Teacher Notes - Reproduction

Notes – Reproduction
Function of reproductive system – to produce offspring
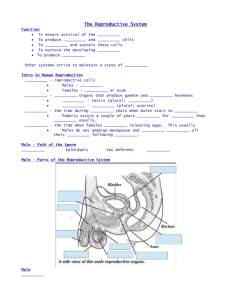
Anatomy of Male Reproductive system
External organs
Testis – primary gonad (sex organ); 5cmx3cm, enclosed in scrotum;
Structure – 250 lobules, ea contains 1 to 4 coiled
semineferous tubules (70cm long uncoiled); joins the
epipidymis; sem.tub. lined with spermatogenic cells (stem cells) produce sperm; interstitial cells produce male sex hormones
Disorder – testicular cancer: epithelial cells in sem tub; occurs in young men, 1 st sign is enlargement of testis or scrotal mass; testis is removed; cure rate is high
Spermatogenesis – sem tub includes 2 cell types, supporting cells and speratogenic cells, sperm production continues throughout reproductive life; sperm collects in the lumen of ea sem tub and pass to epididymis to mature; in young males spermatogenic cells are undifferentiated (spermatogonia) ea contains 46 chromosomes; in early adolescence hormones stimulate cells to undergo mitosis some enlarge to become primary spermatocytes, which undergo meiosis; secondary spermatocytes – spermatids – sperm cells
Head – nucleus, 23 chrom, acrosome at top that contains enzymes to aid in penetrating the egg
Body – contains mitochondria
Tail – flagellum for motility
Scrotum – pouch of skin that hangs from the lower abdominal region; divided into chambers by medial septum; each chamber houses a testis; also contains a serous membrane
1
Penis – organ that conveys urine and semen through urethra; made of three columns of erectile tissue, 2 dorsal corpus cavernosa and one corpus spongiosum; ea column is surrounded by tough white fibrous connective tissue; at the end is the glans penis- sensitive cone shaped portion that covers the copora cavernosa and bears the urethral opening; skin is very thin and hairless; foreskin removed by circumcision.
Internal Accessory organs
Epididymis – tightly coiled tube, 6m long, becomes the vas deferens; immature sperm cells mature and become mobile
Vas deferens – muscular tube about 45cm long, unites with duct of sem vesc. To form ejaculatory duct
Seminal vescicle – sac-like structure 5cm long, secretes a slightly alkaline fluid to help the sperm get through the acid in the vagina; also high in fructose
Prostate gland – surround the beginning of the urethra; secretes a slightly alkaline, (milky); grows to maturity in adolescence, remains unchanged between 20-50 years of age, commonly enlarges in older males which may interfere with urination, treatment is surgical
Bulborethral gland – (Cowper’s gland) 2 structures below the prostate; secrete a mucus like fluid in response to stimulation; provide lubrication at end of penis
Semen: fluid conveyed to outside (by male urethra) as a result of sexual stimulation; consists of sperm secretions, prostaglandins which aid in sperm survival; vol released ranges from 206mL; sperm cells remain inable to fertilize an egg until they enter the female reproductive tract; capacitation – involves changes that weaken the acrosomal membrane
Male infertility (sterility) – lack of ability to induce the fertilization of the egg; caused by – 1). failure of testis to drop into scrotal sac, if sty in abdom, high temp can kill the sperm 2).
Mumps can cause inflammation of testis and destroy cells of sem tub 3). Deficiency of sperm cells or semen (normal 120 million sperm cells per mL) need many sperm because release
2
enzymes from acrosome that remove layers around the egg cell
4). Quality of sperm (motility)
Hormonal control of male reproductive function
Hypothalamus and pituitary – H. secretes gonadotropin releasing hormone to the ant pit which secretes LH, FSH, and ICSH which promotes the development of testes which secrete sex hormones
Androgens – male sex hormones most produced by interstitial cells of testes, some released by adrenal cortex
Testosterone – stimulates spermatogenic cells to undergo spermatogenesis, most abundant, secreted during fetal development and a few weeks after birth; nearly ceases during childhood; between 13-15 androgen production increases rapidly – puberty – phase in development in which the individual becomes reproductively functional.
Testosterone functions: enlargement of testes, dev of secondary sex characteristics, inc body hair in axillary and genital area, enlargement larynx and thickening of vocal cords, thickening of skin, inc musc growth, thicken and strengthening of bones, inc metabolism and RBC production; regulated by negative feedback, amount of testosterone decreases by age 40, male climacteric
Ejaculation – network of vascular spaces separated from each other by crossbars of smooth muscle and connective tissue, normally remain small partially due to contractions in smooth muscle, during sexual stimulation, smooth muscle becomes relaxed, parasympathetic nerve impulses (sacral p/w from the spinal cord) cause arteries in the penis to dilate which causes the veins to constrict (so blood stays in the penis) arterial blood enters the spaces and the penis swells, elongates and becomes erect.
Orgasm – culmination of sexual stimulation, involves a pleasurable feeling of physiological and psychological release, in males accompanied by emission and ejaculation
Emission – movement of sperm cells from the testes and secretions from the prostate and sem vesc into the urethra, occurs in response to sympathetic nerve impulses from the spinal cord which causes peristaltic contraction in testicular ducts, epid, vas deferens and ejaculatory ducts.
3
Organs of the Female Reproductive System
Function to produce and maintain female sex cells - eggs
Ovaries – two, one on ea side in the lateral wall of the pelvic cavity
Structure – medulla – inside, composed of loose connective tissue
Cortex – outer layer, houses the ovarian follicles
Internal Accessory organs
Uterine tubes (fallopian tubes) – walls lines with cilia on simple columnar epithelia which secrete mucus, location of fertilization,
Uterus – receives the embryo and sustains life during development, lower 1/3 is the cervix; cervical cancer detected by pap smear
Vagina – fibromuscular tube extending from the uterus to outside, partially closed by a thin membrane of connective tissue – hymen
Vulva – external organs
Labia majora – encloses and protects other external reproductive organs, rounded folds of adipose tissue, separated by a cleft, joins anteriorly at mons pubis, above pubic symphysis
Labia minora – flattened folds within cleft between labia majora, connective tissue, vascular
Clitoris – anterior end of vulva, b/w labia minora, corresponds to penis, composed of two columns of erectile tissue, richly supplied with nervous tissue
Vestibule – space enclosed by labia minora, pair of vestibular glands lie on either side of vagina, erectile tissue – vestibular bulb
Erection, lubrication and orgasm – erectile tissue responds to stimulation, parasympathetic nerve fibers pass from the sacral portion of spinal cord causing arteries to dilate and veins to contract, clitotis swells, vagina expands, mucus secreted into vestibule, culmination of sexual stimulation is orgasm
4
Hormonal control of female reproductive functions
Hypothalamic, ant. Pit and ovary control hormones secretions.
Hypothalamus secretes gonadotropin releasing hormone to the an. Pit to release LH or FSH; female sex maturation and production of sex hormones;
estrogen – ovary; stimulates enlargement of accessory organs and secondary sex characteristics
progesterone – ovary; promotes changes in uterus during female reproductive cycles; affects mammary glands and regulates secretion of gonadotropins from ant pit
androgen – increases hair growth, low concentration therefore narrow shoulders and broad hips
Female reproductive cycles
Oogenesis and the ovarian cycle
Before birth, oogonia (female stem cells) divide through mitosis to produce primary oocytes which move into the ovaries to form primary oocytes. After birth oogonia do not exist. Lifetime supply of of primary oocytes is about 700,000.
At puberty FSH stimulates a few primary follicles to grow each month
– the ovarian cycle.
1.
follicle enlarges through stimulation of FSH and fills with fluid
2.
primary oocytes begin meiosis, at the end of the first stage a secondary oocyte and a polar body; secondary oocyte arrested in metaphase II
Follicle development to this stage takes about 14 days
3.
LH is released which cause the secondary oocyte to be released from the follicle; LH causes the follicle to become the corpus luteum
4.
If the secondary oocyte is penetrated by a sperm, it will undergo meiosis II that produces another polar body and a ovum nucleus that is haploid and combines with the sperm to form the fertilized egg.
5
Menstrual (uterine) cycle – cyclic changes that the endometrium goes through
1.
Days 1-5 Menses – endometrial lining is sloughed off ; bleeding for 3-5 days; approx ¼ to ½ cup
2.
Days 6-14 Proliferative stage: rising estrogen levels help to repair the endometrial lining (ovulation occurs at the end of this stage)
3.
Days 15-28 Secretory stage: rising progesterone from the corpus luteum causes the endometrium to increase its blood supply even more and for its glands to increase in size; if fertilization occurs the embryo produces a hormone similar to LH which causes the corpus luteum to continue to produce its hormone; if fert does not occur, the corp lut degenerates and progest levels drop causing the b.v. in the endometrium to kink and endometrial cells to die
Menopause – aging of ovaries, follicles no longer mature, ovulation doesn’t occur, blood concentration of estrogen decreases
Mammary glands – secrete milk following pregnancy
Breast cancer – leading cancer in women, breast self-check monthly after menstruation, mammagram after age 40.
Birth control
1. Barrier Methods: employ physical (condom) or chemical
(spermicide) means to separate the sperm from the egg; 88% effective
Male and female condoms
Diaphragms – cap the cervix and block the passage of the sperm into the uterus
2. Hormonal methods: 99% effective, suppress ovulation, usually contain a combination of hormones that prevent the release of FSH and LH, inhibiting the development of the follicle so that no oocytes are released
Oral contraception –
Time-release capsules
3. Surgical Methods: physical prevention, 99% effective
6
Tubal ligation – oviduct is cut and ends tied off to prevent eggs from reaching the uterus
Vasectomy – vas deferens connecting the testes to the urethra is cut and sealed to prevent transport of the sperm
4. Preventing implantation – interferes with the implantation of the blastula into the uterine wall; 99% effective
RU-486 – morning after pill
Intrauterine device (IUD) – springy plastic device inserted through the cervical canal and left in place for 1-4 years
Sexually Infectious Diseases
Category I – produce inflammation of the urethra, epididymis, cervix or oviducts, pain in abdominal cavity; bacterial, can be treated an cured with antibiotics
Gonorrhea – “clap” bacteria, penile and vaginal discharge, abdominal pain and discomfort, can cause scarring and female infertility, often accompanies Chlamydia
Chlamydia – most common infection, 1-3 week incubation, painful urination
Category II – produce sores on the external genitals
Genital herpes – viral, symptoms can be treated, but disease cannot be cured; most common in this class, incubation 4-10 days, red blisters, after 2-10 days blisters burst and seep fluid then form scabs
Syphilis – bacterial, curable with antibiotics
Stage 1: ulcer appears at the site of infection, small hard lesion with no discharge, disappears in 4-6 weeks
Stage 2: pink rash all over body, fever, skin eruptions, joint pain, hair loss, last 3-12 weeks, symptoms can come and go for up to 5 years, still treatable
7
Stage 3: neurosyphilis, damage to b.v. and heart valves, thickening of meninges and lesions on brain, paralysis and dementia
Category III – viral diseases that affect organs other than the reproductive system; spread by sexual contact or blood, infected individuals may appear symptom free for years after infection.
HIV
Hepatitis B
Hepatitis C
8