cbh clinical and child/adolescent committee
advertisement

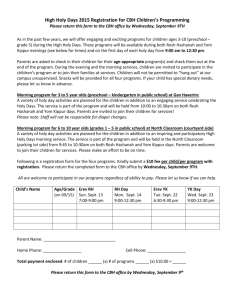
CBH CLINICAL AND CHILD/ADOLESCENT COMMITTEE Minutes – January 23, 2013 The meeting was held at CBH and began at 9:35AM with the following present: Eileen Hastings (UMMC), Clinical Com. Chair and Rob Canosa (Catholic Charities) C&A Com. Chair; Amy Craig-VanGrack and Arleen Rogan (FSI), Cathy and Marty Cassell (Channel Marker), Marsha Gorth (UMMC), Kathy Seifert (ESPS), Trina Payne (MARFY), Samar Khlief (FSF), Rich Bayer and Susanne Blumberg (Upper Bay), Janet Hughes (PEP), Flo Hackerman and Susan Klein (JHBMC), Lillie Hinkelman (Arundel Lodge), Larry Epp (FSIGUIDE), Bill Kordonski and Siri Shaw (Alliance) and Herb Cromwell (CBH). Joining by phone: Sarah Winter-Kolbe (SMCN), Sharon Fischman (SLH-TSI), Cathy Meyers (CFC) and Oleg Tarkovsky (Mosaic). Issues were discussed as follows: CPT Codes – Bill and Siri said VO is rejecting claims for same day services that should be allowed. Upper Bay and others said they too have had this problem. The combination of services rules permit this. Herb cited an email this morning from VO’s Marc Reiner indicating that his staff provided misinformation and to send him the particulars (marc.reiner@valuepotions.com) and copy Karl Steinkraus (karl.steinkraus@valueoptions.com). Bill raised another issue related to the new medication management codes and the interpretation of the elements involved in coding 99212 vs. 99213. Some docs are coding 212 all the time, some 213 all the time. Eileen and Rob said this is a learning curve for docs; Rob will send helpful information from the Academy of C&A Psychiatry. They also cautioned against pattern billing. There was further discussion of the nuances of properly coding this service. Herb said another problem raised by members was VO rejection of 90837; VO acknowledged that this was because VO was late in putting this code into its system and said the rejections should be rebilled. (a later email said not to rebill, VO will reprocess) VO staff also gave out misinformation on that ICD 10 codes should be used; that is not true and won’t be true until 2014; CBH conveyed that to Marc Reiner. OMS Datamart – Tim Santoni followed up recent discussions with CBH with tools to help with data interpretation and analysis. Rob said they give a little more meaning to data differences, adjusting for factors such as effect size. This led to a discussion of the value of benchmarking and the CBH Benchmarking Project. Case mix adjustment still has a way to go in our field. Eileen encouraged all members to go into the Datamart and look at their agency’s data. QuIP – Many agencies present have signed up. VO is just now sending a packet of relevant documents. Eileen reviewed what they include. Participants can access reports about hospitalizations. Flo said this information can be outdated and noted examples; the data is supposed to be available only for consumers with open OMS auths. The biggest concern is the lack of incentive money from MHA and the lack of start-up funds available to providers. Herb said upfront, start-up funding is routine for primary care medical homes but not for us. Without this support, the effectiveness of QuIP will be limited. Provider Services Network – Rob gave an overview of the PSN concept developed by Sheppard affiliated members designed to position community providers to benefit from pay-for-performance and ultimately move to assumption of more financial risk. The eligibility criteria and quality measures are adult oriented. On the adult side, quality measures related to ED reduction for example, is clearly tied to gain-sharing; but for C&A our work impacts less somatic health care and more areas such as school performance, juvenile justice involvement and other non-medical factors where gain-sharing is not now available. Rob asked for feedback on how this PSN approach can work for C&A. He also noted eligibility criteria that don’t apply to children such as the big SAMHSA EBPs. He then suggested C& A levels of care that could be part of this. Arleen described a Care Link project in Montgomery Co. that provides nursing care management for hospital discharged adults to prevent readmission for 1 both psychiatry and somatic care. Rich summarized the three elements to look at: 1) eligibility criteria, 2) the quality measures and 3) where the benefit is. Kathy said the model for C&A is multi-agency and Rob said this is supposed to be via the CME process. Same Day Access – Herb said nine (9) CBH agencies will participate in this National Council initiative. The kick-off webinar is Feb. 1. It is aimed at helping OMHCs facilitate rapid service access, as part of increasing the value of our services to the larger health care world. Rich said his agency is part of a related effort; it is impressive but challenging, particularly with the financial constraints under which we operate. Legislative session update – Herb reported two pieces of good news about the Governor’s FY14 budget: a 2.54% rate increase (rates and grants) and an increase in psychiatric E/M code rates to bring them up to Medicare-equivalency; this should bring an additional $5 million in revenue to OMHCs. On the bad news front, Herb noted the ongoing threat to the carve-out and the pressure by Hopkins, MCOs and others to reject the behavioral health integration recommendation for a performancebased ASO. CBH will be fighting this issue all over again this session. Rich said we do have the power to influence the Secretary and legislature and said our Advocacy Committee can be called into action. There is no news on the Board of Social Work proposal from last summer to require virtually anyone doing social work type of services to be licensed. Kathy noted quality-related reasons for this at least for some staff e.g. in DSS offices. CBH feels overall the proposal is excessive. The Board of Social Work pulled it back. Oleg said the Board of Professional Counselors is putting in legislation to require all licensed counselors to get criminal background checks; the responsibility will be the licensee’s to do it. CBH will follow up. If you are a provider who already has to get background checks for staff, do you have to do another one for LCPCs? Oleg said yes. Herb said we could push that the checks be through private firms such as Kroll instead of having to go through the FBI. Behavioral health integration – We covered this in the earlier discussion of the threat to the carveout. The Secretary has not yet made his decision. Accreditation – Oleg said the last workgroup meeting seemed to indicate that mandated accreditation will require legislation. There is a question as to whether this will be possible this session. If not, it could meant the July 2015 deadline will be moved to 2016. Oleg said another dilemma is which providers will come under the mandate. Health homes – Herb said we are still waiting for Medicaid to release the draft regulations; e.g. the draft Medicaid plan amendments. After review the plan amendment will be submitted to CMS. Whether CMS approval will happen in time for July 1 implementation is a question. C&A services 1915i plan – Rob gave background. The RTC waiver ended last fall and MHA was working on a Medicaid 1915i plan to expand the array of community services for children, particularly those with intensive needs who would otherwise be served in RTC. Ultimately, with CME involvement, the goal is to have such services available for 750 youth as opposed to the couple hundred who were in the RTC waiver. Herb said that Jane Walker reported yesterday that the 1915i has still not gone to CMS for approval. It may be another big issue waiting its turn in the Medicaid office whose first priority is health care reform implementation. Breakthrough Resilience Collaborative – Rob described this initiative. Several CBH members are involved and have assembled teams as he discussed. Adult OMS on BPS Survey – Rob said Benchmarking Project participants added OMS-related C&A items to the quarterly data reports and are now adding adult OMS items. He gave details. This is not a change in OMS. Rob said that some benchmarking capability will be necessary for agencies to meet national accreditation standards. Consumer survey results – Herb said the results of the 2012 survey are now out and they show sizeable declines in satisfaction in almost all areas. MHA says the procedures did not change and it is 2 not clear why satisfaction is lower. Rich ventured a theory: the lack of funds, staff turnover, deteriorating infrastructure etc. are all catching up with providers. Another factor could be the declining of services for people who are no-shows because the provider doesn’t have the resources to maintain support. Bill said Alliance is looking at the Columbia Suicide Severity Rating Scale. Eileen said she uses a tool recommended by the Joint Commission. Kathy said none of the suicide scales out there meet psychometric tests. You take the best you can find; she will send CBH some background for distribution. Arleen asked if anyone has joined the MADC integrated care process? Montgomery County submitted a proposal. Herb said CBH distributed information on this to members several times. Kathy said her agency obtained an addiction license but at this point there are many barriers to service delivery; for example, counselors can not be supervised until the MHA-ADAA merger is complete. Herb said Kathy Seifert will be a plenary session speaker at the MHA conference. She will speak about her research into violence. Larry raised concerns about the potential new reporting requirements that may be coming forth since Newtown. There will likely be related legislation here in Maryland. Herb said CB is keeping an eye on this. The next meeting will be Wednesday, February 27, 9:30AM. The meeting adjourned at 11:25AM. Recorded by Herb Cromwell. 3