Alprazolam and other benzodiazepine withdrawal
Pharmaceutical Services Branch
Alprazolam and other benzodiazepine withdrawal
A resource for Western Australian medical practitioners
Introduction
It is important to ensure that the patient is supported when choosing to withdraw him/her off benzodiazepines. Patients who are assessed as requiring withdrawal and who have substance abuse issues may need to be referred for specialist advice.
Patients who aim to withdraw from benzodiazepines generally fall into one of two categories:
1. Patients who use benzodiazepines for therapeutic purposes only and do not misuse their prescriptions. These patients generally have been prescribed benzodiazepines for a length of time.
1,2 These patients can be managed by their general practitioner.
3
2. Patients who use benzodiazepines erratically in high doses, with other drugs
(polysubstance user). These patients may misuse their prescriptions or use illicit benzodiazepines.
1, 2 These patients are best managed by practitioners with expertise in addiction medicine.
Objective of withdrawal
The aim of benzodiazepine withdrawal is to provide the patient with a minimum supply of medication to prevent severe withdrawal, and to gradually reduce the amount taken.
Benzodiazepine withdrawal requires careful planning due to the risk of a withdrawal syndrome occurring.
4
Withdrawal treatment guidelines
Where possible transfer a patient to a long acting benzodiazepine e.g. diazepam. See
Appendix 1 for comparative doses of benzodiazepines.
5,6
Patients with polydrug use or on high benzodiazepine doses (approximately greater than
40mg of diazepam equivalence) may require management under specialist supervision.
Any underlying, independent disorder such as mood or anxiety should be treated concurrently.
If converting a patient to another benzodiazepine prior to withdrawal, ensure the patient is stable on the chosen benzodiazepine before commencing dose reductions.
Dose reduction should be gradual, approximately every one to two weeks. Dose reductions will vary between patients.
Pro re nata (PRN) doses should not be prescribed.
Do not continue to reduce benzodiazepine dose if patient is experiencing withdrawal symptoms. Stabilise the patient at the dose at which withdrawal symptoms are experienced before commencement of further dose reductions.
1
Pharmaceutical Services Branch
Ensure that adequate records are documented in patient notes of each prescription issued, to maintain a tight control on when renewal prescriptions are due, to prevent overprescribing.
Limited dispensing such as daily or weekly dispensing may be warranted for patients who require an increase in frequency of prescriptions.
This is an effective strategy to control medication intake.
Implement a benzodiazepine treatment agreement to clarify conditions and goals of treatment. The Department has developed a Treatment Contract which incorporates those benzodiazepines which are Schedule 8 (S8) medicines (alprazolam and flunitrazepam).
This contract may be used as a guide to the development of individual patient treatment contracts.
Where to refer/seek further advice on withdrawal
For complex polysubstance abuse patients, specialist advice may be necessary from:
local addiction medicine specialist
Clinical Advisory Service – a telephone service provided by specialist clinicians at Next
Step Specialist Drug and Alcohol Services, available 24 hours a day seven days a week. Telephone (08) 9442 5042 or 1800 688 847
psychiatrist.
For legislative matters pertaining to the prescribing, supply and dispensing of S8 benzodiazepines and other S8 medicines, contact:
Pharmaceutical Services Branch of the WA Department of Health, available Monday to
Friday, 8.30am
– 4.30pm. Telephone
(08) 9222 4424.
To check if a patient is obtaining benzodiazepines prescriptions including other prescription medicines subsided by the Pharmaceutical Benefits Scheme, contact:
Medicare Australia Prescription Shopping program, available 24 hours a day, seven days a week. Telephone 1800 631 181.
2
Pharmaceutical Services Branch
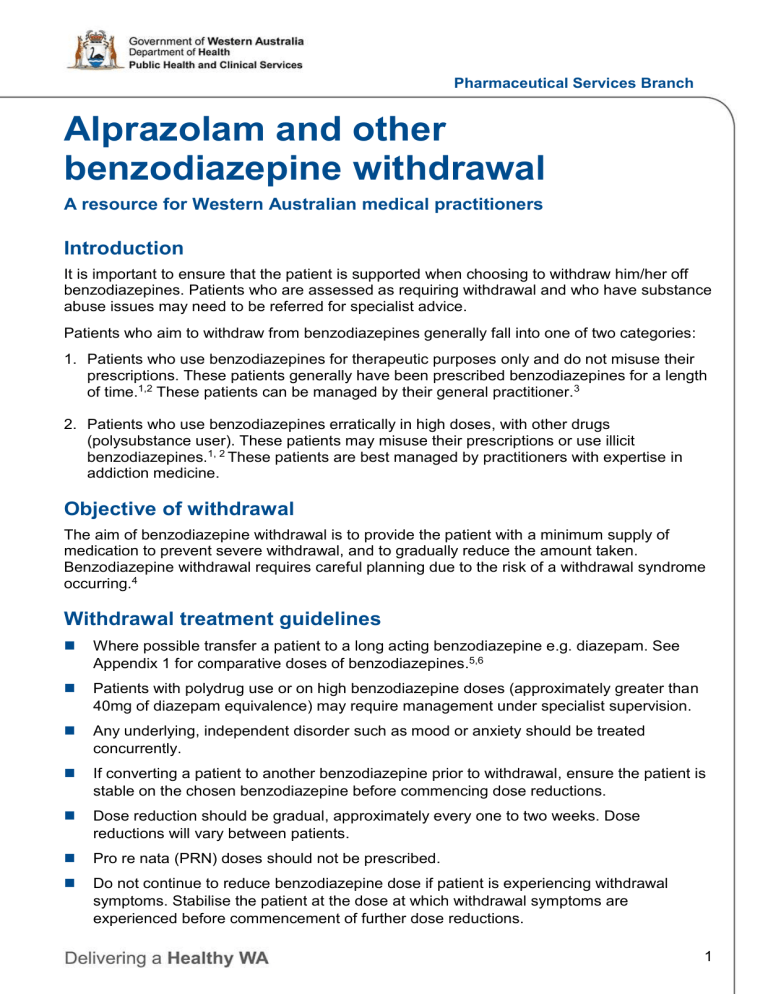
Appendix 1: Comparative doses of benzodiazepines
5, 6
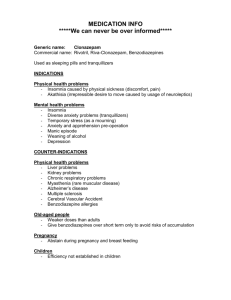
Generic name
Duration of action
Approximate equivalent dose to diazepam 5mg
Trade names
Alprazolam
Bromazepam
Clobazam
Short
Intermediate
Long
0.5mg
3mg
10mg
Alprax, Kalma, Xanax*,
Ralozam
Lexotan
Frisium
Clonazepam Long 0.25mg
Diazepam
Flunitrazepam
Lorazepam
Long
Long
Intermediate
5mg
0.5mg
1mg
Rivotril, Paxam
Antenex, Ducene,
Ranzepam, Valium,
Valpam
Hypnodorm
Ativan
Nitrazepam Long 5mg
Oxazepam
Temazepam
Triazolam
Short
Short
Very short
15mg
10mg
0.25mg
Alodorm, Mogadon
Alepam, Murelax,
Serepax
Normison, Temaze,
Temtabs
Halcion
*Xanax was discontinued from 1 December 2013.
3
Pharmaceutical Services Branch
References and further resources
1. Kenny P, Swan A, Berends L, Jenner L, Hunter B, Mugavin J. Alcohol and Other Drug
Withdrawal: Practice Guidelines Fitzroy, Victoria: Turning Point Alcohol and Drug
Centre; 2009.
2. Lingford-Hughes A, Welch S, Peters L, Nutt D. BAP updated guidelines: evidencebased guidelines for the pharmacological management of substance abuse, harmful use, addiction and comorbidity: recommendations from BAP. Journal of
Psychopharmacology. 2012;0(0):1-54.
3. NSW Department of Health. NSW Drug and Alcohol Withdrawal Clinical Practice
Guidelines. NSW Department of Health ; 2008.
4. Cementon E.Alcohol and Other Drug Withdrawal Practice Guidelines: Acute Inpatient and Residential Services. Melbourne, Victoria: North Western Mental Health; 2011
5. Australian Medicines Handbook. Diazepam: Benzodiazepine withdrawal 2013 [August
12, 2013]. Available from: www.amh.net.au/online/view.php?page=chapter18/monographdiazepam.html#diazepam
6. Therapeutic Guidelines Limited. eTG complete: ‘Benzodiazepines, zolpidem and zopiclone: problem use’ 2013]. Available from www.tg.org.au/index.php?sectionid=71 .
Further reading
National Prescribing Service. Helping patients withdraw 1999 [August 12, 2013].
Available from: http://www.nps.org.au.eplibresources.health.wa.gov.au/__data/assets/pdf_file/0020/157
61/news04_benzodiazepines_0699.pdf
4