- Advanced Paediatric Emergency Medicine course

Applies to:
Emergency service medical officers and nursing staff
Approved:
Director of Emergency
Medicine, Logan Hospital
Replaces:
New document
Due for Review:
February, 2014
Related Links:
Nil
QUEENSLAND HEALTH
METRO SOUTH HEALTH SERVICE DISTRICT
Logan and Beaudesert Hospitals
Procedure Title:
High-flow nasal prong therapy —infants and children up to 4 years of age
Emergency service, Logan Hospital
PURPOSE
To enable the safe administration of high-flow nasal prong (HFNP) therapy by emergency service medical officers and registered nurses.
DEFINITIONS
CEWT —clinical early warning tool
CO
2
—carbon dioxide
CPAP —continuous positive airway pressure
ED
—emergency department
FiO
2
—frequency of inspired oxygen
H
2
O —water
HFNP
—high-flow nasal prong
HR —heart rate
LH —Logan Hospital
MCH —Mater Children's Hospital
NIV —non invasive ventilation
O
2
—oxygen
PEEP —positive end expiratory pressure
RCH —Mater Children's Hospital
RR —respiratory rate
RSQ —Retrieval Services Queensland
For the management of infants and children up to 4 years of age requiring HFNP therapy, the emergency department (ED) Logan
Hospital (LH) endorses the use of the workplace guideline ' Oxygen therapy: application of nasal humidified oxygen via fisher and paykel humidifier infant, small child ' by Gold Coast Health Service District.
1 The procedure section of this document has been adapted from this guideline.
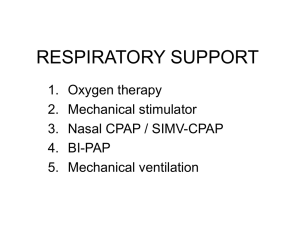
INTRODUCTION
Respiratory distress in infants and young children is a common lifethreatening presentation to emergency services within Australia. It is usually treated with various forms of non-invasive respiratory therapies to improve oxygenation and decrease the work of breathing, including oxygen (O
2
) therapy and continuous positive airway pressure (CPAP).
2
High-flow nasal prong therapy refers to the delivery of air and oxygen via a humidified circuit at a high flow via nasal prongs.
3 The exact mechanism of how it works is still unclear, but research has identified a number of advantages over other forms of O
2
therapy. These
Printed Versions are Uncontrolled 1/6
PROCEDURE <AAA0000> : <Procedure Title> include: 4,5,6
humidification of inspired gas mixture to reduce damage to the upper airway mucosa the high flow washes out the nasopharyngeal anatomical dead space of expired carbon dioxide
(CO
2
) in exchange for oxygen-enriched gas inspired oxygen concentration (FiO
2
) can be titrated according to patient’s needs work of breathing and respiratory rate are decreased
it is better tolerated
nutrition, oral hygiene and communication can be maintained without interrupting oxygen delivery
potentially, positive end expiratory pressure (PEEP) can be delivered (up to 5 cmH
2
O).
Indications for using HFNP therapy include respiratory diseases with documented hypoxemia, such as: 2
bronchiolitis asthma
pneumonia.
Contraindications include: nasal obstruction, e.g. choanal atresia, large polyps
children requiring intubation for airway protection, e.g. reduced conscious level life threatening hypoxia children with hypotension and cardiac arrhythmias foreign body aspiration ingestion and toxins.
—HFNP therapy is not a replacement for intubation and ventilation
EQUIPMENT REQUIRED
Oxygen blender
Flow meter
—0 to 15 L/min
Fisher and Paykel humidifier base
Temperature sensing probe
Temperature heating cable
Breathing circuit
—Paediatric RT329
Nasal prongs sized to fit patient —infant, intermediate infant, paediatric
PROCEDURE
1. Assemble the circuit
2. Set the flow rate
The ED staff specialist or senior medical officer is responsible for determining and documenting the flow rate required.
Generally at the commencement of HFNP therapy set the flow rate at 7-8 L/min and then wean at the discretion of the medical staff, most commonly down to 6 or 4 L/min.
Printed Versions are Uncontrolled Due for Review: <DD-MM-YYYY> 2/6
PROCEDURE <AAA0000> : <Procedure Title>
A precise flow rate cannot be determined for each infant or child. Setting a safe flow rate is estimated based on the following principles:
Size —a larger child will have a higher tidal volume and therefore will require a higher flow rate to meet inspiratory demand
Work of breathing —during respiratory distress, the respiratory rate increases and the inspiratory time becomes shorter. This means that the child must inhale at a faster rate, therefore the flow rate has to be increased to meet the child's inspiratory demand.
Alternatively, use the following formula as a guide 7
Flow (L/min) = 0.92 + 0.68
x ( x = weight in kg)
Turn the flow control on the 0-15 L/min flow meter to commence gas flow through the circuit
(Figure 1).
Figure 1: Flow rate and oxygen blender
Source: Gold Coast Health Service District 1
ALERT: HFNP therapy nasal prongs
3. Set the FiO
2
The nasal prongs limit the amount of flow, i.e. intermediate prongs will not deliver more than 7 L/min and paediatric prongs 8 L/min.
The ED staff specialist or senior medical officer is responsible for determining and documenting the FiO
2
required and the target O
2
saturation range.
Turn the knob on the oxygen blender to set the FiO
2
to a level that will maintain optimum oxygenation (Figure 1). It is reasonable to start with an FiO
2 of 100%.
Titrate the FiO
2
to achieve the target O
2
saturation range (usually greater than 93%).
4. Connecting HFNP therapy to the infant or child
Place the infant or child in a position of comfort.
Feel the outside of the breathing circuit and check the humidifier temperature to ensure that it is warmed to body temperature (37 o C) before connecting the circuit. If the gas flow is not warm, the infant or child will not tolerate the HFNP therapy and this may result in anxiety.
Cut lengths of comfeel and hypafix to size (Figure 2).
Apply the comfeel to the infant or child ’s face (Figure 3).
Position the prongs in the nose and fix in place with hypafix. Ensure that the nasal prongs do not occupy more than 50% of each nare (Figure 4).
Printed Versions are Uncontrolled Due for Review: <DD-MM-YYYY> 3/6
PROCEDURE <AAA0000> : <Procedure Title>
Connect the nasal prongs to the breathing circuit (Figure 5).
Do not lay the breathing circuit on the infant's or child's skin. Place a blanket or towel under the circuit to insulate them from the heat.
Inform the child and visitors not to touch the humidifier plate due to risk of burns.
Figures 2 to 5: Connecting nasal prongs to a patient
Source: Gold Coast Health Service District 1
5. Monitoring response to therapy
Review the respiratory rate (RR), work of breathing and O
2
saturations during the first few minutes of treatment.
Evaluate the need to increase the flow rate (if not at the maximum already) if the infant's or child's work of breathing is high and their oxygen saturations are not improving.
A venous blood gas may be useful to help guide therapy at commencement of HFNP therapy and 30 minutes later to assess response.
When the infant or child is stable, wean the FiO
2 first, then the flow rate.
Turn the FiO
2 down by 0.10 (10%) every 5-10 mins to < 40%, provided the O
2
saturations are maintained within the target range.
Decrease the flow rate by 1 L/min increments, titrated to the infant's or child's response and condition, to a minimum of 4 L/min.
When the flow rate is reduced to 4 L/min and FiO
2 is < 40%, consider humidified low flow nasal prong oxygen OR dry flow nasal prong oxygen via a low flow meter and regular nasal prongs.
The medical staff are responsible for titrating and weaning HFNP therapy settings.
ALERT: Failure criteria
Printed Versions are Uncontrolled
Infants or children still working hard to breath or failing to oxygenate despite flows of 2 L/kg/min and FiO
2
100% will need an increased level of support with NIV or intubation and ventilation. RSQ should be contacted for advice.
Infants less than 3 months of age requiring a flow of more than 5 L/min and
FiO
2
100% require a careful assessment by the attending consultant to assess if the they are approaching failure of treatment. If their respiratory status is not improving or deteriorating, LH paediatric team and RSQ should be contacted for advice
Any infant or child greater than 3 months of age requiring a flow of 8 L/min and FiO
2
100% should be closely observed for signs of respiratory failure.
If their respiratory status is not improving or deteriorating, LH paediatric team and RSQ should be contacted for advice.
Due for Review: <DD-MM-YYYY> 4/6
PROCEDURE <AAA0000> : <Procedure Title>
6.
Nursing care
These infants and children are unwell and should be managed in a high acuity area.
Continuous heart rate (HR) and O
2
saturation monitoring is required.
1 hourly documentation of a full set of vital signs/observations on the ED CEWT tool and CEWT score.
1 hour documentation of humidifier temperature, FiO
2 and flow rate.
1 hourly observations of circuit, water level, and nasal prong position.
It is important to check nasal prong position as dislodgement will result in a loss of respiratory support.
If clinical condition deteriorates the infant or child should be assessed for consideration of escalation in respiratory support, e.g. NIV or intubation and ventilation.
The medical staff are responsible for titrating and weaning HFNP therapy settings.
Nasal hygiene and suctioning as required.
Documentation —note the following in the clinical notes: o date the circuit was assembled o time HFNP therapy was commenced and ceased o target O
2
saturation range o response to treatment.
Disposition 8.
Infants and children requiring HFNP therapy will require admission to hospital. The response to therapy, current condition and associated co-morbidities will determine whether the child is admitted to the paediatric ward at LH (ward 2F) or retrieved to MCH or RCH. Discussion with the attending ED staff specialist and paediatrician will help determine disposition.
If a retrieval is required phone RSQ on 1300 799 127.
When a decision is made to transfer a child to a Level 6 facility, referral must be made through RSQ.
8 http://qheps.health.qld.gov.au/rts/docs/rsq_activation.pdf
Further information on the preparation of a infant prior to transport can be obtained through RSQ Clinical
Guidelines paediatric section (page 31-35).
8 http://qheps.health.qld.gov.au/rts/docs/clin_guide_pt2.pdf
Printed Versions are Uncontrolled Due for Review: <DD-MM-YYYY> 5/6
PROCEDURE <AAA0000> : <Procedure Title>
Secondary Document Information
References
Author
Stakeholders Consulted
1. Gold Coast Health Service District. Oxygen therapy: Application of nasal humidified oxygen via fisher and paykel humidifier infant, small children.
Australia: Gold Coast Health Service District. 2010.
2. Schibler A., Pham TMT., Dunster KR., et al. Reduced intubation rates for infants after introduction of high-flow nasal prong oxygen delivery. Intensive
Care Medicine. 2011; 37 (5): 847-852.
3. Groves N., Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Australian Critical Care. 2007; 20 (4): 126-131.
4. Kernick J., Margarey J. What is the evidence for the use of high flow nasal cannula oxygen in adult patients admitted to critical care units? A systematic review. Australian Critical Care. 2010; 23 (2): 53-70.
5. McKiernan C., Chua LC., Visintainer PF., et al. High flow nasal cannulae therapy in infants with bronchiolitis. The Journal of Pediatrics. 2010; 156 (4):
634-638.
6. Dysart K., Miller TL., Wolfson MR., et al. Research in high flow therapy:
Mechanisms of action. Respiratory Medicine. 2009; 103 (10): 1400-1405.
7. Campbell DM., Shah PS., Shah V., et al. Nasal continuous positive airway pressure from high flow cannula versus infant flow for preterm infants. Journal of Perinatology. 2006; 26 (9): 546-549.
8. Statewide Clinical Coordination and Retrieval Services. Clinical guidelines:
Section two [intranet]. Brisbane (AU): Queensland Government (Queensland
Health); 2008 [cited July 25]. Available from: http://qheps.health.qld.gov.au/rts/docs/clin_guide_pt2.pdf
Clinical Nurse Consultant (Paediatrics) —Emergency service, Logan Hospital
Date Endorsed
DD-MM-YYYY
Version Change History
V#
1 New document
Amendments
Approved
Date Position
23/01/2012 CNC (Paediatrics) )
—
Emergency service,
Logan Hospital
Printed Versions are Uncontrolled Due for Review: <DD-MM-YYYY> 6/6