Predicting Nonlinear Pharmacokinetics of Omeprazole Enantiomers
advertisement
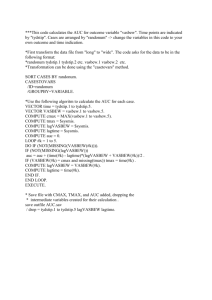
Predicting Nonlinear Pharmacokinetics of Omeprazole Enantiomers and Racemic Drug Using Physiologically Based Pharmacokinetic Modeling and Simulation: Application to Predict Drug/Genetic Interactions Fang Wu1, Lu Gaohua2, Ping Zhao1, Masoud Jamei2, Shiew-Mei Huang1, Edward D Bashaw1, Sue-Chih Lee*1 1. Office of Clinical Pharmacology, Office of Translational Sciences, Center for Drug Evaluation and Research, Food and Drug Administration, Silver Spring, MD 20993 USA 2. Simcyp Limited, Blades Enterprise Centre, John Street, Sheffield, UK Running title: PBPK model predicting nonlinear PK of omeprazole *Corresponding author Sue-Chih Lee, Ph.D. Office of Clinical Pharmacology Office of Translational Sciences Center for Drug Evaluation and Research Food and Drug Administration 10903 New Hampshire Ave Building 51, Room 2142 Silver Spring, MD 20993 Tel: 301-796-1563 Fax: 301-847-8719 Email: suechih.lee@fda.hhs.gov Disclaimer: The views presented in this manuscript are those of authors and do not necessarily reflect the official view of the FDA. 1 SUPPLEMENTARY METHODS 1. Modification of initial PBPK model of esomeprazole by integrating timedependent CYP2C19 inhibition V .Enz (t ) max, H ,2C19 H , 2C19 CLu (t ) CLu int, H int, H ,3 A4 C fup Liver K . mu,2C19 BP Kp / BP Liver V .Enz (t ) max, G,2C19 G, 2C19 CLu (t ) CLu int, G int, G,3 A4 K fu .C mu,2C19 Gut PV (1) (2) Where CLuint,H(t) and CLuint,G(t) are the time variant intrinsic metabolic clearances of esomeprazole in the whole liver and gut, respectively; Vmax,H,2C19 and Vmax,G,2C19 are the maximum metabolic reaction velocities for CYP2C19- and CYP3A4-mediated metabolism of esomeprazole in the whole liver and gut, respectively; Kmu,2C19 is the Michaelis-Menten constant (corrected for non-specific binding) for CYP2C19-mediated metabolism of esomeprazole; CLuint,H,3A4 and CLuint,G,3A4 are the whole liver and gut intrinsic metabolic clearances by CYP3A4-mediated metabolism of esomeprazole, respectively. fup is the fraction unbound in plasma, fuGut is the fraction unbound in enterocyte, KpLiver is the liver to plasma concentration ratio, BP is the blood to plasma concentration ratio, CLiver is the liver concentration and CPV is the portal vein concentration of esomeprazole. Enz(t) signifies the level of relevant active enzyme at the site of metabolism which are calculated as described in the literature (1). 2 Initial model (Model E1) during the first round of model development has a fixed CLuint,2C19 value of (16.2 L/min/pmol of isoform) at enzyme level obtained from the back calculation using retrograde function based on the i.v. clearance after single dose of IV infusion of 20 mg esomeprazole. While in Model E2 during second round of model development, because of TDI, the intrinsic clearance may be more than the fixed value used in Model E1. To determine the possible higher CYP2C19 metabolism expected from the observed nonlinear PK at 20 mg to 40 mg i.v., the value of CLu,int,2C19 was manually increased to 150% or 200% of the initial value. At the same time, kinact and KI values were estimated based on the literature data (2) using sensitivity analysis, which was conducted to assess the effect of a range of kinact (1-10/h) and KI (0.1-1 μM) on the AUC and Cmax values after single i.v. dosing of two doses (20 and 40 mg q.d.) of esomeprazole. For the second round of model development, model E2-1 was selected based on the best matching of the predicted parameters with the observed values as shown in supplementary Table S1. Furthermore, because of the TDI effect of esomeprazole on CYP2C19, the original fm describing metabolism contribution by different enzymes may not be concrete. The CLuint, 2C19 may be larger than the value that was back-calculated from retrograde function of SimCYP. Similarly, CLuint,3A4 could be less than the back-calculated value. Thus, for the third round of model development (E3 round), we used the CLuint,2C19 with 150% or 200% of the initial value and decrease the CLuint,3A4 to 60% and 40% of the initial value. 3 Model E3-II with CLuint,2C19 of 24.3 and CLuint,3A4 of 0.36 μL/min/pmol of P450 was selected as the “best” model during the third round because using Model E3-II can get a good prediction for esomeprazole PK data after i.v. administration, indicating these intrinsic clearance values for CYP2C19 and CYP3A4 are plausible. Therefore, these values were also used in Model E3-II for esomeprazole after p.o. administration. The KI and kinact obtained from IV data analysis were verified by comparing the predicted AUC and Cmax to the observed values for each dose after single and multiple p.o. administration. If there was any discrepancy, sensitivity analysis was performed to assess the effect of kinact (1-10/h) and KI (0.1-1 μM) on AUC96-120 for 20 mg and 40 mg dosing (q.d., 5 days) and on AUC144-168 for 15 mg (q.d., 7 days). Also KI and kinact were adjusted by sensitivity analysis on i.v. data until reaching a compatible value for the p.o. data analysis, which is similar to a simultaneous fitting process to get estimation for K I and kinact. 2. Modification of R-omeprazole PBPK model by integrating CYP2C19 inhibition mechanisms Based on the observed evidence of decreased clearance when multiple doses (40 mg) were given (3), a TDI may exist. To account for higher CYP2C19 metabolism expected from the observed nonlinear PK at 15 mg p.o. compared to 40 mg p.o., auto competitive inhibition and time dependent inhibition effects on the CYP2C19 are taken into account to develop Model R2. The value of CLu,int,2C19 was varied in a range of 100-140% of the 4 initial value in the sensitivity analyses for KI and kinact. The ki value was obtained from literature (2), estimated as IC50/2. At each CLu,int,2C19 level, KI and kinact values were obtained by doing sensitivity analysis conducted to assess the effect of a range of KI (0.3-3 μM) and kinact (2-20/h) on the AUC and Cmax values after 5 days dosing of two doses (20 and 40 mg q.d.) and 7 days dosing of 15 mg q.d. of R-omeprazole. Optimized combination of CLu,int,2C19,, KI and kinact were obtained and incorporated in Model R2, based on the similarity of predicted AUC and Cmax to the observed values for each dose. Both Model R1 and Model R2 were qualified by visually comparing simulated R-omeprazole plasma PK profiles with those from clinical studies (3;4) and the similarities of PK parameters such as AUC, Cmax and clearance/F between the simulated and observed results. 3. Differential equations used in the PBPK model Differential equations describing the kinetics of esomeprazole or R-omeprazole in the PBPK model were shown as follows: dCPV 1 [QPV C sys Q PV C PV f a ka FG (t ) D POk a t ] dt VPV fu dCliver 1 C [QPV C PV Q HA C sys (QPV QHA p CLuint,H (t ) ) liver ] Kpliver dt Vliver BP BP 5 (3) (4) dCsys dt 1 C CL [(QPV Q HA ) liver (QPV Q HA ) C sys R C sys DIV ] Kp Vsys BP liver BP (5) Where CPV, Cliver and Csys are the concentrations of drug in the portal vein, systemic circulation and liver, respectively; VPV and Vliver are the volumes of portal vein blood and of the liver, respectively; Vsys is the volume of distribution of drug (substrate/inhibitor) in the blood; QPV and QHA are the blood flows in the portal vein and hepatic artery, respectively; fup is the unbound fraction in plasma, BP is the blood to plasma concentration ratio of the drug (CB/CP)); fa is the fraction of drug absorbed into the enterocytes; ka is the first-order absorption rate constant of the drug; FG is the intestinal availability of the drug; CLR is the renal clearance of the drug from plasma; Kpliver is the partition coefficient of liver over plasma; Dpo and DIV are the orally and intravenously administered dose of the drug; CLu,int,H(t) is the time-variant intrinsic metabolic clearance of the drug in the liver. 4. Enzymes dynamics and inhibition When both competitive and TDI mechanism were incorporated in the model O to simulate the mutual and auto-inhibitory effects of both R-omeprazole and esomeprazole on the hepatic and intestinal metabolism, the CLu,int,G(t) and CLu,int,H(t) in the PBPK models incorporating TDI were refined by the following equations: FG (t ) Qgut (6) Qgut fugut CLuint,G (t ) CLuint,G (t ) CLuint,2C19 Amt gut 2C19(t ) Actgut 2C19 (t ) CLuint,3 A4 Amt gut3 A4 Actgut3 A4 6 (7) dAmtgut 2C19 kinact kdeg, gut 2C19 Amt 0, gut 2C19 Amtgut 2C19 kdeg, gut 2C19 fu K dt 1 mic I fu gut I PV 1 Actgut 2C19 fugut I PV 1 fumic ( I ) ki FH (t ) QH QH fub CLuint,H (t ) (8) (9) (10) CLuint,H (t ) CLuint,2C19 Amtliver 2C19(t ) Actliver 2C19 (t ) CLuint,3 A4 Amtliver3 A4 Actliver3 A4 (11) dAmtliver 2C19 dt Actliver 2C19 kinact kdeg,liver 2C19 Amt 0,liver 2C19 Amtliver 2C19 kdeg,liver 2C19 fu mic ( I ) K I 1 fu p ( I ) I liver BP ( I ) kpliver ( I ) BP ( I ) 1 fu p ( I ) I liver BP ( I ) kpliver ( I ) BP ( I ) 1 fumic ( I ) ki (12) (13) Where FG (t) is the intestinal availability of the drug; Qgut is a nominal flow in gut model (L/h); fugut is the unbound fraction of drug in enterocytes; fumic(I) is the fraction of unbound inhibitor in the in vitro microsomal incubation; Amtgut2C19 and Amtgut3A4 are the amount of active 2C19 and 3A4 at any given time in the gut; Actgut2C19 and Actgut3A4 are the activity of CYP2C19 and CYP3A4 at any given time in the gut; CLu,int,G (t) is the time-variant intrinsic metabolic clearance of the drug in the gut; kdeg,gut2C19 is the first 7 order turnover rate constant of the enzyme in the gut; The SimCYP mean default value of kdeg,gut2C19 used for the simulations is 0.03/h for the gut, Ipv is the concentration of inhibitor in the portal vein. CLu,int,H(t) is the time-variant intrinsic metabolic clearance of the drug in the liver; Amtliver2C19 and Amtliver3A4 are the amount of active 2C19 and 3A4 at any given time in the liver; Actliver2C19 and Actliver3A4 are the activity of CYP2C19 and CYP3A4 at any given time in the liver; Amt0,liver2C19 is the basal amount of 2C19 in the liver. kdeg,liver2C19 is the first order turnover rate constant of the enzyme in the liver; The SimCYP mean default values of kdeg,liver2C19 used for the simulations is 0.0267/h for the liver; In the absence of inhibitor, the enzyme content in the gut is at steady state and the degradation rate is equal to the synthesis rate, which was assumed to be unaffected by inhibitors. CLu,int,2C19 and CLu,int,3A4 are the time-variant intrinsic metabolic clearance of the drug by CYP2C19 and CYP3A4, respectively; ki is the CYP2C19 competitive inhibition constant of R-omeprazole; kinact and KI are the maximum rate of inactivation and the concentration of inhibitor (R-omeprazole or esomeprazole) that supports half maximal inhibition interaction between the enzyme and inhibitor, respectively; fup(I) is the unbound fraction in plasma, BP(I) is the blood to plasma concentration ratio of the inhibitor(CB/CP); fumic(I) is the fraction of unbound inhibitor in the in vitro microsomal incubation. Kp,liver(I) is the partition coefficient of liver over plasma for the inhibitor; Iliver is the concentration of inhibitor in the liver. 8 SUPPLEMENTARY RESULTS 1. Performance of esomeprazole models (Model E1, Model E2 and E3) and Romeprazole model (Model R1 and Model R2) after IV or oral administration Supplementary Table S1 and S2 show that Model E3-II, relative to Model E1, significantly improved the prediction of clearance after i.v. and oral administration of esomeprazole. Supplementary Table S3 shows that optimized Model R2, relative to Model R1, significantly improved the prediction of clearance after oral administration of Romeprazole. 2. Sensitivity analysis of the impact of TDI parameters (KI and kinact) of CYP2C19 on the CL/F (Dose/AUC) of esomeprazole after oral administration Supplementary Figure S1 shows a representative result for the impact of KI and kinact on the simulated CL/F for esomeprazole after multiple dosing (40 mg q.d.) for 5 days. TDI parameters KI and kinact appear to play an important role in the changes of CL/F, which decreases with both the increase of kinact within the range of 1-10/h and the decrease of KI within the range of 0.1-1 µM. 3. Simulations of active CYP2C19 percentage changes Supplementary Figure S2 shows a representative simulation result for the percentage of active CYP2C19 changes after multiple dosing of omeprazole (40 mg, q.d.) and esomeprazole (40 mg, q.d.) for 5 days. For both omeprazole and esomeprazole, the 9 percentage of active CYP2C19 decreases dramatically during the first 24 hours and then slowly goes down until getting to the steady state at around 48 hours (omeprazole) or 24 hours (esomeprazole). The lowest percentage of active CYP2C19 reaches around 14.1% and 6.2% of original abundance for omeprazole and esomeprazole, respectively. 4. Prediction of Drug-drug Interaction between Omeprazole and Fluconazole: Effect of Concomitant Fluconazole on Omeprazole PK The effect of concomitant fluconazole on omeprazole PK in healthy volunteers with various ethnic groups was predicted using the developed omeprazole PBPK model (combination of esomeprazole model E3-II and R-omeprazole model R2) and fluconazole PBPK model taken from the SimCYP Inhibitor Library. Simulations were conducted according to the trial design reported in the paper by Kang et al (5). In the simulation, a single p.o. dose of 20 mg omeprazole (solution), with fluconazole 100 mg (solution), was administered to male healthy volunteers (n=180, 10 trials and 18 subjects per trial) on day 5 after p.o. dose of 100 mg fluconazole q.d. for 4 days. AUC and Cmax ratios (with/without fluconazole) were calculated using the simulated mean AUC or Cmax values and compared with the observed ratios. The observed and predicted omeprazole AUC ratios (with/without fluconazole) are shown in Supplementary Table S4. Because the study was conducted in Korean population, which is not available in the SimCYP Population Library, we used Japanese, Chinese and Caucasian populations. Compared to the values observed by Kang et al, both predicted AUC and Cmax ratio in Chinese (4.8 and 1.9) and in Caucasian (6.9 and 2.1) populations are comparable to those observed in 10 the Korean population (6.3 and 2.4). Note that we have not considered any possible effect due to formulation differences (solution was used in our simulations while capsule was used in the clinical study). SUPPLEMENTARY DISCUSSION The selection of distribution model of R- and S-omeprazole In this study, minimal PBPK model using SimCYP software was developed to predict drug concentrations in plasma, portal vein and liver compartments as the tissue distribution of R- and S-omeprazole is low with a Vss of 0.1 and 0.2 L/kg which are less than body water (0.7 L/kg) (6). Full PBPK model with TDI inhibition using SimCYP software was also adopted to predict the pharmacokinetic profile after i.v. infusion of 40 mg esomeprazole, however, the simulated results did not capture the observed data, especially it missed the terminal phase (data not shown). For the simplicity of the models and not introducing more unknown parameters such as kps, minimal PBPK model was selected for predicting R- and S-omeprazole pharmacokinetic profiles. Reference List 1. Rowland YK, Jamei M, Yang J, Tucker GT, Rostami-Hodjegan A. Physiologically based mechanistic modelling to predict complex drug-drug interactions involving simultaneous competitive and time-dependent enzyme inhibition by parent compound and its metabolite in both liver and gut - the effect 11 of diltiazem on the time-course of exposure to triazolam. Eur J Pharm Sci 2010; 39(5):298-309. 2. Ogilvie BW, Yerino P, Kazmi F, Buckley DB, Rostami-Hodjegan A, Paris BL et al. The proton pump inhibitor, omeprazole, but not lansoprazole or pantoprazole, is a metabolism-dependent inhibitor of CYP2C19: implications for coadministration with clopidogrel. Drug Metab Dispos 2011; 39(11):2020-33. 3. Hassan-Alin M, Andersson T, Niazi M, Rohss K. A pharmacokinetic study comparing single and repeated oral doses of 20 mg and 40 mg omeprazole and its two optical isomers, S-omeprazole (esomeprazole) and R-omeprazole, in healthy subjects. Eur J Clin Pharmacol 2005; 60(11):779-84. 4. Andersson T, Weidolf L. Stereoselective disposition of proton pump inhibitors. Clin Drug Investig 2008; 28(5):263-79. 5. Kang BC, Yang CQ, Cho HK, Suh OK, Shin WG. Influence of fluconazole on the pharmacokinetics of omeprazole in healthy volunteers. Biopharm Drug Dispos 2002; 23(2):77-81. 6. Chen Y, Jin JY, Mukadam S, Malhi V, Kenny JR. Application of IVIVE and PBPK modeling in prospective prediction of clinical pharmacokinetics: strategy and approach during the drug discovery phase with four case studies. Biopharm Drug Dispos 2012; 33(2):85-98. 12 7. Hassan-Alin M, Andersson T, Bredberg E, Rohss K. Pharmacokinetics of esomeprazole after oral and intravenous administration of single and repeated doses to healthy subjects. Eur J Clin Pharmacol 2000; 56(9-10):665-70. 8. Andersson T, Hassan-Alin M, Hasselgren G, Rohss K, Weidolf L. Pharmacokinetic studies with esomeprazole, the (S)-isomer of omeprazole. Clin Pharmacokinet 2001; 40(6):411-26. 13 Supplementary Table S1. Observed vs. predicted clearance, AUC and Cmax after i.v. single (s.d., Day 1, 0-24 h) ascending doses of esomeprazole solution in population representatives Predicted PK Dose Observeda parameters (mg) Initial model Modified Modified Modified Modified E1 model model model model E2- I E3- I E3-II E3-III (Cluint,2C19 (Cluint,2C19 (Cluint,2C19 (Cluint,2C19 (Cluint,2C19 16.2 16.2 16.2 24.3 32.4 Cluint,3A4 Cluint,3A4 Cluint,3A4 0.36 Cluint,3A4 0.36 Cluint,3A4 0.36 0.612 0.612 µL/min/pmol µL/min/pmol µL/min/pmol µL/min/pmol µL/min/pmol of isoform ) of isoform ) of isoform ) of isoform ) of isoform ) Without KI 0.4 KI 0.8 KI 0.3 KI 0.3 applying umol/L, umol/L, umol/L, umol/L, TDI kinact 6/h kinact 8/h kinact 5/h kinact 8/h CL(Dose/AUC, 20 22.2 21.1 17.9 16.9 19.8 21.5 40 15.8 19.9 14.0 12.8 14.3 13.1 20 2.60 2.75 3.24 3.42 2.93 2.69 40 7.32 5.81 8.28 9.03 8.07 8.83 20 2.62 2.80 2.83 2.89 2.83 2.69 40 5.70 5.92 6.06 6.17 6.06 5.81 L/h) AUC (µM*h) Cmax (µM) a: observed values from Hassen-Alin et al, 2000 (7). The PK parameters such as AUC, Cmax were recalculated using Phoenix WinNonlin based on the digitized data. 14 Supplemental Table S2. Observed vs. predicted clearance after oral single (s.d., Day 1, 0-24 h) and multiple ascending doses (q.d. for 5 days of 20/40 mg esomeprazole solution or 7 days of 15 mg esomeprazole solution) in population representatives PK parameters CL/F (Dose/AUC, L/h) AUC (µM*h) Cmax (µM) Dose(mg) 15 20 40 15 20 40 15 20 40 Observeda s.d. (day1) 67.8 32.9 23.9 0.64 1.76 4.84 0.85 1.33 3.27 m.d. (day5/7) 31.9 18.7 11.0 1.36 3.10 10.5 1.55 1.88 4.73 Predicted Model E1 Model E3-II based on the above Based on the above initial model modified model E3-II Cluint,2C19=16.2 and Cluint,3A4 =0.612 Cluint,2C19=24.3 and µL/min/pmol of Cluint,3A4 =0.36 isoform µL/min/pmol of isoform (Without applying TDI (KI=0.3 μM, kinact=5/h, ka=10/h, fugut=0.03, ka=10/h, fugut=0.03, Vss=0.2 L/kg, Vss=0.2 L/kg, fumic=1) fumic=1) s.d. (day1) 38.4 37.8 37.7 1.13 1.53 3.07 1.20 1.60 3.21 m.d. (day5/7) 37.7 37.8 37.8 1.15 1.53 3.06 1.20 1.61 3.21 s.d. (day1) 39.8 37.4 29.2 1.09 1.55 4.23 1.11 1.5 3.10 m.d. (day5/7) 24.8 20.7 12.5 1.75 2.80 9.24 1.37 1.91 4.29 a. Observed data from Hassan-Alin et al, 2005 and Andersson 2001 (3;8). The PK parameters such as AUC, Cmax were recalculated using Phoenix WinNonlin based on the digitized data. 15 Supplementary Table S3. Observed vs. predicted pharmacokinetic parameters after oral single (s.d., Day 1, 0-24 h) and multiple (m.d., Day 5, 96-120 h or m.d., Day 7, 144-168 h) ascending doses of R-omeprazole solution using population representatives. Predicted PK parameters CL/F(Dose/AUC, L/h) AUC (µM*h) Cmax (µM) Dose (mg) 15 20 40 15 20 40 15 20 40 Observeda s.d. (day1) 127.65 72.38 70.61 0.34 0.8 1.64 0.55 0.8 1.87 m.d. (day5/7) 140.00 65.80 48.25 0.31 0.88 2.4 0.47 0.82 2.34 Initial model (Model R1) Cluint,2C19=29.9 Modified model (Model R2) Cluint,2C19=29.9 µL/min/pmol isoform µL/min/pmol isoform (Without applying TDI, ki=4.05µM (ki=4.05µM, KI =1.6 µM, kinact=4/h, Vss=0.1 L/kg ka=2/h, fugut=0.04, fumic=1) s.d. m.d. (day1) (day5/7) 70.00 64.78 68.93 62.93 66.17 54.62 0.62 0.67 0.84 0.92 1.75 2.12 0.64 0.68 0.86 0.93 1.75 2.02 ka=2/h, fugut=0.04, fumic=1) s.d. m.d. (day1) (day5/7) 71.15 71.15 71.48 71.48 71.48 71.48 0.61 0.61 0.81 0.81 1.62 1.62 0.64 0.64 0.85 0.85 1.70 1.70 a. Observed data from Hassan-Alin et al, 2005 and Andersson 2001 (3;8). The PK parameters such as AUC, Cmax were recalculated using Phoenix WinNonlin based on the digitized data. 16 Supplementary Table S4. Observed vs. predicted omeprazole AUC and Cmax ratios (with/without fluconazole 100mg q.d. from Day 1 to Day 5) following single oral dose of omeprazole 20 mg administered on Day 5 in healthy volunteers Parameters Predicteda in Japanese pop. Predicteda in Chinese pop. Predicteda in Caucasian pop. Observedb in Korean pop. (omeprazole solution) (omeprazole solution) (omeprazole solution) (omeprazole capsules) Omeprazole AUC ratioc 2.5 4.8 6.9 6.3 Omeprazole Cmax ratioc 1.3 1.9 2.1 2.4 (omeprazole+ fluconazole /omeprazole alone) a. Predicted from simulations using virtual population of 10 trials of healthy subjects with various races (n=18 per trial); b. Observed data from Kang et al, 2002 (5). c. Omeprazole AUC ratio = AUCwith fluconzole / AUCwithout fluconazole; Cmax ratio was calculated in a similar manner. 17 Legends to Supplementary Figures Supplementary Figure S1. Changes in esomeprazole CL/F (Dose/AUC) as a function of TDI parameters (KI and kinact) of CYP2C19 pathway, when sensitivity analysis was performed using modified model E3-II in Supplementary Table S2 for esomeprazole after p.o. multiple dosing (40 mg q.d. for 5 days). Supplementary Figure S2. Final model predicted CYP2C19 activity changes in the liver following oral dosing of esomeprazole (A) and omeprazole (B) with TDI effect (dosing regimen: PO-40 mg q.d. for 5 days) Supplemental Figure S3. Simulated (lines) and observed (circles) mean plasma concentration-time profile of R-omeprazole using initial model (model R1) and modified model (model R2) incorporating TDI of CYP2C19 after multiple oral administration of R-omeprazole (A) with 20 mg q.d. dosing for 5 days and (B) with 40 mg q.d. dosing for 5 days in healthy subjects. 18