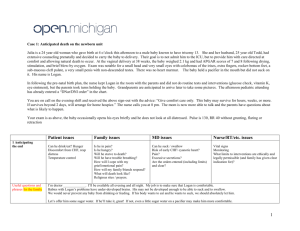
INTERACTIVE CASE STUDY
advertisement

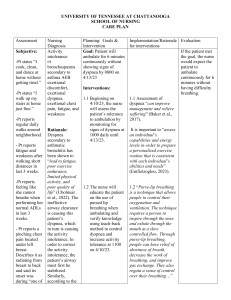
Lewis: Medical-Surgical Nursing, 7th Edition Answer Guidelines for Case Studies in Textbook Chapter 69: Nursing Management: Emergency and Disaster Nursing Trauma 1. The asymmetrical chest movement, decreased breath sounds on the left side of the chest, decreased oxygen saturation, decreased blood pressure, increased heart rate and respiratory rate, and her complaints of shortness of breath indicate a life-threatening breathing problem. The problem is more likely to be a result of hemothorax than pneumothorax, because her vital signs indicate blood loss and there is no other obvious source of significant bleeding. Hypotension can be seen with a tension pneumothorax, but signs specific to a tension pneumothorax, such as tracheal deviation, cyanosis, and jugular vein distention, are not present in this patient. 2. After determining that the patient has an open airway, the priority in her care to is maintain her breathing. She has a life-threatening breathing problem that is the first priority in her care. 3. The patient remains hypoxic on high-flow (100%) oxygen via a non-rebreather mask. The nurse should anticipate rapid sequence intubation and mechanical ventilation to achieve and maintain effective breathing and adequate oxygenation. In addition, a left pleural chest tube will need to be placed to allow for drainage of fluid and reexpansion of the lung. 4. Two large-gauge IV catheters should be inserted for fluid and/or blood replacement and administration of medications. The nurse should prepare to administer fluids, pain medication, and sedation. The head of the bed should be elevated to 30 degrees because of possible increased intracranial pressure as indicated by the patient’s unequal pupil response. The patient has circulatory compromise to her affected leg, but until adequate ventilation and oxygenation are established, the nurse should immobilize the extremity and continue to monitor her peripheral pulses. A urinary catheter will need to be inserted to evaluate fluid replacement and renal function. A nasogastric tube should be inserted to decompress the stomach and reduce the risk of aspiration. Nasogastric drainage should be checked for blood. Laboratory studies, including ABGs and blood typing and crossmatching, will need to be obtained. The nurse should obtain a description of the accident from the patient and a health history, especially any allergies, current medications or drug use, and the last oral intake. After breathing is addressed, surgery will be considered to restore circulation to the lower extremity and reduce the fracture. The nurse should determine the status of the patient’s tetanus immunizations and administer Copyright © 2007 by Mosby, Inc., an affiliate of Elsevier Inc. Answer Guidelines for Case Studies in Textbook 69-2 prophylaxis as indicated. Until the patient is stabilized and transferred from the ED to a clinical unit or surgery, continuous monitoring of vital signs, cardiac rhythm, pulse oximetry, lung sounds, respiratory patterns, level of consciousness, peripheral pulses, and capillary refill must be performed. 5. Hispanic families are usually extended, religious, and expressive in their emotions. In this case, the deaths of the children represent great losses. The mother of the one child who died will need support and this should be arranged (e.g., mental health counselor). It would be proper to ask the family if they would like you to call a member of the clergy. In addition, the family will be concerned about the patient’s condition. Family members are usually very anxious in this type of situation and the nurse should acknowledge and accept their feelings. Lack of information is a major source of anxiety for the family and they should be informed of the patient’s status and the interventions that are being performed to correct or maintain function. As changes in the patient’s condition occur or additional decisions are made regarding collaborative care of the patient, the family should also be informed. Eventually, the patient will need to be told of the status of the children. When this occurs, support should be available (e.g., mental health counselor, member of the clergy). Allowing a limited number of family members to remain with the patient may be reassuring to both the patient and the family. 6. Nursing diagnoses: ineffective breathing pattern, acute pain, fear, anxiety, risk for peripheral neurovascular dysfunction Collaborative problems: hemorrhage, shock, increased intracranial pressure, infection, fat embolism Copyright © 2007 by Mosby, Inc., an affiliate of Elsevier Inc.