BL414 Genetics
advertisement

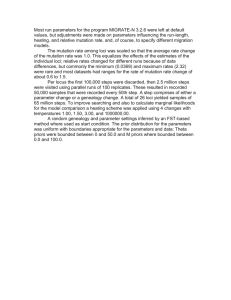
BL414 Genetics Problem Set 4 Answer sheet I. This question assumes that the revertants are caused by an exact reversal of the original mutation. It is also possible that a mutation at another site within the same gene or in another gene could suppress the original mutation – in such a case it would be impossible to tell what the original mutation was without doing molecular analysis at the DNA sequencing level. However if we assume that the revertants are actually reversing the original mutation we would get the following answers: Mutation 1 is reverted by the mutagen that causes transitions, so mutation 1 must have been a transition. Consistent with this conclusion is the fact that the UV light can also revert the mutation and the intercalating agent proflavin does not cause reversion. Mutation 2 is reverted by proflavin and therefore must be either an insertion or a deletion of a base. The other two mutagens do not revert mutation 2. Mutation 3 is not reverted by any of these mutagenic agents. It is therefore not a single-base substitution, a single-base insertion, or a single-base deletion. Mutation 3 could be a deletion of several bases or an inversion. Mutation 4 is reverted only by UV light so it is a single-base change, but not a transition, since EMS did not revert the mutation. Mutation 4 must be a transversion. b. The colonies on the plates could arise by spontaneous reversion of the mutation. Spontaneous reversion should occur with lower frequency than mutageninduced reversion. The important control here is to spread each mutant culture without any mutagen treatment onto selective media to assess the level of spontaneous reversion. A dose response curve would be a good way to quantitatively analyze the mutagenic properties of each mutagen and also normalize the contribution from spontaneous mutations. II. Again we have to make some assumptions to answer this question – the question wants us to assume that the normal tissue is from a patient with one defective p53 gene, and in the tumor tissue, both copies of the p53 gene are defective. By looking at the DNA blot, we try to deduce what the mutations in p53 were. It is also possible that a patient could have two normal copies of p53 and get mutations in both copies to cause cancerous tissue, but that is not the case in this problem. The wildtype p53 region, as seen in the “wild-type” individual, has three hybridizing bands. Because p53 is a tumor suppressor, it is recessive at the cellular level and both copies must be defective in the tumor cells. No observable changes are apparent in patient 1, so this patient must have inherited a small mutation in p53 and in the tumor cells the second copy would also contain a small mutation thereby inactivating both copies of p53 in the tumor. In patient 2, a small mutation must have been inherited. In the tumor, the whole region containing p53 was deleted (thereby removing the second copy of the gene) as seen by the loss of restriction fragments. (If this DNA blot consisted of cDNA which is amplifying the mRNA, the tumor lane could indicate a defect in the promoter region of p53). In patient 3, a deletion mutation (smaller than that in the tumor cells of individual 2), as seen in the altered restriction pattern, was inherited. In the tumor, the second copy of the gene was similarly deleted (probably by homologous recombination causing gene conversion since the pattern is the same for both copies).