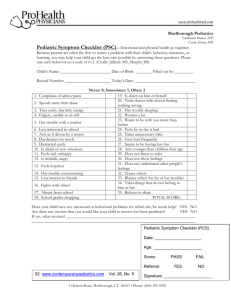
symptom_checklist51907
advertisement
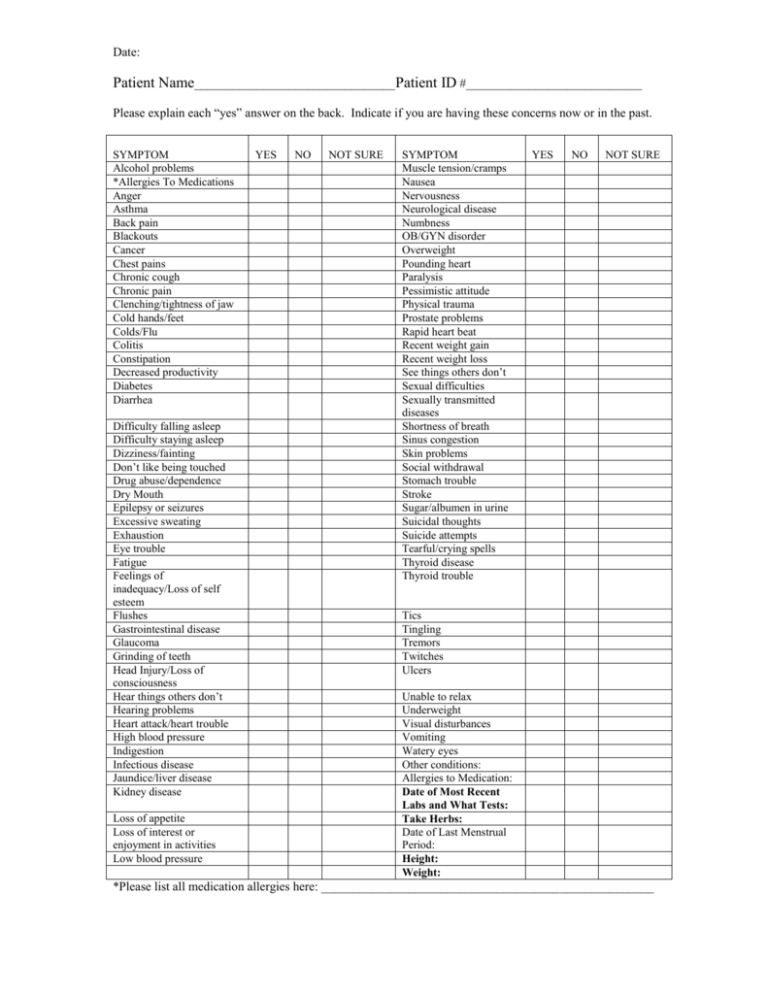
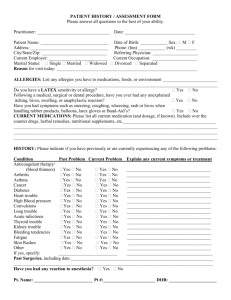
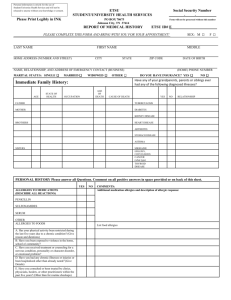
Date: Patient Name________________________________Patient ID #____________________________ Please explain each “yes” answer on the back. Indicate if you are having these concerns now or in the past. SYMPTOM Alcohol problems *Allergies To Medications Anger Asthma Back pain Blackouts Cancer Chest pains Chronic cough Chronic pain Clenching/tightness of jaw Cold hands/feet Colds/Flu Colitis Constipation Decreased productivity Diabetes Diarrhea Difficulty falling asleep Difficulty staying asleep Dizziness/fainting Don’t like being touched Drug abuse/dependence Dry Mouth Epilepsy or seizures Excessive sweating Exhaustion Eye trouble Fatigue Feelings of inadequacy/Loss of self esteem Flushes Gastrointestinal disease Glaucoma Grinding of teeth Head Injury/Loss of consciousness Hear things others don’t Hearing problems Heart attack/heart trouble High blood pressure Indigestion Infectious disease Jaundice/liver disease Kidney disease Loss of appetite Loss of interest or enjoyment in activities Low blood pressure YES NO NOT SURE SYMPTOM Muscle tension/cramps Nausea Nervousness Neurological disease Numbness OB/GYN disorder Overweight Pounding heart Paralysis Pessimistic attitude Physical trauma Prostate problems Rapid heart beat Recent weight gain Recent weight loss See things others don’t Sexual difficulties Sexually transmitted diseases Shortness of breath Sinus congestion Skin problems Social withdrawal Stomach trouble Stroke Sugar/albumen in urine Suicidal thoughts Suicide attempts Tearful/crying spells Thyroid disease Thyroid trouble YES NO NOT SURE Tics Tingling Tremors Twitches Ulcers Unable to relax Underweight Visual disturbances Vomiting Watery eyes Other conditions: Allergies to Medication: Date of Most Recent Labs and What Tests: Take Herbs: Date of Last Menstrual Period: Height: Weight: *Please list all medication allergies here: _____________________________________________________