INTRODUZIONE

A mio marito Giuseppe, il mio esempio e la mia forza, a mio figlio Edoardo, la mia speranza e il mio orgoglio.
Ai miei genitori, da sempre il mio sostegno morale.
EFFECTS AND TOLERABILITY OF ENDOVENOUS
ADMINISTERED TRAMADOL IN HORSES
Thesis presented to
The Faculty of Veterinary Medicine of University of Camerino by
Dr. Cecilia Vullo
For the degree of Philosophy Doctor
January, 2009
2
3
ABSTRACT
EFFECTS AND TOLERABILITY OF ENDOVENOUS
ADMINISTERED TRAMADOL IN HORSES
Dr. Cecilia Vullo Supervisor
University of Camerino Prof. Paolo Scollavezza
Control of painful conditions is becoming an increasingly important part of veterinary medicine. Many of the available analgesics are considered effective for a variety of painful conditions in horses, but their use may be limited for various reasons. The development of unwanted side effects are a major factor that limits their use. Tramadol has only recently gained significant attention as an analgesic in animals despite its having been used in humans in Germany since 1977.
Tramadol hydrochloride, (1RS,2RS)-2-[(dimethylamino)-methyl]-1-(3methoxyphenyl)-cyclohexanol hydrocloride, is a centrally acting analgesic that has been used clinically for the two decades to treat acute and chronic pain in humans. Tramadol produces its antinociceptive effect in animals and analgesic effect in humans by both opioid and non-opioid mechanism of action. Tramadol is available as a racemic mixture composed of (+) and (-) enantiomers in equal proportions. The racemic mixture produces analgesia by synergistic action of
4 two enantiomers and their main O-desmethylated metabolites (M1). In fact
(+)M1 has been demonstrated to have an affinity to µ-opioid receptors that is
200 times greater than that of the parent compound. On the other hand, the monoaminergic component in tramadol analgesia is mediated by (-)tramadol, by means of an inhibition of the re-uptake of the neurotransmitters serotonina and norepinephrine. The therapeutic use of tramadol has not been associated with significant adverse effects, such as respiratory depression, constipation or sedation, and the drug has been used successfully in humans and many animals to produce analgesia in peri-operative and post-operative periods.
The pharmacokinetics of tramadol have been investigated in several animal species and recently also in horse. After IV administration at a dose of 2.0 mg/kg in only two horses muscle twitching were observed and physical examination revealed decreased gastrointestinal sounds. Moreover, there are two studies that showed good analgesic effect after epidural administration of tramadol to horses without any significant influence on heart rate, respiratory rate, arterial blood pressure, body temperature and behaviour. Caudal epidural administration of tramadol was compared with morphine and both are potential drugs in management of perineal and lumbosacral pain in horse
The purpose of this study was to investigate the effects and tolerability of systemically administered tramadol at two different dosages (1.0 mg/kg EV and
2.0 mg/kg EV) in the horse. Heart rate, respiratory rate, arterial blood pressure, body temperature, central nervous system excitement, head ptosis, arterial pH,
5
PaO
2 and PaCO
2
were measured during 12-hour period and the different was statistically evaluated. Analgesia was not documented.
Results of this study suggest that tramadol con be administered to horse systematically at a dose of 2.0 mg/kg.
6
ACKNOWLEDGEMENTS
L’unica parte di questa tesi che ho scelto di scrivere in italiano sono i ringraziamenti, per timore di trovare qualche difficoltà nell’esprimere in una lingua non mia la gratitudine a chi ha permesso l’espletamento di questo lavoro.
Vorrei innanzitutto ringraziare il mio Tutor e Supervisore, il Prof. Paolo
Scrollavezza, anche se i grazie non saranno mai abbastanza, per avere sempre creduto in me e nelle mie capacità. Spero solo di non averlo in nessuna occasione deluso.
Vorrei poi ringraziare il Dipartimento di Scienze Veterinarie e il Collegio dei
Docenti, in particolare il Coordinatore di questo Corso di Dottorato, il Prof
Giacomo Renzoni, per avermi dato l’opportunità di lavorare con impegno e dedizione in questi tre anni per il completamento di questa tesi. Vorrei ancora ringraziare il responsabile della Sezione Clinica, il Prof. Andrea Spaterna, per la stima professionale che mi ha sempre dimostrato e che mi ha reso serena nello svolgimento quotidiano del mio lavoro.
Un grazie ancora al Prof. Alessandro Valbonesi che con estrema disponibilità mi ha aiutato ad elaborare la statistica dei dati.
E poi un grazie speciale alle studentesse interne, Alessandra ed Annalisa, per essermi state vicine durante il monitoraggio “infinito” degli animali, per avermi aiutato nella raccolta e nella trascrizione dei dati in un momento un po’ particolare della mia vita.
7
Grazie ancora al Dott. Marini e al Dott. Spaziante per avermi fornito gli animali sui quali effettuare la parte sperimentale di questa tesi.
E infine al personale tecnico, in particolare nella figura del Sig. Renato
Ramadori, per essersi reso sempre disponibile soprattutto nei momenti di
“forza”, dove la ragione con i cavalli non riesce purtroppo a prevalere; e infine alla Sig.ra Evelina Serri e alla Dott.ssa Carlotta Marini per aver processato con pazienza tutti i campioni prelevati.
Questa tesi dunque è frutto si del mio lavoro e del mio impegno, ma anche dell’aiuto e dell’incoraggiamento di tutti coloro che mi sono stati vicini, in un modo o in un altro.
REFERENCES
TABLE OF CONTENTS
ABSTRACT
ACKNOWLEDGEMENTS
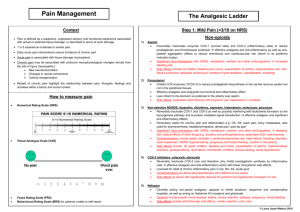
INTRODUCTION: THE PHYSIOLOGY OF PAIN
ANALGESIC DRUGS
PAIN MANAGEMENT IN HORSE
TRAMADOL REVIEW
TRAMADOL: A NEW ANALGESIC DRUG IN VETERINARY MEDICINE
TRAMADOL IN HORSE
SPERIMENTAL STUDY
STATISTICAL ANALYSIS
8
9
INTRODUCTION: THE PHYSIOLOGY OF PAIN
As veterinarians, it is essential that we have a good knowledge and understanding of animal pain. For many years, clinicians lacked information on analgesic agents and their use in animals, and our attempts at pain were rudimentary. In recent years there has been a rapid increase in information on analgesic agent, but use of them remains low in comparison to their use in man
( Flecknell and Waterman-Pearson, 2000 ).
Important advances have occurred in the study of pain after the IASP
(International Association for the Study of Pain) Committee for Taxonomy that defined pain “as unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” ( IASP,
1979 ). The inability to communicate is no way negates the possibility that an individual is experiencing pain and is in need of appropriate pain relieving treatment ( Helley et al., 2007 ).
The last 20 years have seen significant scientific advancement in our understanding of the physiology, pathophysiology and pharmacology of pain
( Kelly et al., 2001 ). Both the peripheral and the central nervous system (CNS) are involved in the perception of pain, with the spinal and supraspinal components of CNS playing key roles ( Kehelet and Dahl, 1993 ). The transduction of noxious stimuli begins with peripheral nociceptors. Each receptor is specialized to detect a particular type of stimulus (e.g. touch,
10 temperature, pain, etc.). Signals from these nociceptors travel primarily along two distinct types of neurons, small myelinated A and unmyelinated C fibres with soma lying in the dorsal root ganglion. This is the first major site where chemical neurotransmitter agents are involved in the propagation of ongoing impulses and is thus important as a site of drug action. After synapsing within the superficial layers of the dorsal horn, the noxious signal travel along the spinothalamic and spinoreticular tracts of spinal cord to the thalamus and the cortex ( Gottschalk and Smith, 2001 ). These higher centres are responsible for the perception of pain and the emotional components that accompany it.
Therefore there are four distinct processes in the sensory pathway: transduction
(nociceptors respond selectively to noxious stimuli and convert chemical, mechanical, or thermal energy at site of the stimulus into neural impulses), transmission (impulses are transmitted via A-delta and C fibres to the dorsal horn of the spinal cord), perception (from the thalamus afferent information is carried to the somatosensory cortex; the impulses transmitted via these tracts are responsible for the sensory discrimination of pain and the emotional responses it evokes) and modulation (some efferent descending pathways can modulate nociceptive transmission in the periphery, in the spinal cord by altering neurotransmitter release, or supraspinally by activation of inhibitory pathways).
Each of these processes presents a potential target for analgesic therapy ( Kelly et al., 2001 ).
11
Painful stimuli ultimately cause activity in both the somatotopically appropriate portion of the sensory cortex and the limbic system ( Rainville et al., 1997 ). One of the best described intrinsic control mechanisms occurs in afferent pain transmission at level of spinal cord. This is the “gate theory” as first proposed by
Melzack and Wall in 1965 which proposed that the signal passed up to the brain is a summation of the excitatory and inhibitory inputs. The purpose of this mechanism may be to prevent the animal being totally overwhelmed by a particularly intense pain and thereby facilitating survival by allowing some form of escape behaviour ( Fields, 1988 ). The process through which the neurons of the dorsal horn of the spinal cord become sensitized by prior noxious stimuli is often referred to as “wind-up” or “central sensitization”, an activity dependent increase in the excitability of spinal neurons. This state manifests as an increase in the response to noxious stimuli and a decrease in the pain threshold ( Willis
1986; Gottschalk and Smith, 2001 ). One of the most critical observations concerning central sensitization is the role played by the first phase of pain response ( Dickenson and Sullivan, 1987 ). After the afferent fibres enter the brain they again synapse at a variety of levels, of which the thalamus is thought to be most important. Some of the ascending fibres terminate in the reticular formation, which is thought to govern consciousness and level of sleep. A practical consequence of this is that increased reticular activity produced by increased noxious input can overcome the effects of general anaesthetics
( Flecknell and Waterman-Pearson, 2000 ). The demonstration that electrical
12 stimulation of particular regions of the brain could produce analgesia ( Reynolds,
1969; Mayer and Liebeskind, 1974 ) led to the concept that animals had an intrinsic pain control system which produced a descending inhibition of pain perception. This concept has allowed not only a much better understanding of action of analgesia drug but also an improved understanding of how pain perception is modulated internally ( Basbaum and Fields, 1984; Fields, 1988 ).
Also of interest for the pharmacological approach to pain control is the wide range of neurotransmitter agents involved in the synapses between the CNS centres, including glutamate, noradrenaline, 5-hydroxytryptamine (5-HT, serotonin), γ-aminobutyric acid (GABA) and endogenous opioid peptides
( Basbaum and Fields, 1984 ).
Studies now indicate that pain also can cause changes in brain and spinal cord neurones that result in a heightened perception of pain after a period of stimulation (hyperalgesia). Primary hyperalgesia refers to receptor field changes within the area of injury, while secondary hyperalgesia refers to changes in the undamaged tissue surrounding the area of injury. In addition, these changes are responsible for the misperception of pain in response to non-noxious stimuli, termed allodynia ( Woolf and Chong, 1993 ).
The central sensitisation to pain and the fact that is easier to prevent it using analgesic drugs given before the pain starts (preemptive analgesia) than to treat the subsequent hyperalgesia, now seems to be well established ( Lascelles et al,
1994; 1995 ). In fact laboratory and clinical studies have shown that a state of
13 altered central processing can occur in response to peripheral injury ( Coderre et al. 1993 ). This “central hypersensitivity” results in a modified response to subsequent afferent inputs which lasts between 10 and 200 times the duration of the initiating stimulus ( Woolf and Chong 1993 ). Pre-injury treatment with opioids ( Woolf and Wall 1986; Dickenon and Sullivan 1987 ) or local anaesthetics ( Coderre et al. 1990 ) prevents or markedly decreases the development of central hypersensitivity ( Woolf and Wall 1986; Dickenson and
Sullivan 1987 ) and behavioural indicators of pain ( Coderre et al. 1990 ), but these treatments are far less effective if administered after the injury is initiated
( Woolf and Wall 1986; Dickenson and Sullivan 1987; Coderre et al. 1990;
Chapman and Dickenson 1993 ). Clinically, it has been reasoned that by preventing the surgical afferent barrage from entering the spinal cord one can prevent the facilitation of spinal nociceptive processing that occurs and, thus, markedly decrease the severity of post-operative pain ( Wall 1988; Woolf 1989 ).
The physiological mechanism of central sensitisation is complex and occurs within both the spinal cord and brain. Excitatory amino acids, such as glutamate
(the major excitatory neurotransmitter in CNS) and aspartate, acting at the Nmethyl-D-aspartate (NMDA) receptor sites, are probably the main transmitters involved. This receptor is intimately involved in the induction and maintenance of altered pain responses following trauma/inflammation ( Woolf and Chong,
1993 ).
14
There are many other physiologic responses which occur after a noxious stimulus. The autonomic reflexes are well documented and include such things as heart rate and blood pressure changes, alterations to respiratory rate and pattern, sweating, piloerection, gut motility and many others. These indicators of pain are often used in animals as marked for pain intensity and analgesic efficacy. All of the changes listed can be induced or modified by stress-related endocrine activity, drugs or external physical effects, and to use them as sole indicators of presence or otherwise of pain is very unwise. Similarly, pain or injury can cause profound endocrine changes and release of hormones from the pituitary, thyroid, parathyroid and adrenal glands and possibly other endocrine organs as well. Like the autonomic reflexes, these responses can be very unreliable indicators of pain although they are commonly used as such in animal studies ( Morgan et al, 1987 ).
Behavioural changes can be considered as the “overall integrated physiological response” to pain. Since they constitute an integrated response, they are obviously complex, difficult to interpret and difficult to quantify, but for pain evaluation in animals, they are perhaps the most useful observation. It is important to realise that alteration of behavioural changes with drugs is not the same thing as analgesia. This is particularly relevant with the sedative drugs which can have a profound effect on behaviour without altering pain perception
( Flecknell and Waterman-Pearson, 2000 ).
15
One of the most critical observations concerning central sensitization is the role played by the first phase of pain response. The definitions of preemptive analgesia were formulated by Crile ( Crile, 1913; Crile and Lower, 1914 ) and have recently been reviewed by Kissin ( Kissin, 1996; 2000 ). Preemptive analgesia is an antinociceptive treatment whose aim is to prevent both peripheral and central sensitization, thereby attenuating (or, ideally, preventing) the postoperative amplification of pain sensation. It prevents establishment of central sensitization caused by incisional and inflammatory injuries; it starts before incision and covers both the period of surgery and the initial postoperative period ( Woolf and Chong, 1993; Kats, 1995 ). Preemptive analgesia strategies have involved intervention at one or more sites along the pain pathway. Treatment can be aimed at the periphery, at inputs along sensory axons, or at CNS sites using single or combination of analgesics (multimodal approaches) applied either continuously or intermittently ( Kehlet and Dahl,
1993 ). These strategies have included infiltration with regional anaesthesia, nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, NMDA receptor antagonists, alfa2 adrenoceptor antagonists, miscellaneous drugs (nitrous oxide,
GABA agonists, antagonists to bradykinin, histamine and serotonin) ( Kelly et al,
2001 part I and II ). Balanced or multimodal analgesia results from the administration of analgesic drugs in combination and at multiple sites to induce analgesia by altering more than one part of the nociceptive process. When multimodal analgesia is used, does of individual drugs can be reduced, thereby
16 decreasing the potential for any one drug to induce adverse side effects.
Balanced analgesic techniques appear to offer several advantages in the management of postoperative pain ( Tranquilli et al., 2007 ).
17
ANALGESIC DRUGS
Analgesia in the strictest sense is an absence of pain but clinically is the reduction in the intensity of pain perceived. Analgesics consist of those classes of drugs whose primary effect is to suppress pain or induce analgesia ( Tranquilli et al., 2007 ).
Analgesic drugs may be divided into six main classes:
1.
Local anaesthetics
2.
Non-steroidal anti-inflammatory drugs (NSAIDs)
3.
Opioids
4.
Alpha2 adrenoceptor agonists
5.
NMDA receptor antagonists
6.
Miscellaneous drugs
LOCAL ANAESTHETICS
These drugs act to decrease or prevent the large transient increased in the permeability of excitable membranes to Na+ that normally occurs when the membrane is slightly depolarised ( Butterworth and Strichartz, 1990 ). Thus, they stop the transfer of noxious information from the periphery along peripheral nerves. Aδ fibres are most susceptible to blockade followed by C fibres and then by large myelinated fibres. Pain is thus the first sensation to be abolished. The duration of action of a local anaesthetic is dependent on time that the drug is in
18 contact with the nerve, which is governed by the lipid solubility of the drug, the blood flow to the tissue and the pH of the tissue. Paradoxically, in the central nervous system local anaesthetics drugs induce stimulation, restlessness and convulsions, which are ultimately followed by depression. Local anaesthetics also act on the myocardium to decreased electrical excitability, conduction rate and force of contraction. They may also induce arteriolar dilatation which results in hypotension. Local anaesthetic drugs are used topically, by local infiltration direct into wound edges, by injection to abolish sensation in a body region, by epidural injection or by intravenous injection. Local anaesthetics are used to provide complete analgesia to allow surgical procedures to be performed in the conscious or sedated animal. The agents most commonly administered in veterinary anaesthesia are Lidocaine, Bupivacaine, Mepivacaine and
Ropivacaine. The clinically important properties of the local anesthetics include potency, speed of onset, duration of anesthetic action, and differential sensory/motor blockade. The clinically observed rates of onset and recovery from blockade are governed by the relatively slow diffusion of local anesthetic molecules into and out of the whole nerve ( Ilkiw, 2001 ). Lidocaine is a shortacting drug with a rapid onset of action and maximum duration of action of approximately 0.75-1 h. Bupivacaine is a long-acting drug with a slow onset time and the duration of action varies from 2-6 h. It is more cardiotoxic than equieffective doses of lidocaina. Mepivacaina is a local anaesthetic drug that widely used in equine medicine. It has duration of action similar to lidocaine.
19
Ropivacaine has a similar onset time and duration of action of bupivacaine but it has a greater margin of safety ( Flecknell and Waterman-Pearson, 2000 ).
NON-STEROIDAL ANTI-INFLAMMATORY DRUGS (NSAIDs)
Several non-steroidal anti-inflammatory drugs (NSAIDs) have been now employed to successfully control post-operative pain in animals. One mode of action of NSAIDs in conferring analgesia is through reduction in prostaglandin
(PG) synthesis via inhibition of cyclooxygenase (COX)-1 (homeostatic or constitutive) or COX-2 (inflammatory or inducible) isoenzymes, or both. Under normal circumstances, PGs synthesized as a result of COX-1 activity, serve to maintain physiologic functions such as gastric mucosal integrity, modulation of renal blood flow, and platelet function. Following tissue injury, activation of the
COX-2 isoform leads to the production of PGs which act as mediators of inflammation, causing hyperalgesia and pain. The differential inhibition of these two COX isoforms by NSAIDs is thought to result in not only the excellent antiinflammatory and analgesic benefits of these agents, but in the potential for adverse effects under certain conditions. Thus, the development of NSAIDs that preferentially inhibit COX-2 over COX-1 may provide safer analgesics
( Mathews, 2001 ). COX-2 has been identified in fibroblasts, chondrocytes, endothelial cells, macrophages, and mesangial cells. COX-2 is induced by exposure to various cytokines, mitogens, and endotoxin, and it up-regulated with inflammation. The prostaglandins produced in the gastrointestinal tract and the
20 kidneys that maintain mucosal integrity in the GI tract and renal perfusion appear to be derived from COX-1. Therefore, suppressing COX-1 activity by
NSAIDs is believed to be critical to the development of toxicity. It is suggested that COX-2 selective NSAIDs would suppress prostaglandin synthesis at sites of inflammation but would spare constitutive prostaglandin synthesis in the GI tract and kidney. The currently available NSAIDs vary in their potency as inhibitors of COX-2, but virtually all are far more potent inhibitors of COX-1 than COX-2.
The pharmaceutical companies are racing to develop COX-2 selective NSAIDs, but this may not be the perfect solution. If COX-2 is primarily responsible for the prostaglandins that mediate pain, inflammation and fever, it is unlikely that
COX-2 selective drugs will be more therapeutically effective, because the available NSAIDs are already very effective inhibitors of COX-2. It is still possible that COX-1 prostaglandins contribute to pain, inflammation, and fever; so COX-2 selective NSAIDs could be less effective. In addition, COX-2 may produce beneficial prostaglandins; therefore, highly selective COX-2 inhibitors may produce adverse reactions not seen with existing NSAIDs. NSAIDs primarily are anti-inflammatory due to their inhibition of prostaglandin production. Some anti-inflammatory action appears to be related to their ability to insert into the lipid bilayer of cell and disrupt normal signals and proteinprotein interactions in cell membranes. NSAIDs are more lipophilic at a low pH, such is found in inflamed tissues. In the cell membrane of neutrophils, NSAIDs inhibit neutrophil aggregation, decrease enzyme release and superoxide
21 generation, and inhibit lipoxygenase. The time to onset and duration of analgesic properties of NSAIDs does not correlate well with their anti-inflammatory properties. The analgesic effect is likely to have a more rapid onset and shorter duration of action. Therefore, dosage regimens for effective analgesia may need to be different than for anti-inflammatory properties ( Dowling, 2001 ).
OPIOIDS
All opioid analgesics are chemically related to a group of compounds that have been purified from the juice of a particular species of poppy: Papaverum somniferum . The word opioid is used broadly to cover all drugs that are chemical derivatives of the compound purified from opium. Exogenously administered of opioids exert their effects by interacting with specific opioid receptors and mimicking naturally occurring molecules known as endogenous opioid peptides ( Tranquilli et al., 2007 ). Opioids act on at least three different opioid receptors: mu (μ), kappa (k) and delta (δ) receptors. Each receptor is distributed differently throughout the CNS. High densities of opioid receptors are found in areas of the central CNS associated with the processing of nociceptive information in all species studied. Opioid receptors are also found throughout the periphery and here they mediate opioid effects such as decreasing gastrointestinal motility. In general, it appears that the μ receptor mediates most of the clinically relevant analgesic effects, as well as most of the adverse side effects associated with opioid administration ( Kieffer, 1999 ).
22
Opioids drugs may be classified according to their receptor selectivity and may be active at one, two or all of the receptors. The differences in drug receptor selectivity confer discrete properties on individual drugs and will help predict the pharmacological properties of given drug in an individual animal species.
Opioids are also categorised as pure agonists (e.g. morphine, pethidine, methadone, fentanyl, alfentanyl), partial agonists (buprenorphine), mixed agonist-antagonists (butorphanol), or antagonists (naloxone, nalmefene), who describes their ability to induce a maximal response irrespective of the dose administered ( Flecknell and Waterman-Pearson, 2000 ). It has been well established that the analgesic effects of opioids arise from their ability to directly inhibit the ascending transmission of nociceptive information from the spinal cord dorsal horn, and to active pain-control circuits that descend from the midbrain to the spinal cord ( Gutstein and Akil, 2001 ). Systemic administration of opioid analgesics via intravenous, intramuscular, or subcutaneous injection will induce a relatively rapid onset of action via interaction with these CNS receptors. Oral, transdermal, rectal, or buccal mucosal administration of opioids will result in variable systemic absorption, depending on the characteristics of the particular agent, with analgesic effects being mediated largely by the same receptors within the CNS ( Glare, 1997 ).
Low-potency opioids such us butorphanol and buprenorphine are said to produce a “ceiling effect” in which higher doses of drug do not increase the level of analgesia because all of receptors are occupied Pure agonist opioids are
23 extremely safe analgesic because their duration is short-lived and side effects can simply be managed by decreasing the dose. If needed, opioids can be reversed with antagonists, such as naloxone or naltrexone, or partially reversed with agonist/antagonist such butorphanol ( Welch, 2005 ). Although opioids are used clinically primarily for their pain-relieving properties, they also produce a host of other effects on a variety of body system, in light of the wide distribution of endogenous opioid peptides and their receptors in supraspinal, spinal, and peripheral locations. Some of these effects may be classified as either desirable or undesirable depending on the clinical circumstances ( Stein, 1993 ).
Opioid drugs cause respiratory depression by decreasing the responsiveness of the respiratory centre to carbon dioxide ( Florez et al, 1968 ). Opioids may alter respiratory rate, rhythmicity and pattern, and minute volume. In general, breathing rate is slowed but tidal volume is unaffected ( Nolan and Reid,
1991 ).The effects of opioid drugs on the cardiovascular system are related to their action on opioid receptors located in the brainstem, causing inhibition of sympathetic tone to the heart. Opioids such codeine, morphine, and butorphanol are well known antitussive drugs ( Bolser, 1996 ). Opioids active at the μ receptor generally induce euphoria while k receptor activation is associated with dysphoria ( Simonin et al., 1998 ) Opioids reduce the propulsive activity of the gastrointestinal tract ( Kromer, 1988 ). Smooth muscle and sphincter tone tend to be increased, but peristalsis is decreased. Morphine induces vomiting by activating the chemoreceptal trigger zone, but appears to be only opioid which
24 induces vomiting in dogs and cats. Butorphanol has show specific antiemetic activity in humans and dogs ( Moore et al., 1994 ). Opioids in general decreased motor activity, but horse show increased locomotor activity when given opioid drugs, and other behaviours such as compulsive eating behaviour and agitation.
Many of these effects are reduced when opioids are used in combination with the tranquilliser acepromazine or alpha2 adrenoceptor agonist sedative ( Nolan and Hall, 1984 ).
ALPHA2 ADRENOCEPTOR AGONISTS
Alpha2 agonists are the most widely used class of sedative in veterinary medicine. These drugs induce reliable dose-dependent sedation, analgesia, muscle relaxation and anxiolysis that can be readily reversed by administration of selective antagonists ( Tranquilli et al., 2007 ). These drugs, xylazine, medetomidine, dexmedetomidine, detomidine and romifidine, produce analgesia by binding to alpha2 receptors present in the CNS. Alpha2 adrenoceptors are located in structures closely related to pain information processing within the brain and spinal cord and in other tissues throughout the body ( Nolan et al.,
1987
). Alpha2 agonists exert their sedative effects through stimulation of α2adrenoceptor in the brain, decreasing norepinephrine release. Sedation results from decreased activity of ascending neural projections to the cerebral cortex and limbic system ( Martin et al., 1984; Stenberg, 1986 ). Analgesia appears to be
25 the results of both cerebral and spinal effects, possibly in part mediated by serotonin and the descending endogenous analgesia system ( Lewis et al., 1983 ).
In addition to having profound sedative and analgesic activity, α2-agonists induce cardiovascular and metabolic responses also related to their peripheral adrenergic effects. The most common side effect noted is an initial hypertension
(due to peripheral postsynaptic adrenoreceptors causing vasoconstriction), which results in a baroreceptor-mediated reflex bradycardia. As the peripheral effects diminish, central alpha-2 actions predominate, leading to decreased blood pressure and cardiac output ( Klide et al., 1975 ). Anticholinergics have been advocated to reduce the bradycardic effects, but their use is controversial
(elevating heart rate in the presence of high systemic vascular resistance can result in increased cardiac workload and myocardial oxygen consumption).
Other side effects can include short term A-V block (most often first or second degree), sinus arrhythmia, sinoatrial block, decreased respiratory rate, peripheral venous desaturation (resulting in a cyanotic appearance to the mucous membranes), vomiting, increased urine output, transient hyperglycemia (due to inhibition of insulin secretion) and increased myometrial tone and intrauterine pressure ( Thurmon et al., 1984; Benson et al., 1984 ). Additionally, xylazine has been associated with the development of aerophagia, gastric dilatation, gastric reflux and cholinergic bradycardia. Following their administration, urinary output is increased as a result of decreased arginine vasopressin release and decreased water reabsorption by nephrons ( Thurmon et al., 1984; Greene and
26
Thurmon, 1988 ). At low doses, both the sedative and analgesic effects of alpha-
2 agonists are dose-dependent. As the dose is increased, there is a ceiling on the degree of analgesia, and further dosing only acts to lengthen the duration of sedation and increase the risk of adverse effects. While xylazine still enjoys popularity in equine and food animal medicine, medetomidine has replaced xylazine in dogs and cats as the alpha2 of choice, due to its greater alpha2:alpha1 affinity (approximately 1620:1 for medetomidine, vs. 160:1 for xylazine). This increased selectivity results in more predictable and effective sedation and analgesia and fewer side effects ( Gaynor and Muir, 2008 ).
NMDA RECEPTOR ANTAGONISTS
Pain is detected by two different types of peripheral nociceptor neurons, C-fiber nociceptors with slowly conducting unmyelinated axons, and A-delta nociceptors with thinly myelinated axons. During inflammation, nociceptors become sensitized, discharge spontaneously, and produce ongoing pain.
Prolonged firing of C-fiber nociceptors causes release of glutamate which acts on N-methyl-D-aspartate (NMDA) receptors in the spinal cord. Activation of
NMDA receptors causes the spinal cord neuron to become more responsive to all of its inputs, resulting in central sensitization. NMDA-receptor antagonists, such as ketamina or dextromethorphan, can suppress central sensitization in experimental animals. NMDA-receptor activation not only increases the cell's response to pain stimuli, it also decreases neuronal sensitivity to opioid receptor agonists. In addition to preventing central sensitization, co-administration of
27
NMDA-receptor antagonists with an opioid may prevent tolerance to opioid analgesia ( Anis et al., 1983 ).
More recently, antagonist of the NMDA receptor has been proposed as the most likely molecular mechanism responsible for most of the anaesthetic, analgesic, psychotomimetic, and neuroprotective effects of the drug ( Kohrs and Durieux,
1998 ).
Ketamine is a non-competitive antagonist of the NMDA receptor. Ketamine is presented as a mixture of isomers and there is some evidence to suggest that the
R(-) isomer is associated with excitatory effects while the S(+) isomer is associated with pain modulating effects ( Flecknell and Waterman-Pearson,
2000 ).
Classic ketamina anaesthetic effects are best described as a dose-dependent CNS depression that leads to a so-called dissociative state, characterized by profound analgesia and amnesia but not necessarily loss of consciousness. Suggested mechanisms for this form of catalepsy include electrophysiologic inhibition of thalamocortical pathways and stimulation of the limbic system Ketamine has other effects beside analgesia and amnesia: it is a bronchodilator; it produces significant increases in blood pressure and heart rate. These effects are due to sympathetic stimulation ( Kohrs and Durieux, 1998 ). Ketamine’s neuropharmacology is complex. The compound interacts with multiple binding sites, including NMDA and non-NMDA glutamate receptors, nicotinic and muscarinic cholinergic, and monoaminergic and opioid receptors. In addition,
28 inhibition of neuronal Na channels provides a modest local anaesthetic effect, whereas Ca channel blockade may be responsible for cerebral vasodilatation
( Wong and Martin, 1993 ).
At small doses (0.1-0.5 mg/kg), ketamine has a noticeable analgesic action, which can be used to supplement regional or local anesthesia. A number of studies have suggested that administration of ketamine before the noxious stimulus occurs is even more effective ( Tverskoy et al., 1994; Wong et al.,
1996 ). This effect is referred to as preemptive analgesia. The goal of preemptive analgesia is to prevent or reduce the development of a “memory” of the pain stimulus in the nervous system ( McQuay, 1992; Wall, 1988 ). When a massive barrage of afferent nociceptive impulses reaches the spinal cord, a hyperexcitable state of CNS sensitization known as wind-up results ( Wall,
1988 ). NMDA receptors seem to be responsible for pain memory and their blockade can contribute significantly to the prevention of pain. NMDA antagonists prevent the induction of central sensitization and even abolish hypersensitivity once it is established ( Woolf, 1991 ). Preoperative (preemptively) administered ketamine seems to reduce the amount of narcotics required postoperatively for pain control ( Fu et al., 1997 ).
Ketamina may have neuroprotective and even neuroregenerative effects
( Himmelseher et al., 1996 ). It seems confirmed that ketamine does not increased
ICP when the blood pressure is controlled and mild hypocapnia is achieved.
Thus, the contraindication for ketamine use in neurosurgical patients is only a
29 relative one, and when further preclinical and clinical studies confirm a neuroprotective effect of the compound, ketamine may well find a place in the neuroanaesthesiology drug cart. Finally, the analgesic properties of small-dose ketamine have been rediscovered. The preventive administration of ketamine can have profound effects on postoperative analgesic requirements ( Fu et al.,
1997 ) with minimal risk and side effects. This provides the anaesthesia practitioner with another useful tool in the management of preoperative pain
( Kohrs and Durieux, 1998 ).
Ketamine may have a role as an analgesic at low doses in cats and it has been used with good success to suppress responses to surgical stimulation in horses during anaesthesia, and by intravenous infusion in horses ( Nolan et al., 1997 ) and perioperatively in dogs ( Lerche et al., 2000 ).
MISCELLANEOUS DRUGS
Nitrous oxide, a gas delivered to the patient by inhalation, is a good analgesic in humans, and it is used routinely to provide analgesia during surgery and anaesthesia. It has low potency in domestic animals; however, when administered at a concentration of 60-70% it appears to have some analgesic proprieties. It is used as an adjunction to inhalational or intravenous anaesthesia; it does not provide lasting analgesia and once administration of nitrous oxide is
30 discontinued the effects wane rapidly (within 5 min) ( Flecknell and Waterman-
Pearson, 2000 ).
In conclusion, better pain management can be provided with the use of current available analgesic drugs by more selective routes of administration (epidural, intra-articular, transdermal patch), by methods that maintain more steady plasma concentrations (CRIs), and with the combination of different pharmacological analgesic groups and techniques rather than single drug usage. Understanding the drugs’ mechanism and site of action is important in selecting the best individual drug or combination of drugs for specific pain situations where relief is necessary for short to extended periods of time without compromising the animal’s well being. Special attention should be given to possible adverse effects of these drugs and doses should be adjusted to the patient’s needs when different pharmacological groups are combined.
31
PAIN MANAGEMENT IN HORSE
Equine analgesia has been a neglected subject until relatively recently, lagging behind progress in small animal. However, the need for good analgesia in horses, particularly perioperatively, is now acknowledged. A horse in pain is usually agitated and likely to cause more damage than a calm animal with good pain management, given physical support to the injury. A horse with wellcontrolled pain that is not depressed will eat readily; adequate energy intake is essential for normal functioning of the immune system and tissue healing
( Taylor, 2003 ). Difference in behaviour between the different species of large animal will also impact the way in which the animal respond to pain, as well as how it should be approached by the clinicians ( Valverde and Gunkel, 2005 ).
Behaviour is generally acknowledged as the best way to asses pain in animals, but attempts to develop any system for horses suffering from clinical pain have been extremely limited ( Raekallio et al., 1997 ). Horses undergoing surgical procedures to correct traumatic/functional conditions represent a special group of patient because of their instinctive flight response to stressful situations.
Providing adequate analgesia to the animal represents one very important step in making the animal comfortable and improving outcome ( Valverde and Gunkel,
2005 ).
Horses frequently require analgesic medication for a variety of soft tissue and orthopaedic diseases. Inflammation is a major component of injury and pain.
32
Therefore, NSAIDs, such as flunixin phenylbutazone and ketoprofen, are the most commonly used analgesics in horses as a part of balanced analgesic technique, because of their inhibitory actions on the cyclo-oxygenase enzyme
(COXs) necessary for prostaglandin production during the inflammatory response. In horses, NSAIDs are used primarily for musculoskeltal injury and to relieve or reduce abdominal pain ( Moses and Bertone, 2002 ). Because of the potentially serious adverse effects, including gastric ulceration, right dorsal colitis, renal impairment and weight loss, many clinicians attempt to minimize the dose administered, possibly at the expense of maintaining adequate analgesia
( McCallister, 1993; Cohen et al., 1995; Sellon et al., 2001 ). Unlike other analgesic drug, plasma concentrations of NSAIDs are not always correlated with analgesic effects. Even when no drug con be detected in plasma, their concentrations at the tissue level may be sufficient to cause an antiinflammatory effect that contributes to analgesia ( Valverde and Gunkel, 2005 ).
The indications for their use include inflammatory conditions, pain, fever, endotoxemia, and thrombosis. Under these conditions, the effects of NSAIDs are beneficial in reducing patient morbidity and improving the clinical disease. It is important to remember that under certain conditions, particularly stress and dehydration, these drugs can have serious side effects, including gastrointestinal ulceration and renal disease. These effects are caused by inhibition of COX-1 isoenzyme. Patients being given these drugs should be closely monitored for signs of toxicity ( Moses and Bertone, 2002 ).
33
Opioid are the mainstay of pain management in most species, but are associated with unwanted side effects in horses. Opioids cause dose-dependent increase in muscle tone and locomotor activity in horses and are known to increase segmental intestinal contraction, but the net effect of their action on the gastrointestinal tract is constipation, because they cause a prolonged overall depression of intestinal propulsion ( Davies and Gerring, 1983 ). Opioids commonly cause an increase in sympathetic stimulation and resulting increases in heart rate, arterial blood pressure, and cardiac output ( Kalpravidh et al., 1984;
Szoke et al., 1998 ). Respiratory depression (as evidence by an increased in
PaCO2) is generally considered a regular side effect of opioid use, but in horses is quite variable, and results appear strongly related to either the opioid is administered alone or in combination with other drugs ( Bennet and Steffey,
2002 ). The analgesic potency of opioids in horses is not readily quantifiable, however, it is generally accepted that if pain is present, these side effects are less commonly observed. Agonist of the μ receptor (morphine, fentanyl, meperidine) are considered better in controlling orthopaedic pain than k-agonist
(butorphanol). Butorphanol, a narcotic agonist-antagonist (μ receptor antagonist and k-receptor agonist), is the most widely used opioid in equine practice and it has been recommended for superficial and visceral pain relief. It is commonly given as a single, repeated IV dose. Used alone, butorphanol can result in ataxia, increased locomotor activity and excitement. Reported gastrointestinal effects include decreased defecation and reduced borborygmi. Because of these adverse
34 effects and its brief duration of action (30-90 min), butorphanol is rarely administered to horses alone but is commonly used in combination with α2 agonist for short term sedation and analgesia ( Valverde and Gunkel, 2005;
Sellon et al., 2001 ). In a review of opioid use for pain management bin horses,
Bennet and Steffey (2002) concluded that systematically administered opioids do not consistently and effectively relieve pain in horses. A combination of opiates and NSAIDs probably achieves greater pain relief postoperatively than either medication alone ( Kehlet, 1994 ). Combination drug therapy, include alpha2 adrenergic agonist, has the additional benefit of minimizing the risk of adverse effects from either class of drugs, because lower doses of each drug can be administered ( Sellon et al., 2001 ). The use of opioids by the epidural route
(fist coccygeal or sacrococcygeal interspace) has been described in the horse
( Valverde et al., 1990; Sysel et al., 1996; Sysel et al., 1997; Doherty et al., 1997;
Natalini and Robinson 2000; Goodrich et al., 2002; Robinson and Natalini,
2002; George, 2004 ). Initially, deposition of opioids into the epidural space of the horse produced signs of profound analgesia. More recently, placement of epidural catheters has gained wider acceptance in horses and has permitted the administration of multiple injections of analgesics and anaesthetics for long durations of pain control ( Valverde et al., 1990; Robinson and Natalini, 2002 ).
The clinical use of opioids for epidural analgesia in horses can be recommended for acute and chronic pain control of the rear limb, perineum, tail and abdominal wall ( Robinson and Natalini, 2002 ). There is mounting evidence that opioids can
35 produce potent analgesic effects by interacting with opioid receptors in peripheral tissue. When compared with other epidurally administered drugs, opioids present advantages over local anaesthetic and alpha2 agonist because motor impairment or sympathetic blockade do not occur with their use
( Stoelting, 1989 ). Opioid receptor have been also identified in equine synovial membranes ( Sheehy and al., 2001 ) and results of these efforts encourage further objective study to assess the degree of analgesia resulting from intra-articular administration of opioid to relieve joint-associated pain in horses ( Bennet and
Steffey, 2002 ).
The alpha2 agonist drugs, including xylyzine, detomidine, romifidine and medetomidine, provide analgesia by stimulating opiate or alpha2 adrenergic receptors, or by altering prostaglandin synthesis ( Daunt and Steffey, 2002 ).
Alpha2 agonist receptor are located in the CNS and periphery, therefore, parental and epidural administration have been used. In the meantime, administration of alpha2 agonist to produce excellent analgesia in horses
( England and Clarke, 1996; Owens et al., 1996; Bettschart-Wolfensberger et al.,
1999; Bettschart-Wolfensberger et al., 2001 ) will be associated with unwanted side effect. It is common practice to combine alpha2 agonist with opioids because of the perception that the combination produces better sedation and analgesia than when each agent is administered alone ( Nolan and Hall, 1984;
Muir et al., 1979 ). Alpha2 adrenergic agonists were the first reported class of agents that significantly and consistently reduce inhalation anaesthetic
36 requirements in horses. These results are in contrast to the opioids that not induce a consistent sparing effect on the minimum alveolar concentration
(MAC) of any inhalant anaesthetic ( Doherty et al., 1987; Matthews and Linsday,
1990; Steffey et al., 2003 ). Use of medetomidine as a CRI (constant rate infusion) has been described for standing sedation in horses ( Bettschart-
Wolfensberger et al., 1999 ) and in a recent clinical trial in horses undergoing different types of surgical procedure and administered medetomidine as a part of pre-medication followed by a CRI during general anaesthesia, 20% less inhalant anaesthetic was required than in horses that received xylazine and no CRI
( Neges et al., 2003 ). Alpha2 agonists have also been administered by the subaracnoid or caudal epidural route to produce perineal analgesia ( LeBlanc et al., 1988; Fikes et al., 1989 ). The use of alpha2 agonists has become popular for caudal epidural analgesia in horses due to the longer duration of activity than most local anaesthetic. Administration of alpha2 agonist into the sacrococcigeal epidural space can provide significant perineal analgesia while reducing some of side effects associated with intravenous or intramuscular delivery. These drugs do not produce motor blockade, thus horses remain standing, even if the analgesic effect spreads cranially into the lumbar and thoracic area ( Robinson and Natalini, 2002 ). However, ataxia and recumbency are still possible complications of this group of drugs in individual horse ( Wittern et al., 1998 ).
Alpha2 agonists are potent sedative-hypnotics. Following IV injection, profound sedation occurs in two to five minutes. Sedation is dose-dependent and
37 characterized by somnolence, lowering of the head, drooping of the lower lip, ataxia, and leaning ( Daunt and Steffey, 2002 ). Alpha2 agonist administration produces a dose-dependent decrease in heart rate and especially increases the frequency of second-degree atrioventricular block ( Wagner et al., 1991 ).
Systemic blood pressure usually increases transiently following IV injection and then is mildly reduced from baseline. Cardiac output and likely tissue perfusion are reduced due to the reduction in heart rate and increase in peripheral resistance ( Wagner et al, 1991; Gasthuys et al., 1990 ). Alpha2 agonists relax the nasal alar and laryngeal muscles, predisposing horses to respiratory stridor and upper airway obstruction ( Muir, 1991 ). Alpha2 agonist decrease respiratory rate, resulting in slightly increased PaCO2 ( Wagner et al, 1991; Gasthuys et al.,
1990 ). During general anaesthesia, alpha2 agonists may cause additional hypoventilation and reduce PaO2 ( Steffey et al., 1985 ). Alpha2 agonists have also been shown to exert various effects on the gastrointestinal system in the horse. These effects may clinically useful in relieving spasm or ipermotility of large bowel ( Stick et al., 1987; Lester et al., 1998; Sutton et al., 2002 ) and the profound suppressive effect of a routine dose of detomidine or xylazine/butorphanol combination on equine duodenal motility must be considered when using these agents for management of colic, especially when encouragement of intestinal motility is desirable ( Merritt et al., 1998 ). Alpha2 agonists induce hyperglicemia and hypoinsulinemia in awake and anesthetized horses and are potent diuretic agent ( Thurmon et al., 1982; Tranquilli et al.,
38
1984; Gashuys et al., 1986; Gasthuys et al., 1988; Steffey et al., 2000; Watson et al., 2002 Nunez et al., 2002 ). The mechanisms of alpha2 agonist induced diuresis include an increase in glomerular filtration rate, inhibition of antidiuretic hormone release, and inhibition of anti-diuretic hormone response by renal tubules and increased release of atrial natriuretic factor ( Maze and
Tranquilli, 1991 ). Alpha2 agonist have also been shown to exert a marked increased in intrauterine pressure ( Schatzmann et al., 1994 ) than it may be prudent to avoid indiscriminate administration of alpha2 agonist to mares, especially during the later phases of pregnancy ( Daunt and Staffey, 2002 ).
Finally, the effects of alpha2 agonists can be pharmacologically antagonized with one of several antagonists. The availability of specific antagonists can be very useful when untoward effects are observed.
Local anaesthetic blocks are very effective in providing analgesia that prevents behavioural reactions associated with pain. In general, local anaesthetic blocks are easy to perform and can represent an important adjunct to other modes of pain relief. The mechanism of action of local anaesthetic involves blockade of sodium channels which prevents nerve depolarization. Use of local anaesthetics
(bupivacaine, lidocaine, mepivacaine) by perineural infiltration, intra-articular or epidural injection provides excellent analgesia ( Valverde and Gunkel, 2005 ).
Caudal epidural anaesthesia or analgesia, first described in 1925, is the most common epidural technique in horses ( Pape and Pitzschk, 1925; McLeod and
Frank, 1927 ). Several local anaesthetic drugs, such as lidocaine, bupivacaine,
39 and mepivacaine, are used to produce epidural anaesthesia, and epidural analgesia is obtained with opioid agonist, alpha2 adrenergic agonist, and ketamine ( Valverde et al., 1990; Gomez, 1998; Skarda and Tranquilli, 2007 ).
Depositions of local anaesthetic into the epidural space of the horse in the sacrococcygeal or intercoccygeal area is today a convenient approach to providing complete loss sensory and motor function (by depressing axonal conduction of nerves) to the tail and the perineum in standing horse, and avoid many of the hazards of general anaesthesia and recumbency ( Robinson and
Natalini, 2002 ). Intravenous administration of the sodium-channel blocker lidocaine is an effective treatment for post operative pain in man ( Cassuto et al.,
1985; Mao and Chen, 2000; Williams and Stark, 2003 ). There has been considerable interest in the use of systematically administered lidocaine as an anaesthetic-sparing and analgesic drug in horses ( Doherty and Frazier, 1998;
Brianceau et al., 2002; Malone and Graham, 2002; Dzikiti et al., 2003; Murrel et al., 2005; Ringer et al., 2007 ). Surgical procedure of tail, anus, rectum, vulva, vagina, urethra and bladder can be performed in the standing horse under caudal epidural injection of local anaesthetic ( Skarda, 1991 ). Additional drugs such alpha2 agonist have been added to increase the intensity, reliability and duration of local anaesthetics but ataxia and recumbency are possible complications
( Chopin and Wright, 1995; Wittern et al., 1998 ). Additional procedures such as surgical correction of prolapsed rectum, or correction of rectovaginal fistula, fetotomy, and correction of uterine torsion, laparoscopic cryptorchidectomy and
40 perineal urethrotomy are indications for local anaesthetics ( Green and Thurmon,
1985; Laverty et al., 1992; Skarda, 1996 ).
Ketamine has been used commonly as a part of the anaesthetic regimen for most species. More recently, it has gained popularity used at subanaesthetic doses to produce analgesia. The analgesia is because of antagonism of N-methyl-Daspartate (NMDA) receptors, inhibiting the excitatory actions of glutamate; this reduces sensitization and wind-up during pain ( Eide, 2000; Kronenberg, 2002 ).
Thus ketamine is more appropriate to prevent secondary hyperalgesia. Ketamine is effective in treating neuropathic and nociceptive pain at subanaesthetic doses and does not cause any of side effects that have been associated with doses that produce dissociative anaesthesia, such as tremors, tonic spasticity, or convulsive seizures ( Valverde and Gunkel, 2005 ). In the anaesthetized horse, ketamine administered as an infusion decreased inhalant anaesthetic requirement accompanied by an increased cardiac output ( Muir and Sams, 1992 ). Ketamine has been used alone for caudal epidurals in awake horses producing 30 to 90 minutes of analgesia, with mild sedation but non cariorespiratory changes
( Gomez et al., 1998 ). In combination with xilazina, mild sedation but no recumbency is produced, and there are significant decreased in heart rate and respiratory rate ( Kariman et al., 2000 ). In anaesthetized horses is a common practice to give a bolus of ketamine (0.1 mg/kg IV) if the horses developed nistagmus to deepen anaesthesia ( Ringer et al., 2007 )
TRAMADOL REVIEW
Chemical formula: C
16
H
25
NO
2
Chemical structure
41
Tramadol is a synthetic opioid analogue of codeine first synthesised in 1962 by
Grunenthal in an attempt to reduce common opioid adverse effects such as respiratory and cardiovascular depression ( Shipton, 2000 ) and has been used clinically for the last two decades to treat pain in humans ( Besson and Vickers,
1994; Eggers and Power, 1995; Kukanich and Papich, 2004 ), particularly for postoperative analgesia following orthopaedic surgery and major gynaecologic surgeries in addition to non-surgical condition ( Lehmann et al., 1990; Grond et al., 1995; Tuncer et al., 2003 ). Tramadol Hydrocloride (1RS, “RS)-
[(dismethylamin) methyl]-1-(3-methoxyphenyl) cyclohexanol HCl, produces its antinociceptive effect in animals and analgesic effect in humans by both opioid and non-opioid mechanism of action ( Hennies et al., 1988; Driessen and
Reimann, 1989; Reimann et al., 1990; Friderichs et al., 1991; Driessen and
42
Reimann, 1992; Friderichs et al., 1992; Kayser et al., 1992; Raffa et al., 1992;
Collart et al., 1993; Collart et al., 1993; Driessen et al., 1993; Raffa et al., 1993;
Sevcik et al., 1993; Desmeules et al., 1994; Desmeules et al., 1994; Reimann and Hennies, 1994; Desmeules et al., 1996; Oliva et al., 2002; Berrocoso et al.,
2006; Ide et al., 2006; Raffa, 2008 ). Tramadol is a centrally acting analgesic, which has a relatively low affinity for opiate receptors and also appears to modify the transmission of pain impulses by inhibition of norepinephrine
(noradrenaline, NA) and 5-hydroxytryptamine (serotonine, 5-HT) uptake in the descending inhibitory spinal monoaminergic pathways ( Raffa et al., 1992;
Desmeules et al., 1996; Bamigbade and Langford, 1998 ). Descending input from limbic and cortical structures involved in the cognitive appraisal of pain is integrated with ascending nociceptive transmission within the brainstem, which in turns, sends reciprocal 5-HT containing and NA containing projections to the spinal cord ( Millan, 2002 ). The balance between descending inhibitory and facilitatory monoaminergic inputs contributes to the maintenance of central sensitisation within nociceptive pathways ( Porreca et al., 2002; Suzuki et al.,
2004 ). That tramadol mediated its analgesic effect through inhibition of monoamine reuptake, an alpha2 adrenergic effect, in vivo was confirmed in animal and human studies, in which tramadol’s analgesic effects were blocked after yoimbine administration ( Raffa et al., 1992; Desmeules et al., 1996 ).
Tramadol has been studied for abuse potential in several animal species, for qualitative response in drug abusers and for actual abuse in epidemiological
43 studies ( Preston et al., 1991; Cicero et al., 2005; Adams et al., 2006; Epstein et al., 2006 ). Each of these approaches has led to the same conclusion, that tramadol has low, but not zero, abuse potential ( Raffa, 2008 ).
In general, tramadol has been found to be an opioid agonist with selectively for the μ receptor but with some weak affinity for the κ and δ receptors. The affinity for the μ receptor is approximately 10-fold less than codeine and 6000-fold less than morphine ( Raffa et al., 1995; Bamigbade and Langford, 1998; Scott and
Perry, 2000 ). Because it is a weak μ-opioid agonist, it produces significantly less respiratory depression ( Duthie, 1998 ).
The contribution of non-opioid activity is demonstrated by the analgesic effects of tramadol, in contrast to other opioids, not being fully antagonised by the μopioid receptor antagonist naloxone. In fact Tramadol-induced analgesia is only partially antagonized by the opiate antagonist naloxone in several animal tests
( Gillen et al., 2000 ).
Tramadol is marketed as a racemic mixture containing 50% of a R(+) tramadol and 50% of a S(-) tramadol. Studies of the effects of tramadol on various neurotransmitter systems have shown that the racemate and the two enatiomers of tramadol hydrochloride have varying effects ( Lee et al., 1993; Dayer et al.,
1997; Bamigbade and Langford, 1998; Scott and Perry, 2000 ). The (+)-tramadol enantiomer is a selective agonist of μ-opioid receptors and inhibits serotonin (5-
HT) reuptake. Whereas (-)-tramadol mainly inhibits noradrenaline (NA) reuptake, stimulating α2-adrenergic receptors but has little affinity for μ-opioid
44 receptors ( Shipton, 2000 ). The (+)-enantiomer was found to have 10-fold higher analgesic activity than the (-)-enantiomer. The complementary and synergistic actions of the two enantiomers improve the analgesic efficacy and tolerability profile of the racemate ( Grond and Sablotzki, 2004 ). In addition to the direct analgesic effect at the opioid receptor, the monoaminergic activity (in particular
α2-adrenergic stimulation) has a significant analgesic contribution by blocking nociceptive impulses at the spinal level ( Shipton, 2000; Scott and Perry, 2000 ).
Tramadol use may be limited by its potential to increase risk of seizures.
Tramadol increased the risk for seizure in patients taking serotonin reuptake inhibitors, tricyclic antidepressant, opioids and if combined with drugs that decrease seizure threshold, such as monoamine oxidase inhibitors. Furthermore, combination of tramadol with CNS depressant may produce respiratory depression ( Stephens et al., 2003; McCarberg, 2007 ). It is recommended that tramadol should not be used in patients with severe renal and liver impairments
( McCarberg, 2007 ).
Tramadol is metabolized by the cytochrome P450 2D6 (CYP2D6) enzyme system in the liver to form 11 metabolites, of which M1 (o-desmethyltramadol) predominates and possess analgesic properties ( Budd and Langford, 1999;
Subrahmanyam et al., 2001; Garcia-Quetglas et al., 2007 ). Therefore the analgesic effect of tramadol is thought to be due to the synergistic activity of the racemate with further contribution from the M1 metabolite. The affinity of the
M1 metabolite to the μ-opioid receptor is 20 to 40 times greater than that of
45 codeine and 160 to 300 times greater than that of the parent compound, while the affinity of morphine is 7 to 12 times greater ( Hennies et al., 1988; Grond et al., 1992; Dayer et al., 1994; Raffa et al., 1995; Frink et al., 1996 ). Furthermore,
M1 has an elimination half-life of nine hours, compared with six hours for tramadol itself. The analgesic effect of tramadol is less in patients who have low
CYP2D6 enzymatic activity. Phase II hepatic metabolism renders tramadol and its metabolites water-soluble and they are mainly excreted by the kidneys. The mean elimination half-life is about 6 hours ( Paar et al., 1997 ).
46
TRAMADOL: A NEW ANALGESIC DRUG
IN VETERINARY MEDICINE
The pharmacokinetics of tramadol have been investigated in several animal species, such as mice, rats ( Tao et al., 2002; Wu et al., 2001, Wu et al., 2006;
Zaho et al., 2008 ), rabbits ( Kucuk et al., 2005; Souza MJ, 2008 ), dogs ( Wu et al., 2001; Kukanich and Papich, 2004; Giorgi et al., 2008; McMillan et al., 2008,
Vettorato et al., 2009 ), cats ( Pypendop and Ilkiw, 2007 ), goats ( De Sousa et al.,
2007 ), camels ( Elghazali et al., 2007 ) and horses ( Giorgi et al., 2006; Shilo et al., 2007; De Leo et al., 2009 ). Pharmacokinetic and pharmacodynamic characterisation of tramadol is difficult because of differences between tramadol concentrations in plasma and at the site of action, and because of pharmacodynamic interactions between the two enantiomers of tramadol and its active metabolites ( Scott and Perry, 2000 ).
Some works have been carrying out to explain antinociceptive effects of tramadol in small animal. The most pertinent studies are briefly reviewed below.
In one of these Mastrocinque and Fantoni (2003) compared morphine (0.2 mg/kg IV) with tramadol (2.0 mg/kg IV) for the management of early postoperative pain following ovariohysterectomy after pyometra in dogs. They concluded that there were no significant differences between the analgesia provided morphine and tramadol suggesting that tramadol may be as effective as morphine for postoperative analgesia for ovariohysterectomy in dogs.
47
In another study, investigators ( Guedes et al., 2005 ) administered tramadol (1 mg/kg) epidurally at the lumbo-sacral space diluted in distilled water in dogs submitted to stifle surgery. They concluded that epidural tramadol produces satisfactory intra-operative antinociception and post-operative analgesia without causing clinically significant hemodynamic and respiratory depression in healthy dogs undergoing stifle surgery.
In the latest work, Kongara et al. (2009) compared the effects of morphine, parecoxib, tramadol and a combination of parecoxib, tramadol and pindolol on nociceptive thresholds in awake animals and their effect on glomerular filtration rate in eight adult dogs subjected to 30 minutes of anaesthesia. They concluded that tramadol and parecoxib (either alone or in combination) can increase nociceptive thresholds in awake dogs and have minimal effects on renal perfusion in normotensive dogs subjected to anaesthesia.
Steagall et al. (2008) compared the antinociceptive effects of subcutaneous tramadol (1.0 mg/kg), or acepromazine (0.1 mg/kg), or tramadol (1.0 mg/kg) with acepromazine (0.1 mg/kg) in cats. They reported that the acepromazinetramadol combination enhanced analgesia above that of either drug alone.
The respiratory depression by tramadol in the cat was investigated by Teppema et al. (2003). In this study the effects of tramadol and naloxone were considered by applying square-wave in end-tidal pressure of carbon dioxide and by analyzing the dynamic ventilatory responses. In the dose range of 1.0-4.0 mg/kg, tramadol caused a dose-dependent depressant effect on ventilatory control,
48 consisting of a decreased in carbon dioxide sensitivity of peripheral and central chemoreflex loops and increased in the apneic threshold. At dose of 0.1 mg/kg, naloxone completely reversed the depressant effect of tramadol on ventilatory control and it prevented more than 50% of the respiratory depression after a single dose of tramadol. The authors concluded that tramadol caused respiratory depression in anaesthetized cat, which is largely, if not completely, mediated by an action on opioid receptors.
Ko and co-workers (2008) in a crossover study compared the effect of oral administration of tramadol alone and with IV administration of butorphanol or hydromorphone on the minimum alveolar concentration (MAC) of sevoflurane in cats. They concluded that administration of tramadol, butorphanol, or hydromorphone reduced the MAC of sevoflurane in cats, compared with that in cats treated with saline solution. The reductions detected were likely mediated by effects of the drugs on opioid receptors. An additional reduction in MAC was not detected when tramadol was administered with butorphanol or hydromorphone.
Pypendop and Ilkiw (2007) investigated the pharmacokinetics of tramadol and the active metabolite M1 in cats after oral administration on 4.0 mg/kg of an immediate-release tablet. They concluded that tramadol concentration at this dose was maintained for fewer 6 hours, but concentration of M1 maintained for greater 12 hours.
49
TRAMADOL IN HORSE
The first study that evaluated the analgesic effects of tramadol in horses was carrying out by Natalini and Robinson (2000). In this study, the authors evaluated the analgesic effects of epidurally administered morphine, alfentanil, butorphanol, tramadol, and U50488H (a selective k agonist) diluted in physiologic saline in horses. The most potent pain-relieving substances known are opioid analgesics, but these drugs are not used extensively in horses, because substantial sympathetic stimulation and CNS excitation are observed when opioids, such as morphine, fentanyl, pentazocine, and butorphanol, are administered IV. The mechanisms for CNS excitation are unknown but may be related to cerebral catecholamine release (norepinephrine and dopamine) and opiate receptor activation ( Tobin and Miller, 1979; Combie et al., 1981 ).
Epidural opioid administration offers a potentially useful alternative to routes of administration that result in systemic distribution in horses. In this experimental study morphine (0.1 mg/kg), alfentanil (0.02 mg/kg), butorphanol (0.08 mg/kg), tramadol (1.0 mg/kg), U50488H (0.08 mg/kg) or sterile water were injected in the first intercoccygeal space in 5 awake standing horses held in stocks.
Avoidance of painful stimulus and analgesia were assessed by use of a constant current nerve stimulator that induced an electrical stimulation. Threshold levels
> 40 V were considered to represent complete analgesia, sufficient for skin incision. Neither ataxia nor recumbency was observed in horses after epidurally
50 injection. The onset time for tramadol was faster than that of morphine because of its higher tissue affinity, which would allow tramadol to cross the dura mater faster than morphine. After crossing the dura mater, lipid-soluble drugs tend to bind to the receptors in the spinal cord, whereas water-soluble drugs tend to remain in the cerebrospinal fluid. The dose of tramadol used in the study was similar to that used in humans ( Baraka et al., 1993 ). The authors concluded that in horses, caudal epidural administration of tramadol or morphine has potential in management of perineal and lumbosacral pain in horses. Regional differences exist in the intensity and duration of pain relief provided by these drugs.
Tramadol had a faster onset of action than morphine, but duration of effect was shorter. The less intense analgesic effect observed could be attributable to the ability of tramadol to inhibit amine neuronal uptake at the descending monoaminergic pathways involved in analgesia.
The same authors (2003) described the effects after epidural administration of morphine (0.1 mg/kg), butorphanol (0.08 mg/kg), alfentanil (0.02 mg/kg), tramadol (1 mg/kg), U50488H (0.08 mg/kg), or sterile water on heart rate, arterial blood pressure, respiratory rate, body temperature, and behaviour (head drooping, spontaneous locomotor activity) in five conscious adult horses restrained in stocks. Treatments were administered into first intercoccygeal epidural space with 18-gauge 3.0-inch epidural needle. It was concluded from the results of this study that caudal epidural administration of opioids and tramadol produces neither clinically relevant cardiovascular, respiratory, or
51 rectal temperature changes, nor locomotors impairment. Sedation and head ptosis are produced with morphine, U50488H, and tramadol. Duration of these effects was shortest (3 hours) with tramadol. Tramadol also produced a shorter duration of sedation because it produces activation of the monoaminergic pathways in the CNS, probably increasing the 5-HT levels and producing awareness.
About the pharmacokinetics of tramadol in horses there are two publications.
The fist one ( Giorgi et al., 2006 ) evaluated the cytochrome P450 metabolism in vitro and it concluded that M1 metabolite was not identified, in accordance with
Nebbia et al.(2003) that observed a wide interspecies variations in the activity of hepatic xenobiotics metabolizing enzyme, including the horse.
In the second study, Shilo and co-workers (2008) investigated the pharmacokinetics of tramadol and its metabolite M1 following oral (2.0 mg/kg
PO) immediate release, oral (2.0 mg/kg PO) slow release, intravenous (2.0 mg/kg IV) and intramuscular (2.0 mg/kg IM) administration in seven horses.
Adverse effects were observed during the IV administration in the first two horses, which were having muscle twitching, mainly of the pectoral muscles that lasted 10-15 min. This adverse effect was not observed when tramadol administration was prolonged (10 min). Twenty four hours after tramadol slow release administration, one of the horses was found in lateral recumbence and its gastrointestinal sounds were decreased. Blood electrolytes were normal and 15 min later the horse was again responsive. Two horses had a mildly elevated
52 blood creatinine values 36 hours after tramadol administration. These values become normal 4 weeks after. Decrease in blood pressure was not noted in any of horses following IV administration of tramadol. No other adverse effects were observed during the study. Very low mean plasma levels of tramadol and the metabolite M1 were detected following IV, IM and PO administration of tramadol at 2.0 mg/kg body weigh. Following IV administration, the elimination half-life of tramadolo was 82 min, significantly shorter than the 5.5 hours reported in humans ( Scott and Perry, 2000 ), and was similar to that reported in dogs ( Kukanich and Papich, 2004 ). Apparent volume of distribution in this study was similar to that reported previously in both humans ( Shipton, 2000 ) and dogs ( Kukanich and Papich, 2004 ). Tramadol was rapidly and completely absorbed after IM administration and adverse effects, including local reaction, were not observed, indicating that IM route of administration could be suggested in horses. Bioavailability in horses after PO administration was very low, which exclude this route of administration in horses. Food-drug interaction in horses, as was described for several drugs ( Bogan et al., 1984; Lees et al., 1988 ), might affect the bioavailability of tramadol. However, food intake withheld for 12 hours before drug administration to avoid food effects and still very low blood levels of tramadol were detected after PO administration. Results of this study suggest that tramadol can be administered to horse parenterally at dose of 2.0 mg/kg. However, tramadol cannot be administered orally as its bioavailability
53 was very low. Lack of detection of the active metabolite M1 suggests that tramadol might be less effective in horses.
54
SPERIMENTAL STUDY
MATERIALS AND METHODS
The study was conducted according to Good Clinical Practice Guideline and was approved by the Local Health Animal Institution of Camerino (ASL n.10).
Five clinically healthy, mature horses (one gelding and four mare), 12.2 ± 5.45 years of age and weighing 549 ± 50.9 kg, were used in the evaluation. Horses were randomly assigned to three treatment groups (Group 1: tramadol 1.0 mg/kg
IV; Group 2: tramadol 2.0 mg/kg IV; Group 3: sterile water IV) using randomized, double blind and crossover design. Horses were housed in a box stall during each of the different administrations. The agents were administered at intervals of at least 7 days, and each horse received each of three test materials. Investigator involved in collection of data were blinded to the identity of the agent being tested. Physical examination, complete blood and serum analysis (hematocrit exam, renal and hepatic functions) were performed 24 hours before the beginning of the study. Feed was withheld from all horses for
12 hours before drug administration and during this time free access to fresh water was provided. Two hours after drug administration, the horses were allowed access to feed.
Tramadol HCl (Tramadolo, Dorom® 100mg/2ml) was used for IV administration. Tramadol was administered intravenously after dilution in saline solution (to attain 40 ml in each syringe) at dose of 1.0 mg/kg and 2.0 mg/kg via
55 an indwelling 14-G catheter inserted in the jugular vein. Tramadol was administered slowly, over 10 minutes (4 ml/minute).
Measurements of response variables took place immediately before (baseline)
IV administration and 5, 10, 15, 30, 60, 90, 120, 240, 480, 600, 720 minutes after injection. Heart rate, respiratory rate, arterial blood pressure, body temperature, blood gas analysis, head ptosis and spontaneous locomotor activity were measured. Heart rate was measured by direct palpation of the mandibular vein or by auscultation. Respiratory rate was determined by counting thoracic and abdominal excursion over a 1 minute period. Arterial blood pressure
(systolic, diastolic, and mean) was measured using an indirect oscillometric blood pressure monitor (Poet Plus® 8100, Criticare Systems Inc.), with the cuff placed at the tail base. Blood pressure measurements were not corrected for the height of the tail above the heart. Rectal temperature (C°) was measured using an electronic thermometer. Arterial blood gases analyses (pH, PaCO
2
and PaO
2
) were monitored using an handheld analyser (I-STAST, Abbott). Head ptosis was assessed by measurements of the distance (cm) from the muzzle to the floor.
Spontaneous locomotors activity was evaluated for muscular coordination and action and score as 0 (no change from baseline), 1 (CNS excitation; hypersensitive to manipulation, increased locomotor activity; muscle twitching),
2 (motor ataxia; inability to control or coordinate movements of the muscles), or
3 (sensory ataxia and loss of proprioception).
56
At 120, 240, and 720 minutes a complete blood and serum biochemical analysis were performed.
The data sheet is showed below.
Time
Group
HR
RR
Temp
Head ptosis
Locom
Activ
Arter pH
PaCO
2
PaO
2
Sistol
Pr
Diastol
Pr
Mean
Pr
Blood
Seamp
T0 x
T5 T10 T15 T30 T60 T90 T120 T240 T480 T600 T720 x x x
STATISTICAL ANALYSIS
Numerical variables were analysed by use of repeated-measures analysis of variance (ANOVA), and categorical variables (spontaneous locomotor activity) were analysed by use of the non-parametric Friedman test. Values of P < 0.05 were considered significant. Data are expressed as mean ± standard deviation
(SD).
57
RESULTS
There were no significant changes in all parameters from baseline after administration of the two dosages of tramadol during the study period, except for spontaneous locomotor activity. In fact, adverse effects were observed at five minutes after IV administration of Tramadol 2mg/kg in all horses, which showed muscle twitching, mainly of the pectoral muscles that lasted 10 minutes.
No horse exhibited signs of CNS excitation at any time after treatments.
No significant changes in laboratory tests were observed during the study.
CONCLUSIONS
Opioids have been used in horse veterinary practice for at least seventy years but any usefulness is restricted because there appears to be a very narrow margin between analgesia and arousal or excitation. Indeed, the analgesic potency of opioids in horses is not readily and consistently quantifiable, and there are a number of other undesirable side effects of opioids that must be considered clinically. Substantial sympathetic stimulation and CNS excitation are observed when opioids are administered IV. Narcotics such as morphine, fentanyl, pentazocine, and butorphanol are potent locomotor stimulants in the horse when administered IV. The mechanism for CNS excitation are unknown but may be related to cerebral catecholamine release (especially norepinephrine and dopamine) and opiate receptor activation. Results of studies in horses indicate
58 that catecholamine inhibition and opiate receptor antagonist, like naloxone, block these CNS excitatory effects.
Tramadol hydrochloride is a centrally acting analgesic agent that is structurally related to morphine and codeine with opioid and non-opioid mechanism of action that causes activation of central pain inhibitory mechanism.
Approximately 30% of analgesic effect of tramadol can be reversed by administration of naloxone in humans. Tramadol differs from typical µ opioid agonists in that it does not cause adverse effects such as respiratory depression, constipation, or sedation.
Tramadol is being used in veterinary medicine, but data regarding its effects and tolerability are limited. By now, there are only two studies regarding tramadol epidurally administration and the authors concluded that tramadol produces neither clinically relevant cardiovascular, respiratory, or rectal body temperature changes, nor locomotor impairment and it has potential in management of perineal and lumbosacral pain in horse.
The aim of the present study was to evaluated the effects and tolerability of systemically administered tramadol.
Following IV administration at a dose of 1.0 mg/kg to five healthy horse, it was well tolerated without any adverse effects. Few side effects were observed in all the horses following the administration of tramadol at a dose of 2.0 mg/kg IV.
Muscle twitching was observed in spite of extending the time of tramadol IV administration (10 minutes). Similar adverse effect was not reported in humans,
59 but it is recommended that IV injections should be given slowly to minimize adverse effects such as transient hemodynamic instability.
At 120, 240, and 720 minutes a complete blood and serum biochemical analysis were performed. Differently from Shilo (2007), high blood creatinine levels were not observed in any horses.
Results of this study suggest that tramadol is well tolerated and can be IV administered to horses at dose of 2.0 mg/kg with caution of slowly injection.
Further studies are required to establish its real potential in management of pain relief regarding the lack of detection of the active metabolite M1. Tramadol could be an important analgesic drug in the management of pain in the horse especially in combination with other sedative agents.
60
STATISTICAL ANALYSIS
Graphic 1. Heart rate collected data: no significant differences were observed.
45
40
95% CI
35
HRT0
HRT5
HRT10
HRT15
HRT30
HRT60
HRT90
HRT120
HRT240
HRT480
HRT600
HRT720
30
25
F T1
Group
T2
HRT0
HRT5
HRT10
HRT15
HRT30
HRT60
HRT90
HRT120
HRT240
HRT480
HRT600
HRT720
Descriptive Statistics
32,60
34,00
33,67
34,80
31,20
34,00
33,33
37,20
34,40
34,40
34,80
34,40
33,60
34,00
34,00
34,40
Mean
33,00
35,60
36,20
34,93
32,80
34,40
36,40
34,53
33,20
35,20
36,40
34,93
35,60
32,00
37,20
33,60
36,00
34,80
33,60
34,80
34,80
31,80
33,60
34,20
36,80
36,80
33,20
35,60
31,60
35,40
32,80
34,33
Std. Deviation
3,317
4,775
2,864
3,751
3,633
3,847
4,561
4,033
4,817
3,347
5,727
4,590
5,727
2,793
6,325
5,473
5,933
1,095
5,657
4,701
5,933
1,673
5,550
4,395
4,775
1,673
2,828
3,117
7,403
2,449
5,215
4,290
3,742
5,215
1,673
3,688
5,586
2,490
3,286
4,507
3,347
5,215
2,683
4,014
2,608
3,578
3,633
4,203
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
Total
F
T1
T2
Total
F
T1
T2
Total
Total
F
T1
T2
Total
F
T1
T2
N
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
5
15
5
5
5
5
15
5
5
5
15
5
5
15
5
5
5
5
5
15
15
5
5
5
15
5
5
5
61
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
72,994
72,994
72,994
72,994
372,489
372,489
372,489
372,489
1788,267
1788,267
1788,267
1788,267
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Type III Sum of Squares
Intercept 212936,006
Group 15,511
Error 883,733 df
Mean
Square F
1 212936,006 2891,406
2 7,756 ,105
12 73,644 df
11
6,103
11,000
1,000
22
12,206
22,000
2,000
132
73,239
132,000
12,000
Mean Square
6,636
11,960
6,636
72,994
16,931
30,516
16,931
186,244
13,547
24,417
13,547
149,022
Sig.
,000
,901
62
F
,490
,490
,490
,490
1,250
1,250
1,250
1,250
Sig.
,907
,817
,907
,497
,218
,266
,218
,321
63
Graphic 2. Respiratory rate collected data: no significant differences were observed.
40
30
RRT0
RRT5
RRT10
RRT15
RRT30
RRT60
RRT90
RRT120
RRT240
RRT480
RRT600
RRT720
20
10
0
F T1
Group
T2
RRT0
RRT5
RRT10
RRT15
RRT30
RRT60
RRT90
RRT120
RRT240
RRT480
RRT600
RRT720
Descriptive Statistics
15,60
20,40
17,73
16,40
14,40
17,20
16,00
16,40
15,60
20,40
17,47
13,60
11,20
19,40
14,73
17,20
Mean
15,20
14,80
18,00
16,00
17,20
17,20
21,60
18,67
16,40
16,00
22,40
18,27
16,40
13,60
16,00
13,87
16,00
14,40
12,80
14,40
13,60
14,80
16,80
16,00
16,00
13,80
15,20
15,00
12,00
14,80
17,20
15,20
Std. Deviation
3,347
4,604
10,198
6,414
4,817
6,261
9,940
7,118
6,542
4,000
14,450
9,254
5,550
2,191
11,082
7,166
5,367
1,673
10,640
6,547
5,727
3,286
11,171
7,230
2,966
1,095
9,581
6,464
6,099
3,847
3,162
3,662
6,481
1,673
3,033
4,154
3,286
2,683
8,786
5,855
5,477
3,033
4,147
4,123
3,464
4,147
10,257
6,361
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
Total
F
T1
T2
Total
F
T1
T2
Total
Total
F
T1
T2
Total
F
T1
T2
N
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
5
15
5
5
5
5
15
5
5
5
15
5
5
15
5
5
5
5
5
15
15
5
5
5
15
5
5
5
64
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
414,178
414,178
414,178
414,178
287,522
287,522
287,522
287,522
1707,467
1707,467
1707,467
1707,467
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Type III Sum of Squares
Intercept 46722,222
Group 383,678
Error 4454,933 df
1
2
12
Mean
Square
191,839
371,244
F
46722,222 125,853
,517 df
11
2,951
4,670
1,000
22
5,902
9,341
2,000
132
35,410
56,043
12,000
Mean Square
37,653
140,361
88,684
414,178
13,069
48,719
30,782
143,761
12,935
48,220
30,467
142,289
Sig.
,000
,609
65
F
2,911
2,911
2,911
2,911
1,010
1,010
1,010
1,010
Sig.
,002
,049
,023
,114
,456
,434
,444
,393
66
Graphic 3. Temperature collected data: no significant differences were observed.
38,0
37,5
TempT0
TempT5
TempT10
TempT15
TempT30
TempT60
TempT90
TempT120
TempT240
TempT480
TempT600
TempT720
37,0
36,5
F T1
Group
T2
TempT0
TempT5
TempT10
TempT15
TempT30
TempT60
TempT90
TempT120
TempT240
TempT480
TempT600
TempT720
Descriptive Statistics
37,260
37,440
37,427
37,300
37,340
37,320
37,320
37,300
37,280
37,260
37,247
37,340
37,200
37,240
37,260
37,580
Mean
37,360
37,440
37,380
37,393
37,38
37,22
37,38
37,33
37,320
37,060
37,260
37,213
37,200
37,32
37,34
37,31
37,620
37,520
37,300
37,480
37,460
37,460
37,200
37,320
37,320
37,460
37,080
37,287
37,28
37,620
37,320
37,467
Std. Deviation
,3647
,1517
,5167
,3494
,482
,438
,482
,440
,4550
,5857
,3130
,4454
,4416
,3362
,2510
,2789
,6964
,1517
,4817
,4601
,4472
,4087
,3847
,3833
,3435
,3674
,3782
,3418
,1789
,311
,462
,402
,3347
,3114
,4123
,3570
,5367
,3286
,2236
,3385
,3271
,2702
,4764
,3777
,502
,2950
,4438
,4237
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
Total
F
T1
T2
Total
F
T1
T2
Total
Total
F
T1
T2
Total
F
T1
T2
N
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
5
15
5
5
5
5
15
5
5
5
15
5
5
15
5
5
5
5
5
15
15
5
5
5
15
5
5
5
67
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
1,224
1,224
1,224
1,224
1,469
1,469
1,469
1,469
13,007
13,007
13,007
13,007 df
11
3,990
7,222
1,000
22
7,980
14,444
2,000
132
47,878
86,662
12,000
Mean Square
,111
,307
,170
1,224
,067
,184
,102
,734
,099
,272
,150
1,084
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Intercept
Group
Error
Type III Sum of Squares
250939,737
,194
10,429 df
1
2
12
Mean Square
250939,737 288740,7
,097
,869
F
,112
Sig.
,000
,895
F
1,130
1,130
1,130
1,130
,677
,677
,677
,677
68
Sig.
,343
,354
,352
,309
,855
,708
,795
,526
69
Graphic 4. Head ptosis collected data: no significant differences were observed.
150
140
130
Head ptosisT0
Head ptosisT5
Head ptosisT10
Head ptosisT15
Head ptosisT30
Head ptosisT60
Head ptosisT90
Head ptosisT120
Head ptosisT240
Head ptosisT480
Head ptosisT600
Head ptosisT720
120
90
110
100
F T1
Group
T2
Head ptosisT0
Head ptosisT5
Head ptosisT10
Head ptosisT15
Head ptosisT30
Head ptosisT60
Head ptosisT90
Head ptosisT120
Head ptosisT240
Head ptosisT480
Head ptosisT600
Head ptosisT720
Descriptive Statistics
118,60
115,40
118,40
121,40
113,20
121,40
118,67
119,80
125,00
116,20
119,00
113,60
116,80
122,00
117,47
121,20
Mean
119,80
112,80
122,00
118,20
111,60
119,00
121,60
117,40
120,00
121,20
118,60
119,93
115,80
114,00
118,80
115,67
110,60
117,00
113,20
113,60
118,40
116,20
117,00
117,67
120,20
112,20
114,20
115,53
114,20
114,00
112,00
114,80
Std. Deviation
8,497
10,085
4,899
8,546
7,701
16,140
7,503
11,255
4,690
9,203
9,711
7,658
7,497
16,757
5,505
9,826
3,050
8,228
2,608
6,321
5,495
5,745
13,572
9,871
8,325
19,422
7,649
12,535
2,387
11,576
6,648
10,314
10,114
6,083
7,259
7,890
5,595
4,817
3,674
4,655
6,870
11,389
6,419
8,643
13,255
3,808
5,385
5,388
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
Total
F
T1
T2
Total
F
T1
T2
Total
Total
F
T1
T2
Total
F
T1
T2
N
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
5
15
5
5
5
5
15
5
5
5
15
5
5
15
5
5
5
5
5
15
15
5
5
5
15
5
5
5
70
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Type III Sum of Squares
Intercept 2472216,80
6
Group 32,078
Error 3598,867 df
Mean
Square
1 2472216,806 8243,318
2
12
16,039
299,906
F
,053
Tests of Within-Subjects Effects
Sig.
,000
,948
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
592,194
592,194
592,194
592,194
1737,122
1737,122
1737,122
1737,122
7839,933
7839,933
7839,933
7839,933 df
11
3,721
6,501
1,000
22
7,442
13,002
2,000
132
44,655
78,009
12,000
Mean Square
53,836
159,139
91,096
592,194
78,960
233,407
133,609
868,561
59,393
175,568
100,500
653,328
71
F
,906
,906
,906
,906
1,329
1,329
1,329
1,329
Sig.
,536
,463
,501
,360
,164
,257
,214
,301
72
Graphic 5. Arterial pH collected data: no significant differences were observed.
7,55
Arterial pHT5
Arterial pHT15
Arterial pHT60
Arterial pHT120
Arterial pHT480
Arterial pHT720
7,50
7,45
7,40
7,35
F T1
Group
T2
73
Arterial pHT5
Arterial pHT15
Arterial pHT60
Arterial pHT120
Arterial pHT480
Arterial pHT720
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
T2
Total
F
T1
T2
Total
F
T1
T2
Total
Descriptive Statistics
Mean
7,4440
7,4420
7,4520
7,4460
7,450
7,444
7,450
7,448
7,4400
7,4360
7,4360
7,4373
7,4420
7,4240
7,4360
7,4340
7,4200
7,4100
7,4200
7,4167
7,4200
7,4140
7,4160
7,4167
Std. Deviation
,03647
,02950
,03701
,03225
,0412
,0351
,0552
,0414
,05148
,04159
,06269
,04877
,04764
,03362
,05595
,04388
,02550
,04243
,03317
,03222
,03317
,03782
,02702
,03063
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
,014
,014
,014
,014
,001
,001
,001
,001
,038
,038
,038
,038 df
5
2,853
4,459
1,000
10
5,706
8,919
2,000
60
34,233
53,513
12,000
Mean Square
,003
,005
,003
,014
6,78E-005
,000
7,60E-005
,000
,001
,001
,001
,003
N
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
F
4,478
4,478
4,478
4,478
,107
,107
,107
,107
Sig.
,002
,010
,002
,056
1,000
,994
,999
,900
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Intercept
Group
Error
Type III Sum of Squares
4972,603
,001
,087 df
1
2
12
Mean
Square
4972,603
,001
,007
F
688090,7
76
,072
Sig.
,000
,931
Graphic 6. PaCO
2 collected data: no significant differences were observed.
50
PaCO2T5
PaCO2T15
PaCO2T60
PaCO2T120
PaCO2T480
PaCO2T720
74
45
40
35
F T1
Group
T2
75
PaCO2T5
PaCO2T15
PaCO2T60
PaCO2T120
PaCO2T480
PaCO2T720
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
T2
Total
F
T1
T2
Total
F
T1
T2
Total
Descriptive Statistics
Mean
40,920
41,880
41,900
41,567
40,800
43,000
41,460
41,753
42,06
44,32
43,04
43,14
40,82
43,34
42,58
42,25
41,02
43,36
40,98
41,79
42,28
44,42
41,44
42,71
Std. Deviation
3,8454
3,2691
2,2814
2,9983
4,9985
3,6695
3,8220
4,0087
5,130
4,115
5,706
4,751
3,366
5,733
4,458
4,416
5,209
6,215
4,558
5,104
4,908
6,187
4,205
4,956
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
28,811
28,811
28,811
28,811
19,261
19,261
19,261
19,261
522,126
522,126
522,126
522,126 df
5
2,980
4,733
1,000
10
5,959
9,466
2,000
60
35,756
56,797
12,000
Mean Square
5,762
9,669
6,087
28,811
1,926
3,232
2,035
9,631
8,702
14,603
9,193
43,511
N
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
F
,662
,662
,662
,662
,221
,221
,221
,221
Sig.
,654
,580
,646
,432
,993
,967
,992
,805
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Type III Sum of Squares
Intercept 160284,040
Group 68,354
Error 1038,678 df
Mean
Square F
1 160284,040 1851,785
2
12
34,177
86,557
,395
Sig.
,000
,682
Graphic 7. PaO
2 collected data: no significant differences were observed.
140
PaO2T5
PaO2T15
PaO2T60
PaO2T120
PaO2T480
PaO2T720
120
76
100
80
60
F T1
Group
T2
77
PaO2T5
PaO2T15
PaO2T60
PaO2T120
PaO2T480
PaO2T720
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
T2
Total
F
T1
T2
Total
F
T1
T2
Total
Descriptive Statistics
Mean
98,20
84,60
87,00
89,93
92,60
83,00
85,40
87,00
88,40
83,80
87,72
86,64
91,20
87,30
88,20
88,90
93,00
90,60
98,80
94,13
91,60
92,00
96,14
93,25
Std. Deviation
13,627
11,104
12,649
13,101
11,327
12,708
8,355
10,981
3,362
7,981
10,139
7,430
4,025
5,119
12,872
7,902
8,031
5,459
18,913
11,910
4,159
7,314
6,633
6,108
N
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
736,886
736,886
736,886
736,886
633,089
633,089
633,089
633,089
3531,935
3531,935
3531,935
3531,935 df
5
2,959
4,688
1,000
10
5,918
9,377
2,000
60
35,509
56,260
12,000
Mean Square
147,377
249,024
157,175
736,886
63,309
106,973
67,518
316,545
58,866
99,465
62,779
294,328
F
2,504
2,504
2,504
2,504
1,075
1,075
1,075
1,075
Sig.
,040
,076
,044
,140
,395
,395
,395
,372
78
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Type III Sum of Squares
Intercept 728604,054
Group 487,711
Error 3593,225 df
Mean
Square F
1 728604,054 2433,259
2
12
243,855
299,435
,814
Sig.
,000
,466
Graphic 8. Systolic pressure collected data: no significant differences were observed.
180
160
140
Systolic prT0
Systolic prT5
Systolic prT10
Systolic prT15
Systolic prT30
Systolic prT60
Systolic prT90
Systolic prT120
Systolic prT240
Systolic prT480
Systolic prT600
Systolic prT720
120
100
80
F T1
Group
T2
Systolic prT0
Systolic prT5
Systolic prT10
Systolic prT15
Systolic prT30
Systolic prT60
Systolic prT90
Systolic prT120
Systolic prT240
Systolic prT480
Systolic prT600
Systolic prT720
Descriptive Statistics
124,20
125,40
122,53
119,40
121,60
125,80
122,27
122,20
128,20
125,00
125,33
129,60
137,20
136,00
134,27
118,00
Mean
129,80
130,00
135,80
131,87
123,80
126,20
136,80
128,93
138,00
121,80
138,40
132,73
122,80
115,20
130,80
120,67
125,20
130,40
111,40
122,33
121,40
114,20
127,20
121,20
124,20
116,40
119,40
120,00
116,00
124,60
118,00
121,33
Std. Deviation
26,546
14,916
11,300
17,598
9,706
21,856
26,781
20,062
23,377
31,483
32,145
28,260
23,499
10,918
28,780
17,594
26,207
5,595
13,646
16,307
19,779
21,959
35,164
25,575
19,731
22,731
21,389
20,037
9,823
10,918
16,423
13,906
7,050
8,532
21,338
15,296
7,701
21,891
6,834
17,110
8,672
15,241
11,261
11,625
9,747
4,037
12,590
8,641
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
Total
F
T1
T2
Total
F
T1
T2
Total
Total
F
T1
T2
Total
F
T1
T2
N
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
5
15
5
5
5
5
15
5
5
5
15
5
5
15
5
5
5
5
5
15
15
5
5
5
15
5
5
5
79
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
4496,044
4496,044
4496,044
4496,044
3985,289
3985,289
3985,289
3985,289
33906,333
33906,333
33906,333
33906,333
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average df
Mean
Square Source
Type III Sum of Squares
Intercept 2825515,02
2
Group 440,044
Error 18673,267
1 2825515,022
2
12
220,022
1556,106
F
1815,761
,141 df
11
4,350
8,268
1,000
22
8,700
16,537
2,000
132
52,202
99,221
12,000
Mean Square
408,731
1033,540
543,763
4496,044
181,149
458,065
240,995
1992,644
256,866
649,526
341,726
2825,528
Sig.
,000
,870
80
F
1,591
1,591
1,591
1,591
,705
,705
,705
,705
Sig.
,108
,186
,135
,231
,828
,697
,787
,513
81
Graphic 9. Mean pressure collected data: no significant differences were observed.
120
100
Mean prT0
Mean prT5
Mean prT10
Mean prT15
Mean prT60
Mean prT90
Mean prT120
Mean prT240
Mean prT480
Mean prT600
Mean prT720
80
60
F T1
Group
T2
Mean prT0
Mean prT5
Mean prT10
Mean prT15
Mean prT30
Mean prT60
Mean prT90
Mean prT120
Mean prT240
Mean prT480
Mean prT600
Mean prT720
Descriptive Statistics
87,60
91,40
85,80
83,20
80,60
85,60
83,13
85,60
86,40
90,80
88,40
95,60
110,20
92,80
99,53
78,40
Mean
87,40
89,80
98,00
91,73
92,80
83,80
102,20
92,93
89,00
88,80
83,60
87,13
88,00
82,80
84,60
82,67
87,20
91,40
78,00
85,53
89,20
72,20
89,60
82,47
81,60
74,40
81,60
79,20
80,60
83,00
77,20
83,13
Std. Deviation
16,652
16,829
9,110
14,350
13,918
19,980
18,295
18,041
8,276
17,782
23,681
16,638
14,612
23,028
17,184
17,288
17,138
8,019
18,968
14,476
12,502
15,915
12,498
13,474
18,420
33,124
18,620
23,913
10,431
3,033
16,607
9,788
10,085
14,993
10,271
12,529
10,330
10,183
21,373
16,252
18,849
12,973
12,857
14,463
6,348
19,455
8,408
13,585
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
Total
F
T1
T2
Total
F
T1
T2
Total
Total
F
T1
T2
Total
F
T1
T2
N
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
5
15
5
5
5
5
15
5
5
5
15
5
5
15
5
5
5
5
5
15
15
5
5
5
15
5
5
5
82
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
5248,194
5248,194
5248,194
5248,194
4424,489
4424,489
4424,489
4424,489
22632,400
22632,400
22632,400
22632,400
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average df
Mean
Square Source
Type III Sum of Squares
Intercept 1356336,80
6
Group 129,911
Error 14543,200
1 1356336,806
2
12
64,956
1211,933
F
1119,151
,054 df
11
5,475
11,000
1,000
22
10,950
22,000
2,000
132
65,700
132,000
12,000
Mean Square
477,109
958,569
477,109
5248,194
201,113
404,061
201,113
2212,244
171,458
344,479
171,458
1886,033
Sig.
,000
,948
83
F
2,783
2,783
2,783
2,783
1,173
1,173
1,173
1,173
Sig.
,003
,021
,003
,121
,283
,323
,283
,343
84
Graphic 10. Diastolic pressure collected data: no significant differences were observed.
140
120
100
Diastolic prT0
Diastolic prT5
Diastolic prT10
Diastolic prT15
Diastolic prT30
Diastolic prT60
Diastolic prT90
Diastolic prT120
Diastolic prT240
Diastolic prT480
Diastolic prT600
Diastolic prT720
80
60
40
20
F T1
Group
T2
Diastolic prT0
Diastolic prT5
Diastolic prT10
Diastolic prT15
Diastolic prT30
Diastolic prT60
Diastolic prT90
Diastolic prT120
Diastolic prT240
Diastolic prT480
Diastolic prT600
Diastolic prT720
Descriptive Statistics
70,80
71,80
67,67
63,60
67,40
62,00
64,33
59,60
71,00
71,20
69,87
72,20
91,60
71,40
78,40
60,40
Mean
64,60
69,80
76,60
70,33
69,20
67,40
76,60
71,07
66,20
64,00
66,40
65,53
67,40
64,80
62,00
64,07
74,00
77,60
58,40
70,00
70,80
62,60
65,80
62,67
66,20
59,00
67,20
64,13
65,40
65,40
59,40
65,20
Std. Deviation
20,599
18,472
18,407
18,476
20,729
24,193
17,573
19,880
14,167
18,330
21,984
17,108
18,078
29,312
20,897
20,938
12,602
11,305
19,000
13,803
8,620
18,987
17,513
16,949
8,044
30,664
15,339
21,162
11,781
5,357
14,832
10,117
13,820
14,893
13,759
15,698
13,864
11,760
27,031
16,625
15,090
9,138
15,959
13,266
10,065
15,805
9,290
13,197
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
T2
T2
Total
F
T1
T2
Total
F
T1
Group
F
T1
T2
Total
F
T1
Total
F
T1
T2
Total
F
T1
T2
Total
Total
F
T1
T2
Total
F
T1
T2
N
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
15
5
5
5
5
15
5
5
5
5
15
5
5
5
15
5
5
5
5
15
15
5
5
5
15
5
5
5
15
5
5
5
85
86
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
3243,261
3243,261
3243,261
3243,261
3920,056
3920,056
3920,056
3920,056
23968,767
23968,767
23968,767
23968,767
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Type III Sum of Squares
Intercept 826753,339
Group 223,144
Error 19048,433 df
Mean
Square F
1 826753,339 520,832
2 111,572 ,070
12 1587,369 df
11
5,964
11,000
1,000
22
11,927
22,000
2,000
132
71,564
132,000
12,000
Mean Square
294,842
543,835
294,842
3243,261
178,184
328,660
178,184
1960,028
181,582
334,926
181,582
1997,397
Sig.
,000
,933
F
1,624
1,624
1,624
1,624
,981
,981
,981
,981
Sig.
,099
,153
,099
,227
,492
,475
,492
,403
87
Graphic 11. Hematocrit collected data: no significant differences were observed.
45
HCTT0
HCTT120
HCTT240
HCTT720
40
35
30
25
HCTT0
HCTT120
HCTT240
HCTT720
F
Total
F
T1
T2
Total
F
T1
T2
Total
Group
F
T1
T2
Total
F
T1
T2
T1
Group
Descriptive Statistics
Mean
34,56
34,80
34,90
34,75
32,320
35,500
34,300
34,040
34,700
35,180
36,060
35,313
34,06
34,48
35,74
34,76
Std. Deviation
2,688
1,924
1,884
2,039
1,5336
4,0447
2,8583
3,0859
1,9481
3,4896
3,6212
2,9411
2,308
3,619
1,986
2,634
T2
N
15
5
5
5
15
15
5
5
5
15
5
5
5
5
5
5
Tests of Within-Subjects Effects
Measure: MEASURE_1
Source time time * Group
Error(time)
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Sphericity Assumed
Greenhous e-Geisser
Huynh-Feldt
Lower-bound
Type III Sum of Squares
12,257
12,257
12,257
12,257
18,297
18,297
18,297
18,297
86,766
86,766
86,766
86,766
Tests of Between-Subjects Effects
Measure: MEASURE_1
Transformed Variable: Average
Source
Type III Sum of Squares
Intercept 72314,817
Group 20,197
Error 284,466 df
1
2
12
Mean
Square F
72314,817 3050,550
10,099 ,426
23,706 df
3
2,067
2,920
1,000
6
4,134
5,840
2,000
36
24,802
35,037
12,000
Mean Square
4,086
5,930
4,198
12,257
3,050
4,426
3,133
9,149
2,410
3,498
2,476
7,231
Sig.
,000
,663
88
F
1,695
1,695
1,695
1,695
1,265
1,265
1,265
1,265
Sig.
,185
,204
,187
,217
,298
,310
,299
,317
89
Non Parametric Test. Spontaneous locomotor activity collected data: significant differences were observed ( P < 0.05).
SplocF
SplocT1
SpolocT2
N
60
60
60
Descriptive Statistics
Mean
,00
,02
,23
Std. Deviation Minimum Maximum
,000
,129
,427
0
0
0
0
1
1
Friedman Test
Ranks
SplocF
SplocT1
SpolocT2
Mean Rank
1,88
1,90
2,23
Test Statistics a
N
Chi-Square df
As ymp. Sig.
60
26,143
2
,000 a. Friedman Test
90
REFERENCES
Adams EH, Breiner S, Cicero TJ, Geller A, Inciardi JA, Schnoll SH, Senay
EC, Woody GE (2006): A comparison of the abuse liability of tramadol,
NSAIDs, and hydrocodone in patients with chronic pain. J Pain Symptom
Manage, 31, pp 465-76.
Anis NA, Berry SC, Burton NR, Lodge D (1983): The dissociative anaesthetics, ketamine and phencyclidine, selectively reduce excitation of central mammalian neurones by N-methyl-aspartate. Br J Pharmacol, 79, pp
565-575.
Bamigbade TA and Langford RM (1998): The clinical use of tramadol hydrochloride. Pain Rev, 5, pp 155-183.
Baraka A, Jabbour S Ghabash M, Nader A, Khoury G, Sibai A (1993): A comparison of epidural tramadol and epidural morphine for postoperative analgesia. Can J Anaesth, 40, pp 308-313.
Basbaum EI and Fields HL (1984): Endogenous pain control systems: brainstem spinal pathways and endorphin circuitry. Annu Rev Neurosci, 7, pp
309-338.
Bennet RC and Steffey EP (2002): Use of opioids for pain and anesthetic management in horses. Vet Clin North Am Equine Pract, 18, pp 47-60.
Benson GJ, Thurmon JC, Neff-Davis CA (1984): Effect of xylazine hydrochloride upon plasma glucose and serum insulin concentrations in adult pointer dogs. J Am Anim Hosp Assoc, 20, pp 791-794.
91
Berrocoso E, Rojas-Corrales MO, Mico JA (2006): Differential role of 5-
HT
1A
and 5-HT
1B
receptors on the antinociceptive and antidepressant effect of tramadol in mice. Psychopharmacol, 188, pp 111-118.
Besson JM (1988): What the brain tells to the spinal cord?
Electrophysiological and behavioural approaches. Acta Anaesthesiol Belg, 39, pp 87-90.
Besson JM and Vickers MD (1994): Tramadol analgesia. Synergy in research and therapy.
Drugs, 47, Suppl 1, pp 1-2.
Bettschart-Wolfensberger R, Clarke KW, Vainio O, Aliabadi F, Demuth D
(1999): Pharmacokinetics of medetomidine in ponies and elaboration of a medetomidine infusion regime which provides a constant level of sedation.
Res Vet Sci, 67, pp 41-46.
Bettschart-Wolfensberger R, Bowen MI, Freeman SL, Feller SL, Bettschart
RW, Nolan A, Clarke KW (2001): Cardiopulmonary effects of prolonged anesthesia via propofol-medetomidine infusion in ponies. Am J Vet Res, 62, pp 1428-1435. feeding on the fate of orally administered phenylbutazone, trimethoprim and sulphadiazine in the horse. Vet Rec, 115, pp 599-600.
Bogan JA, Galbraith A, Baxter P, Ali NM, Marriner SE (1984): Effect of
Bolser DC (1996): Mechanisms of action of central and peripheral antitussive drugs. Pulm Pharmacol, 9, pp 357-364.
92
Brianceau P, Chevalier H, Karas A, Court MH, Bassage L, Kirker-Head C,
Provost P, Paradis MR (2002): Intravenous lidocaine and small-intestinal size, abdominal fluid, and outcome after colic surgery in horses.
J Vet Inter Med,
16, pp 736-741.
Budd K and Langford R (1999): Tramadol revisited. Br J Anaesth, 82, pp
493-495.
Butterworth JF and Strichartz GR (1990): Molecular mechanisms of local anesthesia: a review. Anesthesiology, 72, pp 711-734.
Cagnardi P, Zonca A, Carli S, Fonda D, Ravasio G, Villa R (2006):
Pharmacokinetics of tramadol in cats undergoing neutering. J Vet Pharmacol
Therap, 29, pp 239-301.
Cassuto J, Wallin G, Hogstrom S, Faxen A, Rimback G (1985): Inhibition of postoperative pain by continuous low-dose intravenous infusion of lidocaine. Anesth Analg, 64, pp 971-974.
Chapman V and Dickenson DH (1993): The effect of intrathecal administration of RP67580, a potent neurokinin 1 antagonist on nociceptive transmission in the rat spinal cord. Neurosci Lett, 23, pp 149-152.
Chopin JB and Wright JD (1995): Complication after the use of a combination of lignocaine and xylazine for epidural anaesthesia in a mare.
Aust Vet J, 72, pp 354-355.
Cicero TJ, Inciardi JA, Adams EH, Geller A, Senay EC, Woody GE,
Munoz A (2005): Rates of abuse of tramadol remain unchanged with the
93 introduction of new branded and generic products: results of an abuse monitoring system, 1994-2004. Pharmacoepidemiol Drug Saf, 14, 851-859.
Coderre TJ, Vaccarino AL, Melzack R (1990): central nervous system plasticity in the tonic pain response to subcutaneous formalin injection. Brain
Res, 3, pp 155-158.
Coderre TJ, Kats J, Vaccarino AL, Melzack R (1993): Contribution of central neuroplasticity to pathological pain: review of clinical and experimental evidence. Pain, 52, pp 259-285.
Cohen ND, Mealey RH, Chaffin MK, Carter GK (1995): The recognition and medical management of right dorsal colitis in horses. Veterinary Medicine
90, pp 687–692.
Collart L, Luthy C, Dayer P (1993): Multimodal analgesic effect of tramadol. Clin Pharmacol and Therap, 53, p 223.
Collart L, Luthy C, Dayer P (1993): Partial inhibition of tramadol antinociceptive effect by naloxone in man. Br J Clin Pharmacol, 35, p 75.
Pharmacology of narcotic analgesics in the horse: selective blockade of narcotic-induced locomotor activity. Am J Vet Res, 42, pp 716-721.
Combie J, Shults T, Nugent EC, Dougherty J, Tobin T (1981):
Crile GW (1913): The kinetic theory of shock and its prevention through anoci-association. Lancet, 185, pp 7-16.
94
Crile GW and Lower WE (1914): Anoci-Association. Ed Saunders,
Philadelphia, pp 223-225.
Daunt DA and Steffey EP (2002): Alpha-2 adrenergic agonists as analgesics in horses.
Vet Clin North Am Equine Pract, 18, pp 39-46.
Daunt DA and Steffey EP (2002): Alpha-2 adrenergic agonists as analgesics in horses. Vet Clin North Am Equine Pract, 18, pp 39-46.
Davies JV and Gerring EL (1983): Effect of spasmolytic analgesic drugs on the motility patterns of the equine small intestine. Res Vet Sci, 34, pp 334-339.
Dayer P, Collart L, Desmeules J (1994): Pharmacology of tramadol. Drugs,
47, pp 3-7.
Dayer P, Desmeules J, Collart L (1997): Pharmacology of tramadol. Drugs,
53, pp 18-24.
De Leo M, Giorgi M, Saccomani G, Manera C, Branca A (2009):
Evaluation of tramadol and its main metabolites in horse plasma by highperformance liquid chromatography/fluorescence and liquid chromatography/electrospray ionization tandem mass spectrometry techniques.
Rapid Commun Mass Spectrom, 23, pp 228-236.
Desmeules J, Piguet V, Collart L, Dayer P (1994): Contributions of monoaminergic modulation in tramadol analgesics effects. Clin Pharmacol
Ther, 55, p 151.
95
Desmeules J, Piguet V, Collart L, Dayer P (1994): Yohimbine antagonism as a tool to assess the extent of monoaminergic effects-experience with tramadol. Experientia, 50, p 79.
Desmeules J, Piguet V, Collart L, Dayer P (1996): Contribution of monoaminergic modulation to the analgesics effect of tramadol. Br J
Pharmacol, 41, pp 7-12. activity of dorsal horn neurones in the rat: differential response to an intrathecal opiate administered pre or post formalin. Pain, 30:3, pp 349-360.
Dickenson AH, Sullivan AF (1987): Subcutaneous formalin-induced
Doherty TJ, Geiser DR, Rohrbach BW (1997): Effect of acepromazine and butorphanol on halotene minimum alveolar concentration in ponies. Equine
Vet J, 29, pp 370-373.
Doherty TJ and Frazier DL (1998): Effect of intravenous lidocaine on halothane minimum alveolar concentration in ponies. Equine Vet J, 30, pp
300-303.
Dowling P (2001): Managing chronic pain: the NSAIDs. Proceedings of
26 th WSAVA Congress.
Driessen B and Reimann (1989): Effects of tramadol on noradrenaline release from rat brain cortex slices N-S. Arch Pharmacol, 339, p 89.
Driessen B and Reimann W (1992): Interaction of the central analgesic, tramadol, with the uptake and release of 5-hydroxytryptamine in the rat brain in vitro. Br J Pharmacol, 105, pp 147–151.
96
Driessen B, Reimann W, Giertz H (1993): Effects of the central analgesic tramadol on the uptake and release of noradrenaline and in vitro. Br J
Pharmacol, 108, pp 806-811.
Duthie DJ (1998): Remifentanil and tramadol. Br J Anaesth, 81, pp 51-57.
Dzikiti TB, Hellebrekers LJ, van Dijk P (2003): Effects of intravenous lidocaine on isoflurane concentration, physiological parameters, metabolic parameters and stress-related hormones in horses undergoing surgery. J Vet
Med A Physiol Pathol Clin Med, 50, pp 190-195.
Eggers KA and Power I (1995): Tramadol. Br J Anaesth, 74, pp 247-249.
Eide PK (2000): Wind-up and the NMDA receptor complex from a clinical perspective. Eur J Pain, 4, pp 5-15.
Elghazali M, Barezaik IM, Abdel Hadi AA, Eltaybed FM, Al Masri J,
Wasfi IA (2007): The pharmacokinetics, metabolism and urinary detection time of tramadol in camels. Vet J, 178, pp 272-277.
England GC and Clarke KW (1996): Alpha 2 adrenoceptor agonists in the horse--a review. Br Vet J, 152, pp 641-657.
Epstein DH, Preston KL, Jasinski JL (2006): Abuse liability, behavioral pharmacology, and physical-dependence potential of opioids in humans and laboratory animals: lessons from tramadol. Biol Psychol, 73, pp 90-99.
Fields HL (1988): Sources of variability in the sensation of pain. Pain, 33, pp 195-200.
97
Fields HL (1988): Sources of variability in the sensation of pain. Pain, 33, pp 195-200.
Fikes LW, Lin HC, Thurmon JC (1989): A preliminary comparison of lidocaine and xilazine as epidural analgesics in pinies. Vet Surg, 18, pp 85-86.
Flecknell PA and Waterman-Pearson A (2000): Animal pain – an introduction. In: Pain management in animals. Ed WB Saunders, Philadelphia, p 1.
Florez J, McCarthy LE, Borison HL (1968): A comparative study in the cat of the respiratory effects of morphine injected intravenously and into the cerebrospinal fluid. J Pharmacol Exp Ther, 163, pp 448-455.
Friderichs E, Reimann W, Selve N (1991): Investigations on opioid and non-opioid components in tramadol antinociception. Naunyn-Schmiedebergs
Archives of Pharmacol, 344, p 72.
Friderichs E, Reimann W, Selve N (1992): Contribution of both enantiomers to antinociception of the centrally acting analgesic tramadol.
Naunyn-Schmiedebergs Archives of Pharmacol, 346, p 36.
Frink MC, Hennies HH, Englberger W, Haurand M, Wilffert B (1996):
Influence of tramadol on neurotransmitter systems of the rat brain.
Arzneimittelforshung, 46, pp 1029-1036.
Fu ES, Miguel R, Scharf JE (1997): Preemptive ketamine decreases postoperative narcotic requirements in patients undergoing abdominal surgery.
Anesth Analg, 84, pp 1086-1090.
98
Garcia-Quetglas E, Azanza JR, Sàdaba B, Munoz MJ, Gil I, Campanero
MA (2007): Phermacokinetics of tramadol enantiomers and their respective phase I metabolites in relation to CYP2D6 phenotype. Pharmacol Res, 55, pp
122-130.
Gasthuys F, Vandenhende C, de Moor A (1986): Study of some ionary parameters in horse serum and urine during halothane anaesthesia with xylazine premedication. J Vet Med, 33, pp 791-800.
Gasthuys F, Vandenhende C, de Moor A (1988): Biochemical changes in blood and urine during halothane anaesthesia with detomidine premedication in the horse. J Vet Med, 35, pp 655-664.
Gasthuys F, Martens L, Goosens L, De Moore A (1996): A quantitative and qualitative study of the diuretic effects of romifidine in the horse. J Assoc Vet
Anaesth, 23, pp 6-10.
Gaynor JS and Muir WW (2008): Handbook of veterinary pain management. Ed Mosby, 2 nd ed.
Gillen C, Haurand M, Kobelt DJ, Wnendt S (2000): Affinity, potency and efficacy of tramadol and its metabolites at the cloned human mu-opioid receptor. Naunyn Schmiedebergs Arch Pharmacol, 362, 116-121.
Giorgi M, Saccomani G, Daniello MR, Manera C, Soldani G, Ferrarini PL,
Giusani M (2006): In vitro metabolism of tramadol in horses: preliminary data.
Drug Met Drug Met Enz, p 124.
99
Giorgi M, Saccomani G, Lebkowska-Wieruszewska B, Kowalski C (2008):
Pharmacokinetic evaluation of tramadol and its major metabolites after single oral sustained tablet administration in the dog: a pilot study. Vet J, 28, article in press.
Glare P (1997): Problems with opiates in cancer pain: parenteral opioids.
Support Care Cancer, 5, pp 445–450.
(1998): Epidural injection of ketamine for perineal analgesia in the horse. Vet
Surg, 27, pp 384-391.
Gomez de Segura IA, De Rossi R, Santos M, San-Roman JL, Tendillo FJ
Gottschalk A and Smith DS (2001): New concepts in acute pain therapy:
Preemptive Analgesia. American Family Physician, 15:63, pp 1979-1984.
Green SA and Thurmon JC (1985): Epidural analgesia and sedation for selected equine surgeries. Equine Pract, 7, pp 14-19.
Greene SA.and Thurmon JC (1988): Xylazine: a review of its pharmacology and use in veterinary medicine. J Vet Pharmacol Ther, 11, pp
295–313.
Grond S and Sablotki A (2004): Clinical pharmacology of tramadol. Clin
Pharmacokin, 43, pp 879-923.
Grond S, Zech D, Lynch J, Schug S, Lehmann KA (1992): Tramadol-a weak opioid for relief of cancer pain. Pain Clinic, 5, pp 241-247.
100
Grond S, Meuser T, Zech D, Hennig U, Lehmann KA (1995): Analgesic efficacy and safety of tramadol enantiomers in comparison with the racemate: a randomised, double-blind study with gynaecological patients using intravenous patient-controlled analgesia. Pain, 62, pp 313-320.
Guedes AGP, Natalini CC, Robinson EP, Alves SDL, Oliveira ST (2005):
Epidural administration of tramadol as an analgesic technique in dogs submitted stifle surgery. Intern J Appl Res Vet Med, 3, pp 351-359.
Gutstein H and Akil H (2001): Opioid analgesics. In: The pharmacological basis pf therapeutics. Ed Goodman and Gilman’s, New York, pp 569-621.
Helley PW, Robertson SA, Fails AD (2007): Pain and its management. In:
Lumb & Jone’s, 4 th edn. Ed Blackwell, p 32.
Hennies HH, Friderichs E, Schneider J (1988): Receptor binding, analgesic and antitussive potency of tramadol and other selected opioids.
Arzneimittelforschung, 38, pp 877-880.
Himmelseher S, Auchter M, Pfenninger E, Georgieff M (1996): The effects of ketamine-isomers on neuronal injury and regeneration in rat hippocampal neurons. Anesth Analg, 83, pp 505-512.
Ide S, Minami M, Ishihara K, Uhl GR, Sora I, Ikeda K (2006): Mu opioid receptor-dependent and independent components in effects of tramadol.
Neuropharmacol, 51, pp 651-658.
Ilkiw J (2001): Local anesthesia and local anesthetic technique.
Proceedings of 26 th WSAVA Congress.
101
International Association for the Study of Pain (IASP) (1979): Pain terms: a list with definition and notes on usage. Pain 6, pp 249-252.
Kalpravidh M, Lumb WV, Wright M, Heath RB (1984): Analgesic effects of butorphanol in horses: dose-response studies. Am J Vet Res, 45, pp 211-
216.
Kariman A, Nowrouzian I, Bakhtiari J (2000): Caudal epidural injection of a combination of ketamine and xylazine for perineal analgesia in horses. Vet
Anesth Analg, 27, p 115.
Kats J (1995): Pre-emptive analgesia: Evidence, current status and future directions. Eur J Anaesth, 12:10, pp 8-13.
Kayser V, Besson JM, Guilbaud G (1992): Evidence for a noradrenergic component in the antinociceptive effect of the analgesic agent tramadol in an animal model of clinical pain, the arthritic rat. Eur J of Pharmacol, 224, pp 83-
88.
Kehlet H and Dahl JB (1993): The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg, 77, pp 1048-1056.
Kehlet H (1994): Postoperative pain relief-what is the issue? Br J Anaesth
72, pp 375-378.
Kelly DJ, Ahmad M, Brull S (2001): Preemptive analgesia I: physiological pathways and pharmacological modalities. Can J Anest, 48, pp 1000-1010.
102
Kelly DJ, Ahmad M, Brull S (2001): Preemptive analgesia II: recent advances and current trends. Can J Anest, 48, pp 1091-1101.
Kieffer BL (1999): Opioids: first lessons from knockout mice. Trends
Pharmacol Sci, 20, pp 19-26.
Kissin I (1996): Preemptive analgesia. Why its effect is not always obvious.
Anesthesiology, 84, pp 1015-1019.
Kissin I (2000): Preemptive analgesia. Anesthesiology, 93, pp 1138-1143.
Klide AM, Calderwood HW, Soma LR (1975): Cardiopulmonary effects of xylazine in dogs. Am J Vet Res, 36, pp 931-935.
Ko JC, Abbot LA, Weil AB, Johnson BM, Inoue T, Payton ME (2008):
Effect of orally administered tramadol alone or with an intravenously administered opioid on minimum alveolar concentration of sevoflurane in cats.
JAVMA, 232, pp 1834-1840.
Kongara K, Chambers P, Johnson CB (2009): Glomerular filtration rate after tramadol, parecoxib and pindolol following anaesthesia and analgesia in comparison with morphine in dogs. Vet Anaesth Analg, 36, pp 86-94.
Koshers R and Durieux ME (1998): Ketamine: teaching an old drug new tricks. Anesth Analg, 87, pp 1186-1193.
Kromer W (1988): Endogenous and exogenous opioids in the control of gastrointestinal motility and secretion. Pharmacological reviews, 40, p 121.
103
Kronenberg RH (2002): Ketamine as an analgesic: parenteral, oral, rectal, subcutaneous, transdermal and intranasal administration.
J Pain Palliat Care
Pharmacother, 16, pp 27-35.
Kucuk A, Kadioglu Y, Celebi F (2005): Investigation of the pharmacokinetics and determination of tramadol in rabbit plasma by a highperformance liquid chromatography-diode array detector method using liquidliquid extraction. J Chromatogr B Analyt Technol Biomed Life Sci, 816, pp
203-208.
Kukanich B and Papich MG (2004): Pharmacokinetics of tramadol and the metabolite O-desmethyltramadol in dogs. J Vet Pharmacol Ther, 27, pp 239-
246.
Lascelles DB, Butterworth SJ, Waterman AE (1994): Postoperative analgesic and sedative effects of carprofen and pethidine in dogs. Vet Rec, 19, pp 187-191.
Lascelles DB, Cripps P, Mirchandani S, Waterman AE (1995): Central sensitization as a result of surgical pain: investigation of the pre-emptive value of pethidine for ovariohysterectomy in the rat. Pain, 62, pp 201-212.
Laverty S, Pascoe JR, Ling GV, Lavoie JP, Ruby AL (1992): Urolithiasis in
68 horses. Vet Surg, 21, pp 56-62.
LeBlanc PH, Caron JP, Patterson JS, Brown M, Matta MA (1988):
Epidural injection of xylazine for perineal analgesia in horses. J AmVet Med
Assoc, 193, pp 1405-1408.
104
Lee CR, McTavish D, Sorkin EM (1993): Tramadol. A preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in acute and chronic pain states. Drugs, 46, pp 323-340.
Lees P, Taylor JBO, Higgins AJ, Sedgwick AD (1988): In vitro and in vivo binding of phenylbutazone and related drugs to equine feeds and digesta. Res in Vet Science, 44, pp 50-56.
(1990): Postoperative patient-controlled analgesia with tramadol: analgesic efficacy and minimum effective concentrations. Clin J Pain, 6, pp 212-220.
Lehmenn KA, Kratzenberg U, Schoeder-Bark B, Horrichs-Haemeyer G
Lerche P, Nolan AM, Reid J (2000): Comparative study of propofol or propofol and ketamine for the induction of anaesthesia in dogs. Vet Rec, 146, pp 571-574.
Lester GD, Merrit AM, Neuwirth L, Vetro-Widenhouse T, Steible C, Rice
B (1998): Effect of alpha 2-adrenergic, cholinergic, and nonsteroidal antiinflammatory drugs on myoelectric activity of ileum, cecum, and right ventral colon and on cecal emptying of radiolabeled markers in clinically normal ponies. Am J Vet Res, 59, pp 320-327.
Lewis JW, Cannon JT, LiebenskindJC (1983): Involvement of central muscarinic cholinergic mechanisms in opioid stress analgesia. Brain Res, 270, pp 289-93.
Malone E and Graham L (2002): Management of gastrointestinal pain. Vet
Clin North Am Equine Pract, 18, pp 133-158.
105
Mao J and Chen LL (2000): Systemic lidocaine for neuropathic pain relief.
Pain, 87, p 717.
Martin WR (1984): Pharmacology of opioids. Pharmacological reviews, 35, pp 283-323.
Mastrocinque S and Fantoni DT (2003): A comparison of postoperative tramadol and morphine for the control of early postoperative pain in canine ovarihysterectoomy. Vet Anaesth Analg, 30, pp 220-228.
Mathews K (2001): Perioperative use of nonsteroidal anti-inflammatory analgesics. Proceedings of 26 th WSAVA Congress. halothane minimal alveolar concentration in ponies. Equine Vet J, 22, pp 325-
327.
Matthews NS and Lindsay SL (1990): Effect of low-dose butorphanol on
Mayer DJ and Liebeskind JC (1974): Pain reduction by focal electrical stimulation of the brain: an anatomical and behavioral analysis. Brain Res, 15, pp 73-93.
Maze M and Tranquilli W (1991): Alpha-2 adrenoceptor agonists: defining the role in clinical anesthesia. Anesthesiology, 74, pp 581-605.
McCallister CG (1993): Comparison of adverse effects of phenylbutazone, flunixin meglumine, and ketoprofen in horses. J Am Vet Med Assoc, 202, pp
71-77.
McCarberg B (2007): Tramadol extended-release in the management of chronic pain. Ther Clin Risk Manag, 3, pp 401-410.
106
McLeod WM and Frank ER (1927): A preliminary report regarding epidural anesthesia in equines and bovines. J Am Vet Med Ass, 72, pp 327-
335.
McMillan CJ, Livingston A, Clark CR, Dowling PM, Taylor SM, Duke T,
Terlinden R (2008): Pharmacokinetics of intravenous tramadol in dogs. Can J
Vet Res, 72, pp 325-331.
McQuay HJ (1992): Preemptive analgesia. Br J Anaesth, 69, pp 1-3.
Melzack R and Wall PD (1965): Pain mechanism: a new theory. Science,
19, pp 971-999.
Merrit AM, Burrow JA, Hartless CS (1998): Effect of xylazine, detomidine, and a combination of xylazine and butorphanol on equine duodenal motility.
Am J Vet Res, 59, pp 619-623.
Millan MJ (2002): Descending control of pain. Progress in Neurobiology,
66, pp 355-474.
Moore AS, Rand WM, Berg J (1994): Evaluation of butorphanol and cyproheptadine for prevention of cisplatin-induced vomiting in dogs. J Am Vet
Med Ass, 205, pp 441-443.
Morgan P, Lynn AM, Parrot C, Morray JP (1987): Hemodynamic and metabolic effects of two anesthetic techniques in children undergoing surgical repair of acyanotic congenital heart disease. Anesth Analg, 66, pp 1028-1030.
107
Moses VS and Bertone AL (2002): Nonsteroidal anti-inflammatory drugs.
Vet Clin North Am Equine Pract, 18, pp 21-37.
Muir WW, Skarda RT, Sheehan W (1979): Hemodynamic and respiratory effects of xylazine-morphine sulfate in horses. Am J Vet Res, 40, pp 1417-
1420.
Muir WW (1991): Standing chemical restraint in horses: tranquilizers, sedatives and analgesics. In: Equine Anesthesia. Monitoring and Emergency
Therapy. Muir WW, ed Hubbell JAE Mosby, St Louis, pp 247-280.
Muir WW III and Sams R (1992): Effects of ketamine infusion on halothane minimal alveolar concentration in horse. Am J Vet Res, 53, pp 1802-
1806.
Murrel JC, While KL, Johnson CB, Taylor PM, Doherly TJ, Waterman-
Pearson AE (2005): Investigation of the EEG effects of intravenous lidocaine during halothane anaesthesia in ponies. Vet Anaesth Analg, 32, pp 212-221.
Natalini CC and Robison EP (2000): Evaluation of the analgesic effects of epidurally administered morphine, alfentanil, butorphanol, tramadol, and
U50488H in horses. Am J Vet Res, 61, pp 1579-1586.
Natalini CC and Robinson EP (2003): Effects of epidural opioid analgesics on heart rate, arterial blood pressure, respiratory rate, body temperature, and behaviour in horses. Vet Therap, 4, pp 364-375.
Nebbia C, Dacasto M, Rossetto Giaccherino A, Giuliano Albo A, Carletti
M (2003): Comparative expression of liver cytochrome P450-dependent
108 monooxygenases in the horse and in other agricultural and laboratory species.
Vet J, 165, pp 53-64.
Neges K, Bettschart-Wolfensberger R, Muller J, Furst A, Kastner S (2003):
The isoflurane sparing effect of a medetomidine costant rate in horses. Vet
Anaesth Analg, 30, pp 93-94.
Nolan AM and Hall LW (1984): Combined use of sedatives and opiates in horses. Vet Rec, 114, pp 63-67.
Nolan AM and Hall LW (1984): Combined use of sedatives and opiates in horses. Vet Rec, 114, pp 63-67.
Nolan AM, Livingston A, Waterman A (1987): Antinociceptive actions of intravenous alpha 2-adrenoceptor agonists in sheep. J Vet Pharmacol and
Therap, 10, pp 202-209.
Nolan AM and Reid J (1991): The use of intraoperative fentanyl in spontaneously breathing dogs undergoing orthopaedic surgery. J of Vet
Phermacol and Therap, 17, pp 323-326.
Nolan A, Reid J, Welsh E, Flaherty D, McCormack R, Monteiro AM
(1996): Simultaneous infusions of propofol and ketamine in ponies premedicated with detomidine: a pharmacokinetic study. Res Vet Sci, 60, pp
262-266.
Nunez E, Steffey EP, Ocampo L, Rodriguez A, Garcia AA (2001): Effect of xylazine and detomidine on urine production in horses deprived of food and
109 water. Proceedings Annual Meeting of the American Association of Veterinary
Anaesthesiologists, New Orleans.
Owens JG, Kamerling SG, Stanton SR, Keowen ML (1996): Evaluation of detomidine-induced analgesia in horses with chronic hoof pain. J Pharmacol
Exp Ther, 278, pp 179-184.
Paar WD, Poche S, Gerloff J, Dengler HJ (1997): Polymorphic CYP2D6 mediates O-demethylation of the opioid analgesic tramadol. Eur J Clin
Pharmacol, 53, pp 235-239.
Pape J and Pitzschk K (1925): Versuche ueberextradurale anaesthesie beim pferde. Arch Wiss Prackt Tierheilkd, 52, pp 558-571.
Porreca F, Ossipov MH, Gebhart GF (2002): Chronic pain and medullary descending facilitation. Trends in Neurosciences, 25, pp 319-325.
Pretson KL, Jasinski DR, Testa M (1991): Abuse potential and pharmacological comparison of tramadol and morphine. Drug Alcohol
Depend, 27, pp 7-17. metabolite O-desmethyl-tramadol, in cats. J Vet Pharmacol Therap, 31, pp 52-
59.
Pypendop BH and Ilkiw JE (2007): Pharmacokinetics of tramadol, and its
Raekallio M, Taylor PM, Bennet RC (1997): Preliminary investigations of pain and analgesia assessment in horses administered phenylbutazone or placebo after arthroscopy surgery. Vet Surg, 26, pp 150-155.
110
Raffa RB, Friderichs E, Reimann W, Shank RP, Codd EE, Vaught JL
(1992): Opioid and nonopioid components independently contribute to the mechanism of action of tramadol, an 'atypical' opioid analgesic. J Pharmacol
Exp Ther, 260, pp 275–285.
Raffa RB, Friderichs E, Reimann W, Shank RP, Codd EE, Vaught JL,
Jacoby HI, Selve N (1993): Complementary and synergistic antinociceptive interaction between the enantomers of tramadol. J Pharmacol Exp Ther, 267, pp 331-340.
Raffa RB, Nayak RK, Liao S, Minn FL (1995): The mechanism of action and pharmacokinetics of tramadol hydrochloride. Rev Cont Pharmacol, 6, pp
485-498.
Raffa RB (2008): Basic pharmacology relevant to drug abuse assessment: tramadol as example. J Clin Pharm Therap, 33, pp 101-108.
Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC (1997): Pain affect encoded in human anterior cingulate but not somatosensory cortex.
Science, 15, pp 968-971.
Reimann W, Driessen B, Schlutz H (1990): Does a non-opioid component contribute to the efficacy of the central analgesic tramadol? Proceedings of 10 th
European Winter Conference on Brain Research.
Reimann W and Hennies HH (1994): Inhibition of spinal noradremaline uptake in rats by the centrally acting analgesic tramadol. Bioch Pharmacol, 47, pp 2289-2293.
111
Reynolds DV (1969): Surgery in the rat during electrical analgesia induced by focal brain stimulation. Science, 25, pp 444-445.
Ringer SK, Kalchofner K, Boller J, Furst A, Bettschart-Wolfensberger R
(2007): A clinical comparison of two anaesthetic protocols using lidocaine or medetomidine in horses. Vet Anaesth Analg, 34, pp 257-268.
Robinson EP and Natalini CC (2002): Epidural anaesthesia and analgesia in horses. Vet Clin North Am Equine Pract, 18, pp 61-82.
Schatzmann U, Jossfck H, Stauffer JL, Goossens L (1994): Effects of alpha
2-agonists on intrauterine pressure and sedation in horses: comparison between detomidine, romifidine and xylazine. Zentralbl Veterinarmed A, 41, pp 523-
529.
Scott LJ and Perry CM (2000): Tramadol: a review of its use in perioperative pain. Drugs, 60, pp 139-176.
Sellon DC, Monroe VL, Roberts MC, Papich MG (2001):
Pharmacokinetics and adverse effects of butorphanol administered by single intravenous injection or continuos intravenous infusion in horses. Am J Vet
Res, 62, pp 183-189.
Sevcik J, Nieber K, Driessen B, Illes P (1993): Effects of the central analgesic tramadol and its main metabolite, O-desmethyltramadol, on rat locus coeruleus neurons. Br J Pharmacol, 110, pp 169-176.
112
Sheely JG, Hellyer PW, Sammonds GE, Mama KR, Powers BE,
Hendrickson DA, Magnusson KR (2001): Evaluation of opioid receptors in synovial membranes of horses.
Am J Vet Res, 62, pp 1408-1412.
Shilo Y, Britzi M, Eytan B, Lifschitz T, Soback S, Steinman A (2008):
Pharmacokinetics of tramadol in horses after intravenous, intramuscolar and oral administration. J Vet Pharmacol Therap, 31, pp 60-65.
Shipton EA (2000): Tramadol-present and future. Anaesth Intensive Care,
28, pp 363-374.
Shipton EA (2000): Tramadol-present and future. Anaesth Intensive Care,
28, pp 363-374.
Simonin F, Valverde O, Smadja C, Slowe S, Kitchen I, Dierich A, Le Meur
M, Roques BP, Maldonado R, Kieffer BL (1998): Disruption of the kappaopioid receptor gene in mice enhances sensitivity to chemical visceral pain, impairs pharmacological actions of the selective kappa-agonist U-50,488H and attenuates morphine withdrawal. EMBO J, 16, pp 886-897.
Skarda RT (1991): Local Anesthetics and local anesthetic techniques in horses. In: Equine Anesthesia, Mosby ed, St. Luis, pp 199-246.
Skarda RT and Tranquilli WJ (2007): Local Anesthetics. In: Tranquilli WJ,
Thurmon JC, Grimm KA Lumb end Jone’s Veterinary anesthesia and analgesia. 4 th ed, Blackwell Publishing.
113
Souza MJ, Greenacre CB, Cox SK (2008): Pharmacokinetics of orally administered tramadol in domestic rabbits (Oryctolagus cuniculus). Am J Vet
Res, 69, pp 979-982.
Steagall PVM, Taylor PM, Brondani JT, Luna SPL, Dixon MJ (2008):
Antinociceptive effects of tramadol and acepromazine in cats. J Feline Med
Surg, 10, 24-31. respiratory effects of acetylpromazine and xylazine on halothane anesthetized horses. J Vet Pharmacol Therap, 8, 290-302.
Steffey EP, Kelly AB, Farver TB, Woliner MJ (1985): Cardiovascular and
Steffey EP, Pascoe PJ, Woliner MJ, Berryman ER (2000): Effects of xylazine hydrochloride during isoflurane-induced anaesthesia in horse. Am J
Vet Res, 61, pp 1225-1231.
Steffey EP, Eisele JH, Baggot D (2003): Interactions of morphine and isoflurane in horses. Am J Vet, 64, pp 166-175.
Stein C (1993): Peripheral opioid receptors and their role in postoperative pain management. Schmerz, 7, pp 4-7.
Stenberg D (1986): The role of alpha-adrenoceptors in the regulation of vigilance and pain. Acta Vet. Scand, 82, pp 29-34.
Stephens J, Laskin B, Pashos C, Pena B, Wong J (2003): The burden of acute postoperative pain and the potential role of the COX-2-specific inhibitors. Rheumatology (Oxford), 42, pp 40-52.
114
Stoelting RK (1999): Pharmacology and physiology in anesthetic practice.
3 rd ed, Philadelphia Publisher, pp 77-112.
Subrahmanyam V, Renwick AB, Walters DG, Young PJ, Price RJ, Tonelli
AP, Lake BG (2001): Identification of cytochrome P-450 isoforms responsible for cis-tramadol metabolism in human liver microsomes. Drug Metab Dispos,
29, pp 1146-1155.
(2002): The effects of xylazine, detomidine, acepromazine and butorphanol on equine solid phase gastric emptying rate. Equine Vet J, 34, pp 486-492.
Sutton DG, Preston T, Christley RM, Cohen ND, Love S, Roussel AJ
Suzuki R, Rygh LJ, Dickenson AH (2004): Bad news from the brain: descending 5-HT pathways that control spinal pain processing. Trends in
Pharmacological Sciences, 25, pp 613-617.
Sysel AM, Pleasant SR, Jacobson JD (1996): Efficacy of an epidural combination of morphine and detomidine in alleviating experimentally induced hindlimb lameness in horses. Vet Surg, 25, pp 511-518.
Sysel AM, Pleasant SR, Jacobson JD, Moll HD, Warnick LD, Sponenberg
DP, Eyre P (1997): Systemic and local effects associated with long-term epidural catheterization and morphine-detomidine administration in horses.
Vet Surg, 26, pp 141-149.
Tao Q, Stone DJ, Borenstein MR, Codd EE, Coogan TP, Desai-Krieger D,
Liao S, Raffa RB (2002): Differential tramadol and O-desmethyl metabolite levels in brain vs. plasma of mice and rats administered tramadol hydrochloride orally. J Clin Pharm Ther, 27, pp 99-106.
115
Taylor PM (2003): Pain and analgesia in horses. Vet Anaesth Analg, 30, pp
121-123.
Teppema LJ, Nieuwenhuijs D, Olivier CN, Dahan A (2003): Respiratory depression by tramadol in the cat. Anesthesiology, 98, pp 420-427.
Thurmon JC, Neff-Davis CA, Davis LE, Stoker RA, Benson GJ, Lock TF
(1982): Xylazine hydrochloride-induced hyperglycemia and hypoinsulinemia in thoroughbred horses. J Vet Pharmacol Ther, 5, pp 241-245.
Thurmon JC, Steffey inkl JG, Woloner M, Howland D Jr (1984): Xylazine causes transient dose-related hyperglycemia and increased urine volumes in mares. Am J Vet Res, 45, pp 224-27.
Tobin T and Miller JR (1979): The pharmacology of narcotic analgesics in the horse. I. The detection, pharmacokinetics and urinary clearance times of pentazocine. J Equine Med and Surg, 3, pp 191-198.
Tranquilli WJ, Thurmon JC, Neff-Davis CA, Davis LE, Benson GJ,
Hoffman W, Lock TF (1984) : Hyperglycemia and hypoinsulinemia during xylazine-ketamine anesthesia in thoroughbred horses. Am J Vet Res, 45, pp
11-14.
Tranquilli JW, Thurmon JC, Grimm KA (2007) : Lumb & Jones’
Veterinary anesthesia and analgesia. 4 th ed, Blackwell Publishing.
Tuncer S, Pirbudak L, Balat O, Capar M (2003): Adding ketoprofen to intravenous patient-controlled analgesia with tramadol after major
116 gynecological cancer surgery: a double-blinded, randomized, placebocontrolled clinical trial. Eur J Gynaecol Oncol, 24, pp 181-184.
Tverskoy M, Oz Y, Isakson A, Finger J, Bradley EL Jr, Kissin I (1994):
Preemptive effect of fentanyl and ketamine on postoperative pain and wound hyperalgesia. Anesth Analg, 78, pp 205-209.
Valverde A, Little CB, Dyson DH, Motter CH (1990): Use of epidural morphine to relieve pain in a horse. Can Vet J, 31, pp 211-212.
Valverde A and Gunkel CI (2005): Pain management in horses and farm animals. J Vet Emerg Crit Care, 15, pp 295-307.
Vettorato E, Zonca A, Isola M, Villa R, Gallo M, Ravasio G, Beccaglia M,
Montesissa C, Cagnardi P (2009): Pharmacokinetics and efficacy of intravenous and extradural tramadol in dogs. Vet J, 10, artiche in press.
Wagner AE, Muir WW, Hinchcliff KW (1991): Cardiovascular effects of xilazine and detomidine in horses. Am J Vet Res, 52, pp 651-657.
Wall PD (1988): The prevention of postoperative pain. Pain 33, pp 289-
290.
Wall PD (1988): The prevention of postoperative pain. Pain, 33, pp 289-
290.
Watson ZE, Steffey EP, VanHoogmoed LM, Snyder JR (2002): Effect of general anesthesia and minor surgical trauma on urine and serum measurements in horses. Am J Vet Res, 63, pp 1061-1065.
117
Welch J (2005): Analgesics agent. Proccedings of 2005 AVDS Diplomate
Resorte Meeting, pp 73-77.
Williams DR and Strark RJ (2003): Intravenous lignocaine (lidocaine) infusion for the treatment of chronic daily headache with substantial medication overuse. Cephalalgia, 23, pp 963-971.
Willis WD Jr (1986): Ascending somatosensory system. In: Spinal afferent processing. Ed Yaksh TL, New York, pp 398-416. associated with administration of detomidine into the caudal epidural space in a horse.
J Vet Med Assoc, 213, pp 516-518.
Wittern C, Hendrickson DA, Trumble T, Wagner A (1998): Complications
Wong BS and Martin CD (1993): Ketamine inhibition of cytoplasmic calcium signalling in rat pheochromocytoma (PC-12) cells. Life Sci, 53, pp
359-364.
Wong CS, Shen TT, Liaw WJ, Cheng CH, Ho ST (1996): Epidural coadministration of ketamine, morphine and bupivacaine attenuates postherpetic neuralgia-a case report. Acta Anaesthesiol Sin, 34, pp 151-155.
Woolf CJ and Wall PD (1986): Morphine-sensitive and morphineinsensitive actions of C-fibre input on the rat spinal cord. Neurosci Lett, 28, pp
221-225.
Woolf CJ (1989): Recent advances in the pathophysiology of acute pain. Br
J Anaesth, 63, pp 139-146.
118
Woolf CJ (1991): Generation of acute pain: central mechanisms. Br Med
Bull, 47, pp 523-533.
Woolf CH and Chong MS (1993): Preemptive analgesia--treating postoperative pain by preventing the establishment of central sensitization.
Aneath Analg, 77, pp 362-379.
Wu NM, McKown NA, Gauthier AD, Jones WJ, Raffa RB (2001):
Metabolism of the analgesic drug, tramadol hydrochloride, in rat and dog.
Xenobiotica, 31, pp 423-441.
Wu WN, McKown NA, Codd EE, Raffa RB (2006): Metabolism of two analgesic agents, tramadol-n-oxide and tramadol, in specific pathogen-free and axenic mice. Xenobiotica, 36, pp 551-565.
Zaho Y, Tao T, Wu J, Pi J, He N, Chai X, Chen Q (2008):
Pharmacokinetics of tramadol in rat plasma and cerebrospinal fluid after intranasal administration. J Pharm Pharnacol, 60, pp 1149-1154.