Comprehensive: Primary - Depression, anxiety
advertisement
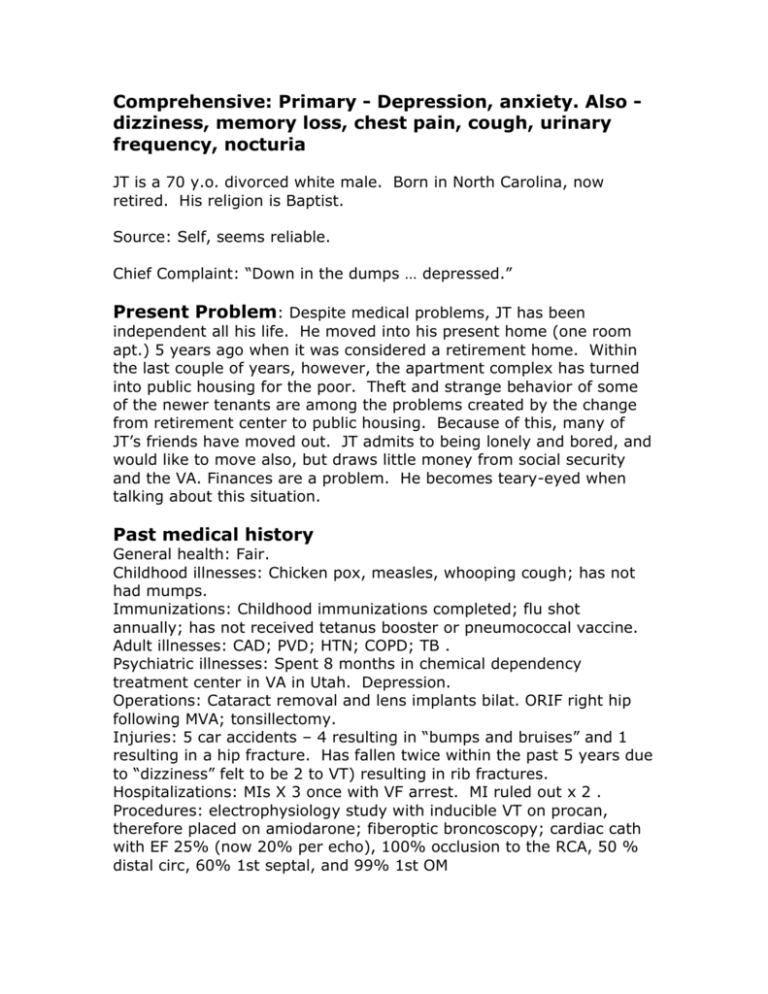
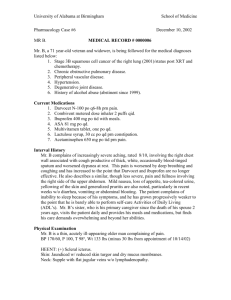
Comprehensive: Primary - Depression, anxiety. Also dizziness, memory loss, chest pain, cough, urinary frequency, nocturia JT is a 70 y.o. divorced white male. Born in North Carolina, now retired. His religion is Baptist. Source: Self, seems reliable. Chief Complaint: “Down in the dumps … depressed.” Present Problem: Despite medical problems, JT has been independent all his life. He moved into his present home (one room apt.) 5 years ago when it was considered a retirement home. Within the last couple of years, however, the apartment complex has turned into public housing for the poor. Theft and strange behavior of some of the newer tenants are among the problems created by the change from retirement center to public housing. Because of this, many of JT’s friends have moved out. JT admits to being lonely and bored, and would like to move also, but draws little money from social security and the VA. Finances are a problem. He becomes teary-eyed when talking about this situation. Past medical history General health: Fair. Childhood illnesses: Chicken pox, measles, whooping cough; has not had mumps. Immunizations: Childhood immunizations completed; flu shot annually; has not received tetanus booster or pneumococcal vaccine. Adult illnesses: CAD; PVD; HTN; COPD; TB . Psychiatric illnesses: Spent 8 months in chemical dependency treatment center in VA in Utah. Depression. Operations: Cataract removal and lens implants bilat. ORIF right hip following MVA; tonsillectomy. Injuries: 5 car accidents – 4 resulting in “bumps and bruises” and 1 resulting in a hip fracture. Has fallen twice within the past 5 years due to “dizziness” felt to be 2 to VT) resulting in rib fractures. Hospitalizations: MIs X 3 once with VF arrest. MI ruled out x 2 . Procedures: electrophysiology study with inducible VT on procan, therefore placed on amiodarone; fiberoptic broncoscopy; cardiac cath with EF 25% (now 20% per echo), 100% occlusion to the RCA, 50 % distal circ, 60% 1st septal, and 99% 1st OM Current Health Status Current Medications: Isordil 40 mg tid; amiodarone 200 mg tid; captopril 50 mg tid; sertraline 50 mg hs; coated asa 324 mg qd; cimetidine 400 mg qd; docusate 100 mg tid; NTG 0.3 mg prn sl; bisacodyl 10 mg prn; mom prn. Allergies: Penicillin (hives). Diet Breakfast: Cereal or eggs, toast, prunes, coffee. Lunch: Canned vegetables, deli salads. Dinner: Cereal, oatmeal or canned chili/soup, canned fruit. Exercise: Walks daily – sky walks in winter, outside otherwise for 1 to 1 ½ miles. Tolerates OK if slow pace, otherwise develops calf pain bilat. States he does not develop angina while walking. Doesn’t use a cane or walker, but stays near walls due to potential for a “dizzy spell” which occurs both with and without chest pain. Alcohol: Abused in past; currently, states to use it rarely if at all. Tobacco: 3-6 cigars per day X 20 years; cigarettes – 55 pack years. Sleep: Sleeps poorly. Has a difficult time falling asleep. Rises early. Frequently tired during the day. Family history Minimal info - Mother’s sister mentally ill, and her uncle was an alcoholic. No family history of CA. Psychosocial JT was raised on a dairy farm. He joined the air force and attended radio and gunners school while enlisted. He served as a radio operator and a B25 and 29 gunner during WWII in the Aleutian Islands. He was honorably discharged “after 3 years, 1 month, and 1 day.” JT was married and had 4 children. During that time he worked as a used car salesman, real estate agent and insurance agent, and traveled a lot. JT and his wife divorced after 15 years of marriage. He is currently not close to any of his kids, and has never seen his grand children. Following the divorce, he attended the University of Georgia, majoring in Marketing. He worked the majority of his employment years in market research, where he again traveled frequently. He quit this job after his second MI, but continued to work part-time with the chamber of commerce, and later with an electronics store as a full-time employee again. In the interim between jobs, JT was an inpt on the chem. dep unit in the Utah VA for about 8 months. Currently, JT lives in a one-room apartment with a small TV, radio, kitchenette, bed, 3 chairs, a table and bathroom. JT’s typical day includes rising early, breakfast in the apartment complex’s dining room, walking, occasionally visiting with friends (planned meetings as most have moved away), and eating lunch in the dining room. Dinner is usually something “simple” in his room. Occasionally he’ll go out to dinner with friends. Every Mon. and Thurs. JT attends the Adult Health Day Center at the VA. He has just started this and is somewhat saddened by the fact that most of the other people are in w/cs. He also finds some of the activities boring. JT’s financial situation is stressful for him, as half of his earnings from SS and the VA go directly to rent. He would like to move out of the apartment, but finances limit his options. Review of Symptoms General: Has gained five pounds since the holidays. Skin: No rashes or other changes. Head: Rare HAs; no hx head injuries. Eyes: Reading glasses; good vision for distances; bilat lens implants, laser therapy to floaters in R eye; last exam: 6 mo ago. Ears: Hearing good; does not have hearing aids; c/o tinnitus for past 4-5 years – alternating ears; hx of wax buildup bilat; no vertigo, infection. Nose/Sinus: Occasional colds. No allergies, nosebleeds, sinus trouble. Mouth/Throat: Upper and lower dentures; last dental exam 3-4 years ago; no bleeding, sore throat, hoarseness, or sores. Neck: No lumps, goiter, or pain. Breasts: No pain, discharge. Respiratory: Has had a productive cough of white sputum for 1 year; had pneumonia as a child and in one post MI/ dx’d and treated for TB ; last CXR 1 month ago; no hemoptysis, wheeze, asthma, or emphysema. Heart: Sleeps on 1 pillow; has had rare instances of PND resolved quickly with sitting up; has occasional cp and palpitations (pt. vague re: frequency – from once a week to once a month) that occasionally lead to dizziness, the two are not always associated with each other. CP is usually relieved with 1-2 ntg; CP occurs at rest and with anxiety (especially re: finances). No edema, dyspnea. EKG: NSR with 1st degree heart block and occasional PVCs. GI: Neg ultrasound 2 weeks ago for new onset of sharp abd pain in varying locations over the abd that occur occasionally for 1-2 minutes at a time; associated with loose, watery stools at least once per day. Hx of constipation. No swallowing difficulties, indigestion, rectal bleeding, food intolerance, excess belching/flatulence, hemorrhoids, jaundice or hepatitis. GU: New onset of urinary frequency, nocturia, hesitancy and dribbling. Has R inguinal hernia that is painful with cough. No incontinence, UTI, stones, penile discharge or testicular pain/mass. Genito-Reproductive: No hx VD/AIDS; is not having sexual relations currently. Musculoskeletal: Occasional c/o lower back pain due to MVA. No arthritis or gout. Peripheral vascular: PVD; calf pain if walking too fast; decreased hair growth knees down. No phlebitis. Neurologic: “Drop foot” to R foot with pain at night due to ORIF. Both feet are numb, and tingle. Reports to have almost “blacked out” on occasion (felt to be assoc. with VT according to chart). States to be having more memory problems. No seizures, paralysis or tremors. Psychological: See present problem and psychosocial. Endocrine: No thyroid problems, sweating, intolerance to heat/cold, diabetes or excessive thirst/hunger. Hematologic: Has received 1 blood transfusion while in the service after a MVA. Reports to bruise easily. No anemia. Physical exam Mr. T is a well-dressed elderly gentleman of average ht and wt. He walks slowly, but appears steady. He answers questions appropriately and likes to converse. He appears sad when discussing his social situation. Pulse: 52, reg. Resp: 12. BP 112/60. Wt. 173. Ht. 5’10”. Skin: Cool, dry. Head: Thinning hair; scalp and skull nl. Eyes: Able to read consent form with reading glasses without difficulty; visual fields are nl; conjunctivas are of good color; scleras are clear; PERRLA; EOMs intact, no nystagmus; L disc well-delineated, R is blurry. Ears: Acuity is fair to quiet voice, better to normal voice; wax partially obstructs TM bilat, but membranes are pearly in color; Rinni test performed with barely audible air vibration L ear, not audible in R; bone vibration long bilat. Nose: No sinus tenderness; septum midline; R nare boggy in appearance, L is moist and shiny. No polyps. Mouth: Upper and lower dentures; tongue midline; mucosa pink and gums appear healthy except for 2 black spots: 1) L back lower gum (1-2 mm diameter), and 2) L buccal mucosa (1 mm diameter); these spots are not painful. Normal phaynx. Neck: Trachea midline; thyroid isthmus barely palpable, lobes not felt. Nodes: No cervical, axillary, epitrochlear or inguinal nodes felt. Thorax and lungs: Thorax symmetrical; good excursion; lungs resonant; diaphragm descends 3 cm on inspiration; BS decreased throughout with few bibasilar rales (L > R). Heart: Distant S1, S2. Negative JVP. Carotid pulses nl, and without bruits. Breasts: No masses or discharge. Abdomen: Sl. Obese, symmetrical, hyper-active bowel sounds; no masses or tenderness; liver, spleen, kidneys not felt; liver span in midclavicular line is 7 cm, Genitalia/Rectal: Pt. chose to omit. Peripheral vascular: Pulses: Radial R 3+, L 3+ Femoral R 2+, L 1+ Pop R 2+, L 2+ DP R 2+, L 2+ PT R 2+, L 2+ Decreased hair growth knees down. No edema or calf tenderness. Musculoskeletal: No joint deformities. ROM nl. to all extremities and spine by observation. Good muscle strength against resistance to upper and lower extremities. Neurological: CNs (see also H&N): 5- strength good and sensation intact; 7- facial movements good; 11- sternomastoids and trapezii strong. Motor: Difficulty with heel and toe walking; turned 360 with discontinuous steps; staggers slightly with nudge. No fasciculations, tremors. Neg Rhomberg. Sensory: Pain, vibration, light touch and position senses intact. Reflexes: Bicep R 2+, L 2+. Tricep R 2+, L 2+. Brachialradialus R 2+, L 2+. Knee R 2+, L 2+. Ankle R 2+, L 1+. Plantar R (ticklish), L (ticklish). Mental Status: Alert, cooperative, coherent thought; LTM intact, did not notice STM deficit.