to be oxygenated. (cause cyanosis early in postnatal life) Tetralogy of Fallot o 1. Ventricular Septal Defect (VSD) o 2. Obstruction to the right ventricular outflow tract (subpulmonary stenosis) o 3. An aorta that overrides the VSD o 4. Right ventricular hypertrophy Transposition of the Great Arteries (TGA) Not Viable without a VSD o Implies ventriculoarterial discordance, such that the aorta arises from the right ventricle and the pulmonary artery arises from the left ventricle. This condition is incompatible with postnatal life unless a shunt exists for adequate mixing of blood (causing cyanosis) Truncus Arteriosus o Normally during embryo development the truncus arteriosus separates to form the aorta and the pulmonary aorta. Thus without this separation blood from the R and L ventricles mixes. Tricuspid Atresia Not Viable without an ASD and VSD Total Anomalous Pulmonary Venous Connection (TAPVC) Not viable without an ASD HAEMOTOLOGICAL CAUSES Polycythemia is an excess of RBCs. This means that when the blood filters through the lung capillaries the normal amount of Haemoglobin picks up the normal amount of oxygen and distributes it: all is good. Except that there is an excess in Deoxygenated Haemoglobin circulating in the blood which are blue/deep purple thus causing Cyanosis. This represents an excess of deoxygenated haemoglobin but not decreased arterial haemoglobin oxygen saturation Methemoglobinaemia occurs when iron exits in the oxidized form (ferric) in greater than 1% of cells. This occurs in congenital and acquired forms (usually due to toxic exposures). Patients with congenital methemoglobinemia are cyanotic, which is primarily of cosmetic importance. It generally follows a benign course. In acquired states, cyanosis reflects acute alteration of tissue oxygen delivery. Methemoglobin has a very high affinity for oxygen and does not deliver oxygen well to tissues. Methemoglobin levels greater than 50% can be rapidly fatal. Central cyanosis may also result from reduced Pao2 at high altitudes. 3. Describe the use of arterial blood gas as a clinical measurement in cyanosis. Hyperoxia Test In general, infants with a cardiac origin for their cyanosis exhibit a worsening of their cyanosis with crying. Administration of 100% oxygen (also known as the Hyperoxia test) can be used as a bedside diagnostic tool to help differentiate between cardiac and pulmonary causes of central cyanosis. This test consists of assessing the rise in arterial oxygenation with the administration of 100% oxygen. The response to 100% oxygen can either be determined by the pulse oximeter or by actually measuring an arterial blood gas. According to one reference, if the patient's oxygen saturation increases by more than 10% or the PaO2 rises by more than 20% to 30%, then the most likely origin for the cyanosis is pulmonary rather than cardiac. If the oxygen saturation does not increase and the cyanosis does not improve with supplemental oxygen, then a cardiac origin for the patient's cyanosis should be suspected. The measured PaO2 in patients with a pulmonary origin for cyanosis should rise well above 200 mm Hg unless the degree of pulmonary disease that is present is severe. PaO2 values that do not rise above 100 mm Hg in cyanotic patients are highly suggestive of a cardiac defect. A PaO2 that remains lower than 100 mm Hg despite 100% oxygen is suggestive of a congenital heart defect with decreased pulmonary blood flow and/or right-to-left shunting. Those congenital heart defects with an increased pulmonary blood flow may exhibit a rise in their PaO2 (up to 150 mm Hg) in response to 100% oxygen. Prolonged administration of 100% oxygen may cause some theoretical problems, such as closing the ductus arteriosus in those infants with critical left heart obstructions or by causing pulmonary vasodilation (which would potentially worsen pulmonary vascular congestion). 4. Outline how arterial blood gas measurements relate to the biochemistry and physiology of gas exchange. ABGs - Normal Values pH PaO2 PaCO2 HCO3- 7.35 – 7.45 80 – 110 36 -44 22 -26 (mmHg) (mmHg) (mmol/L) Gas exchange occurs at two places in the circulatory system: at the lungs and at the tissues Arterial Blood gases are taken from the Systemic Arterial Circulation which is one point of the circuit. The measurement is directly downstream from the gas exchange occurring at the lungs and gives us a good idea of lung function. pH ; H+ indicates if a patient is acidotic (pH < 7.35) or alkalotic (pH > 7.45). PaO2 ; A low O2 indicates that the patient is not respiring (absorbing oxygen into the blood stream) properly. At a PaO2 of less than 60 mm Hg (and a Sa O2 of < 90%) a patient is hypoxaemic and oxygen should be administered. PaCO2 ; The carbon dioxide and partial pressure (PaCO2) indicates a respiratory problem: for a constant metabolic rate, the PaCO2 is determined entirely by ventilation. A high PaCO2 (respiratory acidosis) indicates hypoventilation, a low PaCO2 (respiratory alkalosis) hyperventilation. PaCO2 levels can also become abnormal when the respiratory system is working to compensate for a metabolic issue so as to normalize the blood pH. An elevated PaCO2 level is desired in some disorders associated with respiratory failure; this is known as permissive hypercapnia. HCO3- ; The HCO3- ion indicates whether a metabolic problem is present (such as ketoacidosis). A low HCO3- indicates metabolic acidosis, a high HCO3- indicates metabolic alkalosis. HCO3- levels can also become abnormal when the kidneys are working to compensate for a respiratory issue so as to normalize the blood pH.