Health - LegTrack
advertisement

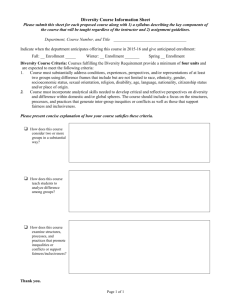
AB 1102 Page 1 Date of Hearing: April 28, 2015 ASSEMBLY COMMITTEE ON HEALTH Rob Bonta, Chair AB 1102 (Santiago) – As Amended March 26, 2015 SUBJECT: Health care coverage: special enrollment periods: triggering event. SUMMARY: Requires a health care service plan (plan) or health insurer (insurer) to allow an individual to enroll in or change an individual plan or policy as a result of pregnancy. EXISTING LAW: 1) Establishes under federal law, the Patient Protection and Affordable Care Act (ACA) which requires that all individuals, with certain exceptions, who have access to affordable coverage purchase minimum essential coverage, as defined, or pay a penalty. 2) Establishes the Knox-Keene Health Care Service Plan Act of 1975 which provides for the licensure and regulation of health care services plans by the Department of Managed Health Care (DMHC) and provides for the regulation of health insurers by the California Insurance Commissioner. 3) Establishes the California Health Benefit Exchange (Exchange), now called Covered California, to arrange for and offer coverage to individuals and small groups, consistent with state and federal requirements, including determining eligibility for federal premium tax credits to assist eligible low- and moderate-income persons with the purchase of health coverage from contracted Covered California health plans and insurers. 4) Requires, under both federal and state law, health plans and insurers issuing health benefit plans in the individual and small group market to comply with specified requirements regarding the offering, sale, and scope of coverage provided, including requirements to cover the following 10 essential health benefits (EHBs): maternity and newborn care; ambulatory patient services; emergency services; hospitalization; mental health and substance use disorder services, including behavioral health treatment; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; preventive and wellness services and chronic disease management; and, pediatric services, including oral and vision care. 5) Requires all plans and insurers to fairly and affirmatively offer, market, and sell all of the health benefit plans that are sold in the individual market to all individuals and dependents in each of the plan’s or insurer’s service areas. 6) Requires plans and insurers to limit enrollment in individual health benefit plans to annual open enrollment periods, and special enrollment periods, as specified. 7) Requires plans and insurers to allow individual health plan subscribers to add dependents to the plan at the option of the subscriber, consistent with open enrollment and special enrollment periods. AB 1102 Page 2 8) Requires plans and insurers to allow an individual to enroll in or change individual health benefit plans as a result of specified triggering events including when the individual: a) Loses minimum essential coverage, as defined; b) Gains a dependent or becomes a dependent; c) Is mandated to be covered as a dependent pursuant to a valid state or federal court order; d) Is released from incarceration; e) Gains access to a new health benefit plan as a result of a permanent move; f) Received services from a contracting provider for specified conditions, and the provider is no longer participating with the plan or insurer; g) Demonstrates to the Exchange that he or she did not enroll in a plan or insurance policy during the immediately preceding open enrollment period because of misinformation that he or she was covered under minimum essential coverage; h) Is a member of the reserve forces of the United States military, or of the California National Guard returning from active duty; or, i) With respect to individual health plans offered through the Exchange, qualifies under specified federal provisions regarding special enrollment periods, changes in eligibility for federal advance premium tax credits. 9) Provides that an individual shall have 60 days from the date of a triggering event to apply for coverage, as specified. 10) Sets forth specified timeframes by which an individual may exercise the right to buy coverage, and for when coverage becomes effective after application for enrollment during annual open and special enrollment periods, including effective dates of coverage in cases of birth, adoption, placement for adoption, marriage, domestic partnership, or loss of minimum essential coverage. 11) Prohibits plans and insurers from basing eligibility for coverage on specified factors, including health status or medical condition, and prohibits plans or insurers from requiring applicants for coverage, or any dependents, from completing a health assessment or medical questionnaire, or from acquiring or requesting information that relates to a health statusrelated factor prior to enrollment. FISCAL EFFECT: This bill has not yet been analyzed by a fiscal committee. COMMENTS: 1) PURPOSE OF THIS BILL. According to the author, maternity care is an EHB under the ACA, and special enrollment exists for women who give birth. The author states, because of this, it makes sense to ensure that access to prenatal care is granted. The author contends AB 1102 Page 3 that, if pregnancy qualifies as a triggering event, women will be afforded the opportunity of important preventive measures that, in the long run, would save lives and the health care system money. 2) BACKGROUND. a) Open enrollment and special enrollment periods. Under the ACA, individuals are required to maintain health insurance or pay a penalty, with exceptions for financial hardship, religion, incarceration, and immigration status. Individuals who do not meet these requirements may be subject to a penalty when filing their federal income tax return. Effective January 1, 2015, the penalty is the greater of $325 or 2% of income. The ACA also includes several insurance market reforms, such as prohibitions against health insurers imposing preexisting health condition exclusions and a requirement that health plans and insurers offer EHBs in the individual and small group markets. The ACA requires the U.S. Secretary of Health and Human Services (HHS) to establish open enrollment periods for health plans sold through state health benefits exchanges, and requires individual market plans sold outside an exchange to be offered during this open enrollment period as well. Open enrollment serves as a safeguard against people waiting to become sick to enroll. People will generally be unable to enroll in individual coverage outside of the open enrollment period unless they experience a qualifying life event, which triggers a special enrollment opportunity. Such events include loss of eligibility for other coverage, gaining a dependent, divorce, or a large change in income. Under current state or federal law, none of the qualifying life events triggering a special enrollment period are based on changes in health status. The open enrollment period for this year was November 15, 2014 to February 15, 2015. According to recently released federal regulations, for 2016, the open enrollment period will run from November 1, 2016 to January 31, 2016. Additionally, a special open enrollment period was authorized by the federal government, and implemented by Covered California, for individuals who were unaware of the tax penalty for failing to maintain health insurance. The special enrollment period runs from February 15, 2015 to April 30, 2015. b) California Health Benefits Review Program (CHBRP) analysis. On April 23, 2015, CHBRP published an analysis of this bill. According to CHBRP, there appear to be two populations of pregnant women affected by this bill: those who are already insured with maternity benefits, and those who are uninsured at the time of conception. It should also be noted that these women would also most likely be of midrange to higher incomes considering the existing public program coverage options for women of lower incomes. CHBRP’s analysis focused on the bill’s impact to Covered California, noting that 21.7% of Covered California enrollees are women of childbearing age. In terms of utilization and cost, CHBRP estimated the impact to Covered California expenditures if 10% and 25% of women dropped coverage as a result of this bill. Specifically, CHBRP found that if 10% of women dropped coverage, and later added coverage after becoming pregnant, Covered California would experience an increase in premiums of 0.4% amounting to AB 1102 Page 4 $22.8 million. If 25% of women took the same actions, premiums would increase by 1.2% or $75.8 million. CHBRP also estimated that 3.6% of women aged 19 to 44 become pregnant each year, and about a quarter of those with higher incomes would be expected to temporarily add coverage for maternity and childbirth expenses. CHBRP estimated that 489 women would newly enroll in Covered California, generating a net cost impact of approximately $5,822,339. According to CHBRP, this group of women would also propel somewhat of an increase in utilization of prenatal care services once their new insurance is activated. CHBRP also considered the potential for insured women to, upon pregnancy, change from a more affordable plan with a limited network, to a more expensive plan with a broader network selection. CHBRP was unable to perform a complete projection of the impact of this scenario, but stated that it would likely be of smaller magnitude than that of women dropping and later re-enrolling upon pregnancy, or of uninsured women seeking coverage upon pregnancy. The CHBRP analysis notes disparities among insured and uninsured women with regard to prenatal care. Specifically, about 94% of privately insured women initiated prenatal care in their first trimester as compared to 61% of uninsured women. Additionally, CHBRP noted that the annual societal economic burden associated with preterm births is an average of $51,600 per infant born preterm. A pregnancy and non-complicated birth costs approximately $18,690 in California. In California, 10.1% of babies are born prematurely, and CHBRP notes that, to the extent that this bill could increase utilization of effective prenatal care that can reduce outcomes such as preterm births and related infant mortality, there is a potential to reduce morbidity and mortality and associated societal costs. Finally, CHBRP's review of medical effectiveness of this bill focuses on prenatal care, due to the fact that this bill could increase the number of pregnant women with health insurance, and, thus reduce-out-of-pocket expenses for prenatal care. CHBRP states that reducing out-of-pocket costs could, in turn increase pregnant women's use of prenatal care. CHBRP states that there is clear and convincing evidence that certain prenatal care services produce better outcomes for mothers and infants. c) Recent federal correspondence. At the federal level, the U.S. Department of HHS is being urged by advocates and lawmakers to add pregnancy as a qualifying life event for a special enrollment period outside of open enrollment. In March 2015, 37 U.S. Senators sent a letter to HHS Secretary Sylvia Mathews Burwell, encouraging her to institute a special open enrollment period for women to enroll in health coverage when they find out they are pregnant. In the letter, the Senators asserted, among other things, that if a woman becomes pregnant at a time outside of the open enrollment period and is uninsured, or enrolled in a grandfathered plan that does not cover maternity services, then she will not be able to access coverage for maternity care, forcing them to either forgo critical care or face significant out-of-pocket costs. On April 10, 2015, Secretary Burwell responded in a letter stating that, after reviewing federal statute and regulations, HHS does not have the legal authority to establish pregnancy as an exceptional circumstance. Secretary Burwell also added that, under the AB 1102 Page 5 ACA, all non-grandfathered individual and small group plans, including those sold through an Exchange, must cover maternity services, and women cannot be discriminated against on the basis of gender or pre-existing conditions when purchasing health insurance through an Exchange. Additionally, Secretary Burwell noted that the federal Medicaid and Children's Health Insurance Program provide access to coverage for pregnant women who can enroll in these programs anytime if they qualify. In March 2015, U.S. Senators Barbara Boxer and Dianne Feinstein sent a letter urging Covered California to add pregnancy as a qualifier for special enrollment through Covered California. The Senators stated that prenatal care "is critical for ensuring a healthy pregnancy and positive outcomes for both the baby and the mother. Especially since having a child is a qualifying life event, it makes sense to ensure that access to care is granted prior to birth." The Senators also stated that, "allowing women to purchase health insurance during pregnancy will increase access to care and has the potential to improve health, save lives, and reduce future health costs." On April 15, 2015, Covered California issued a response to this letter stating that, "absent HHS guidelines, Covered California is unable to even consider making pregnancy a qualifying life event that would trigger a special enrollment period in the California Health Benefit Exchange." The letter also stated that, moving forward, Covered California will continue to "stress the importance of making sure that all consumers, regardless of health status, understand the benefits of enrolling during the Open Enrollment period as well as potential tax penalties for not having coverage through the year." d) Public coverage programs. Currently, women with qualifying low-income who become pregnant can apply for Medi-Cal at any time during the year as Medi-Cal does not subject applicants to an open enrollment period. Pregnant women may also apply through their provider for Medi-Cal Presumptive Eligibility (PE) for pregnant women, a program that provides immediate no-cost pregnancy-related care to low-income women pregnant women while their application is evaluated for ongoing Medi-Cal. PE for pregnant women offers coverage for specific ambulatory, pregnancy-related care, some lab tests, and prescription drugs for pregnancy-related conditions. PE for pregnant women is a temporary program, and a pregnant woman may apply for Medi-Cal on an ongoing basis during the PE period. Additionally, the Medi-Cal Access Program (MCAP), formerly known as the Access for Infants and Mothers Program, provides low-cost affordable health coverage for middleincome pregnant women, specifically those with income too high for no-cost Medi-Cal, but at or below 400% of the federal poverty level. MCAP coverage costs 1.5% of an enrollee's adjusted net-annual income and is billed over a 12-month period. MCAP provides coverage for pregnant women who are not eligible for no-cost Medi-Cal, as specified, and who do not have health insurance, or have private insurance with a maternity-only deductible or co-payment greater than $500. 3) SUPPORT. Supporters state that half of all pregnancies are unintended, which means that if a pregnant woman is uninsured at the time of pregnancy and does not have employer-based coverage or does not qualify for Medi-Cal or MCAP, she will not have any coverage options until after the child is born. Supporters assert that without prenatal care, expectant parents AB 1102 Page 6 are far more likely to lack diagnosis and treatment of serious, even life-threatening complications during and after pregnancy, and are more likely to have a pre-term delivery. Supporters state that preterm birth is the leading cause of infant death, developmental disabilities, and imposes significant costs to the health care system. Supporters further argue that the ACA implemented several changes which would mitigate the potential consequences of adverse selection that opponents of this bill argue, including individual mandate requirements, massive coverage expansions, and the requirement for maternity care to be covered as an EHB. Supporters conclude by stating that this bill would help bridge a narrow, but significant gap in access by extending coverage to uninsured women at a time when it most makes sense. 4) OPPOSITION. Opponents state that annual open enrollment periods are designed to provide a period of open access into any health plan of an enrollee's choice, while protecting against individuals waiting to enroll until they need health care. Opponents argue that special enrollment periods allow individuals to enroll outside of this annual open enrollment period, but only for narrow, qualifying events in a person's life, such as the loss of coverage through divorce. Opponents state that adding additional special enrollment periods not intended by the ACA potentially drives up the cost of health care and provides disincentives for individuals to enroll under the normal timeframe. 5) RELATED LEGISLATION. SB 125 (Ed Hernandez) establishes an annual open enrollment period for purchasers in the individual health insurance market for the policy year beginning on January 1, 2016, from November 1, of the preceding calendar year, to January 31, of the benefit year, inclusive; extends the sunset date of CHBRP to June 30, 2017. 6) PREVIOUS LEGISLATION. a) SB 20 (Ed Hernandez), Chapter 24, Statutes of 2014, requires a plan or insurer to provide annual enrollment periods for policy years beginning on or after January 1, 2016, from October 15 to December 7, inclusive, of the preceding calendar year. b) SB X1 2 (Hernandez), Chapter 2, Statutes of 2013-14 First Extraordinary Session, applied the individual insurance market reforms of the ACA to health plans regulated by DMHC and updates the small group market laws for health plans to be consistent with final federal regulations. c) AB X1 2 (Pan), Chapter 1, Statutes of 2013-14 First Extraordinary Session, established health insurance market reforms contained in the ACA specific to individual purchasers, such as prohibiting insurers from denying coverage based on pre-existing conditions and makes conforming changes to small employer health insurance laws resulting from final federal regulations. d) SB 900 (Alquist), Chapter 659, Statutes of 2010, and AB 1602 (Perez), Chapter 655, Statutes of 2010, established the Exchange. e) AB 1180 (Pan), Chapter 441, Statutes of 2013, made inoperative several provisions in existing law that implement the health insurance laws of the federal Health Insurance Portability and Accountability Act of 1996 and additional provisions that provide former employees rights to convert their group health insurance coverage to individual market AB 1102 Page 7 coverage without medical underwriting. Established notification requirements informing individuals affected by AB 1180 of health insurance available in 2014. f) SB X1 2 (Hernandez), Chapter 2, Statutes of 2013-14 First Extraordinary Session, and AB X1 2 (Pan), Chapter 1, Statutes of 2013-14 First Extraordinary Session, conform California law to the ACA as it relates to the ability to sell and purchase individual health insurance by prohibiting pre-existing condition exclusions, establishing modified community rating, requiring the guaranteed issue and renewal of health insurance, and ending the practice of carriers conditioning health insurance on health status, medical condition, claims experience, genetic information, or other factors. The bills also update the small group market laws for health plans to be consistent with final federal regulations. g) AB 1602 (John A. Pérez), Chapter 655, Statutes of 2010, and SB 900 (Alquist), Chapter 659, Statutes of 2010, establish the Exchange and its powers and duties. h) AB 1996 (Thomson), Chapter 795, Statutes of 2002, requests the University of California (which created CHBRP in response), until January 1, 2007, to, within 60 days of receiving a request by the Legislature, review legislation proposing to mandate or repeal a health plan or health insurance benefit or service for public health, medical, and financial impacts. 7) POLICY COMMENT. The goal of this bill is well intended. As CHBRP stated in its analysis, there is clear and convincing evidence that certain prenatal care services produce better birth outcomes. Thus, this bill could very well have a positive public health impact and reduced costs over time as a result in improved health outcomes for pregnant women and their infants. However, the bill also raises important policy questions about the introduction of triggering events based on health-conditions. While California law has exceeded federal law by adding our own qualifying events for special enrollment such as being released from incarceration, or returning from active military duty, none of the current qualifying events in state or federal law are based on a change in health status. Other policy questions to consider are what kind of impact the bill may have on the insurance market in terms of possible disincentives to maintain coverage pursuant to the individual mandate, and potential adverse selection. Should this bill move forward, the author should consider the potential impact of this bill on the individual market as a whole, and continue to seek additional data and information to determine to what degree the benefits of increased access to coverage for prenatal care or other health care services for pregnant women would offset the potential for adverse selection and accompanying increases in costs to the individual marketplace. Finally, as stated in the analysis, women with incomes below 400% of the federal poverty limit may obtain free or low-cost coverage through Medi-Cal or the Medi-Cal Access Program when they become pregnant. As such, this bill would essentially apply to women of relatively higher financial means, those with incomes above 400% of the federal poverty limit. AB 1102 Page 8 REGISTERED SUPPORT / OPPOSITION: Support Maternal and Child Health Access Western Center on Law and Poverty SEIU California Opposition Association of California Life and Health Insurance Companies California Association of Health Plans Analysis Prepared by: Kelly Green / HEALTH / (916) 319-2097