Granulocytes & Monocytes: Formation, Function, & Clinical Significance
advertisement

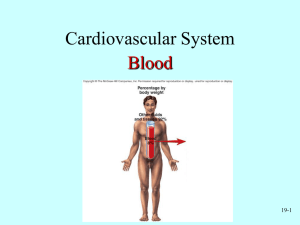
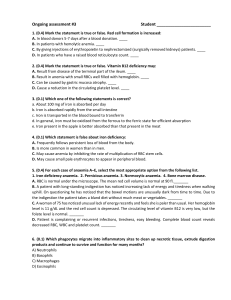
BIO3CBH – Granulocytes and Monocytes Lecturer Helen Irving Intended learning outcomes for this lecture (specifically relating to subject learning outcome 1) By the end of this lecture, you should be able to: • Distinguish different types of white cells in peripheral blood • consider size, organelles, etc. • Explain granulopoiesis and compare it to haemopoiesis • Compare and contrast monocyte and granulocyte formation and function • Explain what differences in neutrophil, basophil and eosinophil amounts in FBE/CBC tell you about the patient’s health • Analyse how malfunctions in granulopoiesis can contribute to disease states • Analyse blood results in relation to granulocytes and monocytes and disease states Leukocytes (white blood cells) in normal peripheral blood Task: note some features. Neutrophils (~ 1,500-8,000/ μL) Eosinophils (~ 0-450 / μL) Basophils (~ 0-200 / μL) Monocytes (~ 200-950 / μL) Blood film stained with Romanowsky type dyes (e.g. eosin and methylene blue) to differentiate white cell features FBE/CBC – WBC: differential versus absolute differential count • Proportion of each leukocyte cell type is important in many diagnostic tests Absolute Differential differential Absolute differential = percentages times total WBC Source: https://upload.wikimedia.org/wikipedia/commons/thumb/6/69/Hematopoiesis_%28human%29_diagram.png/1200px-Hematopoiesis_%28human%29_diagram.png By A. Rad - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=1042490 Stages of maturation of granulocytes What are some of the key features distinguishing myeloblast and mature segmented cells? Which are found in the bone marrow and which in the blood? Stages are the same for basophils, eosinophils and neutrophils, only the granules are different How long does granulopoiesis take? Diameter 16 24 Maturation time 14 days no yes Mitotic Granules 10-12 μm no azurophilic Specific 20% 80% Growth factors responsible for haemopoiesis GM-CSF (granulocytemonocyte colony stimulating factor), interleukins (e.g. IL-3), granulocyte stimulating factor have varying lineage specificities for the granulocytes Integration of factors determining neutrophil lifespan. Neutrophils are also found in “marginated pools,” vascular pools located in the lungs, spleen, and liver. Key: DAMPs – damage associated molecular pattern molecules (AMPs) PAMPs – pathogen AMPs LPS – lipopolysaccharide fMLF - formyl-methionyl-leucyl phenylalanine HMGB1 - high-mobility group box-1 Carlos Silvestre-Roig et al. Blood 2016;127:2173-2181 ©2016 by American Society of Hematology Why are there so many neutrophils? • Neutrophils are phagocytes • Involved in first line of defence against invading pathogens • Important mediators of inflammation induced injuries • Neutropenia: _____________________________________ • Neutrophil leucocytosis: _____________________________ • Recent work suggests neutrophils are actually heterogenous population with roles in shaping adaptive and innate immune responses (Silvestre-Roig et al. Blood 2016;127:2173-2181) Source: Carlos Silvestre-Roig et al. Blood 2016;127:2173-2181 What do these results tell you about the blood of a patient? CBC/FBE • WBC 16,800 / μL • Neutrophil 15,000 / μL • Lymphocytes 1,400 / μL • Eosinophils 340 / μL • Hb 92 g/L • MCV 86 fL • Platelet count 140,000 / μL • Task: Relate the white cell CBC results to the blood film Some changes in neutrophils due to bacterial infection Dohle bodies - Inclusions found near the plasma membrane of neutrophils usually in neutrophil leucocytosis in response to bacterial infection. Toxic granulation - Coarse granulation in neutrophils, another indicator of bacterial infection What do these results tell you about the differential white cell blood count? • • • • • • WBC 16.5 x 109 / L Neutrophils 80% Band cells 4% Lymphocytes 12% Eosinophils 4% Basophils 0 % • • • • • • WBC 17 x 109 / L Neutrophils 66% Band cells 14% Lymphocytes 17% Eosinophils 3% Basophils 0 % Source https://library.med.utah.edu/WebPath/HEMEHTML/HEME001.html • Task: What do you think is meant by “left shift”? Benign disorders – changes in neutrophil morphology Source: https://commons.wikimedia.org/wiki/File:May-Hegglin_smear_2009-11-13.JPG • May-Hegglin anomaly Pelger-Huet anomaly • Autosomal dominant uncommon condition • Task: Compare and contrast the neutrophils? What makes them abnormal? Neutropenia – a case history • Samantha has received chemotherapy for her breast cancer. Samantha is feeling unwell and feverish and attends her hospital (clinically upon arrival she is febrile (e.g. >38°C). She is administered intravenous antibiotics within 60 min of admission followed by G-CSF in consultation with her clinician. • The clinician orders CBC and carefully examines the absolute differentials at 12 hour intervals. • Task: What is the clinician looking for? Explain. What do these results tell you about the blood of a patient? • • • • • WBC 10,800 / μL Neutrophil 7,700 / μL Lymphocytes 2,400 / μL Eosinophils 580 / μL Basophils 120 / μL Source: https://medlineplus.gov/eosinophilicdisorders.html • Task: consider the WBC differential and suggest possible causes and next steps Eosinophils and basophils • Eosinophils, enter inflammatory exudates and have roles in local immune responses and tissue repair • Particularly allergic responses, defence against parasites and removal of fibrin. Normal eosinophil • Basophils rarely seen in normal peripheral blood but are rapidly recruited to sites of inflammation • When stimulated, they release their contents, including histamine, and cytokines to aid immune responses , particularly against parasites Normal basophil Monocytes and their derivatives • Monocytes develop in bone marrow and spend some time in peripheral circulation before entering tissues where they mature to macrophages with different tissue determined functions • Macrophages can self replicate and can live for months to years. • Monocytes can also form dendritic cells involved in antigen presentation Normal monocyte Kidney: Brain: Serosal Intraglomerular microglia macrophages mesangial cells Lungs: Liver: Alveolar Küpffer cells macrophages Spleen sinus: Macrophages, APC Lymph node Bone marrow: Macrophages, macrophages, APC APC APC = antigen presenting cell Comparison of formation of monocyte and basophil phagocytes From Hoffbrand & Moss (2016) Hoffbrand’s Essential Haematology 7th edition Normal and abnormal monocytes From: Lynch & Foucar (2016) Ask the Hematopathologists: Diagnostic Approach to Monocytosis http://www.hematology.org/Thehematologist/Ask/5658.aspx; accessed 12/03/2018 Task: why is moncytosis associated with chronic infections? Questions and Next Lecture • Next lectures will cover the lymphocytes and white cell disorders (see notes to Haematology 3 and 4)