Patients not appropriate for offering benzodiazepine
advertisement
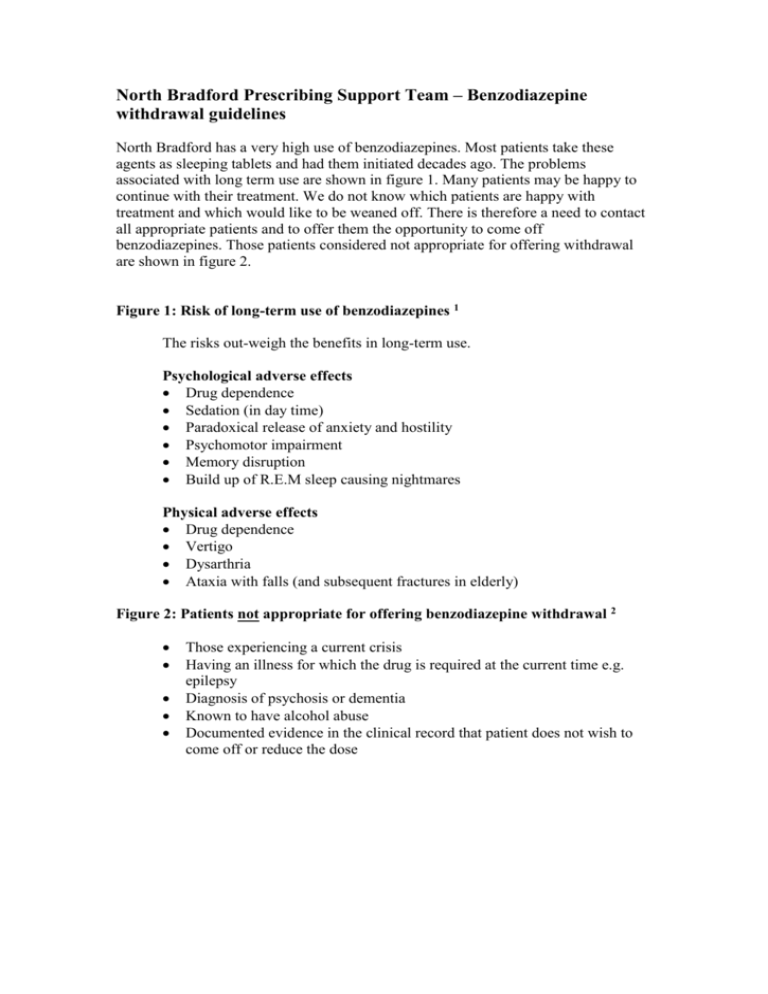
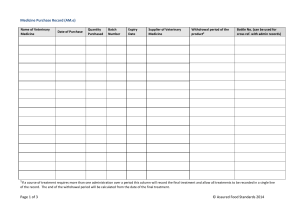
North Bradford Prescribing Support Team – Benzodiazepine withdrawal guidelines North Bradford has a very high use of benzodiazepines. Most patients take these agents as sleeping tablets and had them initiated decades ago. The problems associated with long term use are shown in figure 1. Many patients may be happy to continue with their treatment. We do not know which patients are happy with treatment and which would like to be weaned off. There is therefore a need to contact all appropriate patients and to offer them the opportunity to come off benzodiazepines. Those patients considered not appropriate for offering withdrawal are shown in figure 2. Figure 1: Risk of long-term use of benzodiazepines 1 The risks out-weigh the benefits in long-term use. Psychological adverse effects Drug dependence Sedation (in day time) Paradoxical release of anxiety and hostility Psychomotor impairment Memory disruption Build up of R.E.M sleep causing nightmares Physical adverse effects Drug dependence Vertigo Dysarthria Ataxia with falls (and subsequent fractures in elderly) Figure 2: Patients not appropriate for offering benzodiazepine withdrawal 2 Those experiencing a current crisis Having an illness for which the drug is required at the current time e.g. epilepsy Diagnosis of psychosis or dementia Known to have alcohol abuse Documented evidence in the clinical record that patient does not wish to come off or reduce the dose Strategies for benzodiazepine withdrawal The key to successful withdrawal is; Patient motivation Gradual dosage reduction Anxiety management Method 1 : Benzodiazepine withdrawal – self management of withdrawal Asking patients, either verbally, or by letter (see example) will result in around 1660% either stopping or substantially reducing the dose by themselves.3,4,5 The following points need to be considered: This method works best for patients taking low doses (the higher the dose the greater the likelihood of dependence). Emphasis the benefits of withdrawal. Needs the patient to be motivated. Withdrawal may need to occur over a several months or longer Ask patient to cut down the dose very gradually by reducing the number of tablets and then, if necessary, halving the last tablet Warn patients of benzodiazepine withdrawal syndrome (see box) 40% of patients can stop with no difficulty. About 40% may experience benzodiazepine withdrawal syndrome. Patient who experience benzodiazepine withdrawal syndrome may need a slower reduction in dose. In which case method 2 is recommended. Box : Benzodiazepine withdrawal syndrome Recurrence of the underlying disorder Rebound symptoms lasting only a few days after drug discontinuation Withdrawal symptoms e.g. excess sensitivity to light and sound, tremulousness, sweating, insomnia, abdominal discomfort, tachycardia (and mild systolic hypertension).2 Abrupt withdrawal can cause convulsions, panic attacks and confusional states Method 2: Benzodiazepine withdrawal – conversion to diazepam with support. This method is particularly important for patients on high doses and those experiencing difficulty in reducing the dose of their current benzodiazepine. 1. Convert patient to equivalent daily dose of diazepam preferably taken at night. Diazepam is a long acting benzodiazepine and makes the dose reduction much easier. It does not produce the “kick” often experienced after larger doses of temazepam, but its calming effect may last up to 24 hours. 2. The rate of withdrawal needs to be tapered for each individual patient. Patients on an initial dose of diazepam 20mg daily or less may need a dose reduction of 1mg every 1 to 2 weeks. Patients on initial doses of 40mg of diazepam can usually tolerate larger dosage reductions of 2mg every 1 to 2 weeks. Once a daily dose 45 mg has been reached then dose reduction may need to be 0.5mg every 1 to 2 weeks. If withdrawal symptoms occur, maintain at this dose until symptoms improve (it may be necessary to step back up the dose for a short while). It is better to reduce too slowly rather than too quickly.6 3. Diazepam is available as 2mg and 5 mg tablets or liquid 2mg/5ml (for very gradual reduction e.g. 1ml is 0.4mg. 4. Stop completely. Withdrawal may take 6-8 weeks or even up to 1 year. 5. Once treatment has stopped continue to provide cognitive treatments to support patient if necessary (see method 3). Equivalent doses of benzodiazepines (from BNF) Approximate equivalent doses, diazepam 5mg = = = = = = chlordiazepoxide 15mg lorazepam 500 micrograms lormetazepam 0.5-1mg nitrazepam 5mg oxazepam 15mg temazepam 10mg Method 3: Anxiety management 6 Patients withdrawing from benzodiazepines may suffer from anxiety. Many patients are anxious anyway. Whether the anxiety is due to withdrawal or another cause it needs managing. The degree of support required will vary from simple encouragement to formal cognitive, behavioural therapies. Support may need to be given during the withdrawal stage and for prolonged periods afterwards. Providing information Clear information about how best to withdraw treatment needs to be given at the outset. Emphasis the fact that withdrawal will be tailored to the individual; it will be gradual and can stop at any stage. Explain that the specific symptoms that may be experienced are temporary and not a sign of physical or mental disease. Try and dispell any inappropriately held beliefs’ patients have about withdrawal. Dealing with specific symptoms Insomnia Give reassurance Advise on avoiding stimulants such as tea, coffee and alcohol at bed time Use of relaxation tapes and anxiety management techniques Panic attacks Panic attacks can occur for the first time during withdrawal. Give an explanation of the physical mechanism of panic Keeping a diary can help to pinpoint precipitating factors Patients can exercise control by using relaxation techniques, breathing exercises, being trained in anxiety management, through yoga etc. Discovering that panic attacks can be managed without having to take a tablet can be a boost to self-confidence. Agoraphobia Agoraphobia and social phobia may occur for the first time during withdrawal (it may have been the underlying reason for prescribing the benzodiazepine in the first instance). Formal therapy can be offered but in most cases the phobia disappears along with other symptoms after drug withdrawal. Depression Clinical depression requires treatment with antidepressants Motivation Highly motivated patients can usually manage their own withdrawal Less motivated patients can be encouraged by pointing out the advantages of withdrawal and offering a reducing in dose (rather than a complete withdrawal). Enforced withdrawal will not work and is inappropriate. Many patients may simply choose to reduce the dose rather than stopping completely. Outcome of withdrawal Symptoms characteristically wax and wane, varying in severity and type. Typically “windows” of normality appear and over time these “windows” become longer whilst discomfort slowly regresses. However patients remain vulnerable to external stresses for some time and the clinical course after drug cessation can be protracted. References 1. 2. 3. 4. 5. 6. Lader MH. Limitations on the use of benzodiazepine in anxiety and insomnia:are they justified. Eur. Neuropsychopharmacol 1999;suppl 6:S399-405 Anon . Managing hypnotic and anxiolytic withdrawal in primary care. Regional Drug and Therapeutic Centre. Drug Update.2001;number 14. Hopkins D,sethi K, Mucklow J. Benzodiazepine withdrawal in general practice. Journal of the Royal College of General Practitioners. 1982;32:758-762. Cormack M, Owens RG, Dewey ME. The effects of minimal interventions by general practitioners on long-term benzodiazepine use. Journal of the Royal College of General Practitioners. 1989;39:408-411. Holden J. benzodiazepine prescribing and withdrawal for 3234 patients in 15 practices. Family Practice 1994;11:358-362. Ashton H. The treatment of benzodiazepine dependence. Addiction 1994;89:15351541. Procedure for writing out to all patients in a practice on benzodiazepines Identify patients prescribed benzodiazepines chronically (i.e. 3-4 months) Identify patients who are appropriate for benzodiazepine withdrawal Ask each appropriate patient if they would like to discontinue treatment (see letter) If yes If no Ask patient to try and quit by themselves (method 1) if would like to quit Try and opportunistically talk to the patient Explain risks of chronic treatment and benefits of quiting If patient has problems in withdrawing or reducing the dose too fast then increase the dose again and re-continue with gradual withdrawal If unable to quit or wants support Then offer reduction strategy using Diazepam and support (method 2 and 3) Once drug withdrawal has begun offer Anxiety management (method 3). Continue To offer this support if necessary after withdrawal If still not willing to quit record that the patient is not willing or able to withdraw despite counselling Use a Read code such as “chronic benzodiazepine user” Example letter (to be amended by each practice if necessary) Dear I have noticed in your record that you have been taking …………. for some time now. I am writing to you because, recently, family doctors have become concerned about this kind of tranquilizing medication when it is taken over long periods. Research has shown that the body can become used to repeated use of this sort of medication so the tablets no longer work properly. The tablets may also cause anxiety and sleeplessness and they can be addictive. I am writing to ask you to consider cutting down on your dose of these tablets and perhaps stopping them at some time in the future. It is best to cut down very gradually because you will be less likely to have unpleasant withdrawal symptoms. The best way to cut down is to take these tablets only when you feel they are absolutely necessary. For example, take them only when you know you have to do something that might be difficult for you. Once you have begun to cut down, you might be able to think about stopping them completely. If you would like to talk to your doctor or the practice pharmacist about this then please make an appointment. Please indicate on the attached slip whether you would like to try and come off these tablets or not. Yours sincerely Dr and Partners Patient …………………… I would like to try and reduce the dose of my sleeping tablet with a view to possibly stopping them some time in the future I do not want to stop my sleeping tablets and do not need any help Please return this slip with your next repeat prescription request. Your response will be treated in strict confidence.