zoonoses dog/cat
advertisement

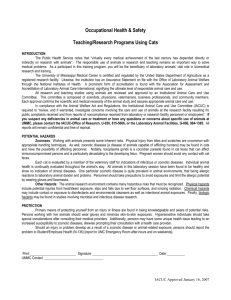
ZOONOSES ZONE "Although zoonotic spread of infectious disease continues to occur in laboratory animals used in biomedical research, reported outbreaks have been minimized with the advent of rigorous veterinary and husbandry procedures, the use of commercially reared animals, and the institution of appropriate personnel health programs. Maintaining animals in modern facilities with appropriate safeguards against introduction of vermin and biologic vectors is also important in preventing zoonotic disease in personnel. Nevertheless, established zoonotic agents, newly discovered microorganisms, or new animal species not previously recognized as carriers of zoonotic microorganisms are encountered, and the potential for spread of infectious disease from animals to humans still exists. Active dialogue between veterinarians and physicians regarding the potential of zoonotic disease, the species of animals that are involved, and the methods of diagnosis, is an indispensable component of a successful preventative health program involving personnel who deal with laboratory animals." Weinberg, A.N., Weber, D.J. "Infectious Disease Clinics of North America: Animal Associated Human Infections". Volume 5, Number 1, 1992 ZOONOTIC DISEASES OF CAT AND DOGS: VISCERAL LARVAL MIGRANS: Visceral larval migrans and ocular larval migrans are conditions caused in humans by different species of roundworms, particularly Toxocara canis and Toxocara cati. The ingested eggs of these roundworms species hatch in the intestines of the aberrant host and produce larvae. The larvae then enter the lymphatics and circulatory system where they may spread to almost any organ. The most common destinations are the liver, lungs, heart, brain and eye. The symptoms are caused by the larvae and by the body's granulomatous response to this intruder. The diagnosis can be suspected when appropriate symptoms occur in a patient with significant eosinophilia. Treatment of VLM is primarily symptomatic. CUTANEOUS LARVAL MIGRANS: Cutaneous larval migrans is a dermatological condition caused by a raised, reddened, itchy rash. It occurs most commonly on the lower extremities and children are the usual victims. Cutaneous larval migrans is caused by the larvae of the cat or dog hookworm, Ancylostoma caninum or A. braziliense. It can be prevented by properly deworming canine populations and proper husbandry procedures for the removal of fecal material. Treatment is supportive. TOXOPLASMOSIS: Toxoplasmosis is a protozoal infection maintained in nature by cats and a wide variety of intermediate hosts. As far as is known, the only sources of human infection are cat feces, raw or undercooked meat, and congenital infection from an infected mother. Although acquired toxoplasmosis infection is usually minor, congenital disease can be quite severe. Approximately 8% of children born with congenital toxoplasmosis are diagnosed at birth with acute generalized or neurological sequelae, and by 10 years of age have developed disabilities ranging from slight visual impairment to blindness and severe mental retardation. In acquired toxoplasmosis, symptoms of fever and generalized body aches can be mistaken for the flu. In immunocompromised persons, a fatal pneumonia or encephalitis may occur. Preventative measures are primarily targeted for pregnant women and include the following: wash hands after handling raw meat and cat litter, thoroughly cook all meat, and wear gloves while gardening. CAT SCRATCH FEVER: Cat scratch disease is an infection associated with a cat scratch or bite that is caused by a small gram negative pleomorphic bacillus. The cat itself is thought merely to serve as a mechanical vector for this disease. The disease is characterized by a primary tender papule or vesicle that occurs at the scratch site 3 to 10 days after the injury. Days to weeks later, a regional lymphadenopathy usually appears, The involved nodes may become filled with pus and drain spontaneously, but usually heal with little scarring. Systemic symptoms are mild and most commonly consist of headache, fever and malaise. RINGWORM: Dermatomycosis, or ringworm, is an extremely common presenting complaint in the office of the primary care physician. Animal contact is not necessary for a human being to develop ringworm; however, the most common causative fungi, Microsporum canis and Trichophyton mentagrophytes, are shared by both man and pets. Transmission can occur with direct or indirect contact with carrier animals, bedding, caging or other materials. The skin lesion of dermatomycosis is usually a pruritic papule that spreads peripherally with central clearing. The scalp is more frequently involved in M. canis infection with resultant hair loss is many cases. T. mentagrophytes infections usually occur on the body. Infected pets, particularly cats, may show no overt signs of disease. RABIES: Although rabies infection has been increasing in the feral animal population of the United States, at this time, there are few reports of rabies diagnosis from laboratory animal facilities. Most laboratory animal species are susceptible, however, many species are bred specifically for the laboratory and are routinely vaccinated, and as such, have limited exposure to the virus. Transmission of the virus occurs through bite wounds with contact of infected saliva. Incubation periods can vary, and clinical signs are not a definitive indicator of the stage of infection. Animals may have clinical signs that vary from none to a "dumb" state to "furious". Vaccines are available for domestic animals and as well as preexposure prophylaxis for humans in high risk situations. ANIMAL BITES: An estimated 500,000 to 1 million animal bites are reported each year in the U.S., accounting for 1% of all emergency room visits. Although most bites produce minor injury, at least 10% require suturing, and 1-2% require hospitalization. Approximately 75% of bites are of canine origin. Although most morbidity from animal bites results from the physical trauma of the bite, a proportion of bite wounds become infected. Infection of the wound site (mainly Pasturella multocida) may occur in 5-15% of dog bites and a higher percentage of cat bites. Tetanus immunization status of the bite victim should be determined and a booster given if more than 10 years has passed since the last tetanus booster. ALLERGIC DISEASE:Allergic disease is often overlooked as an animal related malady. Allergic disease secondary to animal dander usually presents as allergic rhinitis or as an asthmatic condition. As much as 5% of the general population may have a sensitivity to animal dander. Protective measures may vary from total avoidance of animal dander to use of mask, gloves, overclothing or respirators. Proper protective garments may minimize exposure to the allergens thereby postponing or avoiding the immune system triggers. Treatment is supportive.