Histology of the Skin (Integumentary System)
advertisement

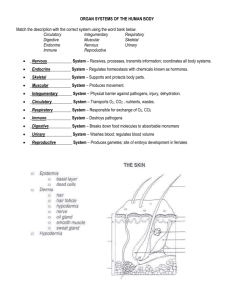
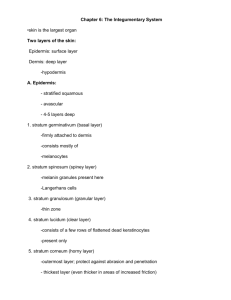
THE SKIN (INTEGUMENTARY SYSTEM) Rhonda Ghorbani, MD Reading: Klein and McKenzie, pp 211-219; Gartner and Hiatt Chapter 11, p217 Learning Objectives: List the basic functions of the skin and describe its overall structure Describe basic skin embryology State the names of the layers of the epidermis and how to distinguish them histologically Explain ultrastructural (electron microscopic) features of the epidermis and the epidermal/dermal junction Describe the process of keratinization in the epidermis, hair, and nail Describe the formation of the water barrier in the epidermis Name the non-keratinocytic cells in the epidermis and state their functions Explain the structure and components of the dermis, including types of nerves and vascular system State the segments and layers of the hair follicle Describe the relationship between hair size and phase of hair growth Describe the structure, location, and function of different types of cutaneous glands Describe the structure and growth of the nail Key Words: arrector pili muscle, dermal papillae (dermal ridges), dermal sheath, dermis, duct of sweat gland, epidermis, external root sheath, glassy membrane, hair bulb, hair follicle, hair matrix, hair papilla, hair root, hair shaft, hypodermis, internal root sheath, interpapillary pegs (rete pegs), Meissner's corpuscle, melanocytes of epidermis, melanosomes (melanin granules), myoepithelial cell, Pacinian corpuscle, papillary layer of dermis, reticular layer of dermis, sebaceous gland, stratum basale, stratum corneum, stratum granulosum, stratum lucidum, stratum spinosum, sweat gland INTRODUCTION Skin is one of the largest organs in the human body, representing 15-20% of total body weight. It serves many functions, including: S – SENSATION (it is a receptor for pain, pressure, touch, temperature) C – CONVERSION (of precursor molecules into vitamin D) R – REGULATION (of heat) A – ABSORPTION (of certain lipid-soluble therapeutic substances) P – PROTECTION (against injury of many kinds) & PREVENTION (of water loss) E – EXCRETION (of waste products via sweat glands) The skin can be divided into compartment EMBRYOLOGY Epidermis: single-layered ectoderm multilayered periderm stratified squamous epithelium o Vernix caseosa: desquamated periderm/epidermis; slippery; protective and aids in birth Dermis: mesoderm mesenchyme dermis composed of multiple cell types Hair: epidermal invagination lanugo hairs (fine, lightly pigmented) mature hairs Melanocytes: neural crest become melanoblasts in mesenchyme mature in epidermis EPIDERMIS Avascular layers of keratinocytic and non-keratinocytic cells Thickness ranges from 0.1 – 1.0 mm, depending on location o The terms “thin” and “thick” skin refer to the thickness of the epidermis o Thin skin = hairy skin (most of the body) o Thick skin = hairless skin (glabrous skin on palmar/plantar surfaces, i.e. palms/soles) KERATINOCYTES Squamous cells which form a stratified epithelium and are the major cellular components of the epidermis Migrate from the basal layer to the superficial surface over a period of about 3-4 weeks (approximately 26 days) UPPER LAYERS OF EPIDERMIS LOWER LAYERS OF EPIDERMIS (stratum Malpighi or Malpighian layer) KERATINIZATION Keratohyaline granules are rich in histidine, cystine, and filaggrin Filaggrin combines with cytoplasmic filaments in the process of keratinization Cells undergo keratinization after leaving the stratum granulosum and entering the stratum corneum Keratinization involves breakdown of nucleus and organelles and thickening of plasma membrane Stratum corneum = dead cells with thick plasma membranes, cytoplasmic filaments, and interfilamentous matrix Types of keratin: o Soft keratin: produced via granules (e.g. in the epidermis) o Hard keratin: produced without granules (e.g. in the hair and nails) It is hard because there are many disulfide bonds WATER BARRIER Lipid-containing lamellar granules (a.k.a. Odland bodies) are produced by the Golgi of keratinocytes and are discharged into the intercellular space by cells of the stratum granulosum Released lipid localizes to the lower stratum corneum, forming a barrier to water loss NON-KERATINOCYTIC CELLS OF EPIDERMIS MELANOCYTES Round cells with clear cytoplasm and basophilic nuclei by H&E stain Have long dendritic processes (not visible by H&E) which extend between keratinocytes Located within the basal layer of the epidermis and in hair follicles Do not establish desmosomal attachments with keratinocytes; instead, they bind to the basal lamina via hemidesmosomes Contain premelanosomes (visible only by electron microscopy), which are membrane-bound spherical and elliptical organelles produced by Golgi The enzyme tyrosinase is responsible for the production of melanin within premelanosomes: tyrosine 3,4-dihydroxyphenylalanine (DOPA) dopaquinone melanin Skin color is influenced by: o Melanin: pigment within melanosomes Types: eumelanin (usual type) and pheomelanin (blonde and red hair) Number of melanocytes in normal skin is constant among races – approximately 1 melanocyte per 4-10 basal keratinocytes – but may vary from region to region within an individual Degree of skin pigmentation is dependent on melanosomes in keratinocytes – their number, size, location within the cell (closer to the nucleus in fair-skinned), stability, and degree of melanization Tanning is due to increased rates of melanin darkening, transfer of melanosomes to keratinocytes, and melanin production Increased pigment shields nucleic acids and proteins from UV radiation Gray hairs are due to decreased number and activity of melanocytes in follicular bulbs Oxyhemoglobin: in dermal vascular bed Carotenes: food pigment in fat-containing tissues Exogenous minerals (e.g. tattoos) Hemoglobin breakdown products (e.g. hemosiderin, bilirubin) The basal laminae separate the epidermis from the dermis and form a network of components keeping the epidermis connected to the dermis Most EDJ components are only visible by electron microscopy Regions of the EDJ: o Basal keratinocyte o Lamina lucida: electron-lucent zone o Lamina densa: electron-dense zone o Sublamina densa: uppermost papillary dermis Individual structures of the EDJ: o Hemidesmosome: attaches basal keratinocyte to basal lamina o o Anchoring filament: attaches hemidesmosome to basal lamina Extends from inner plasma membrane to lamina densa Anchoring fibril: tethers epidermis to dermis Extends from lamina densa into papillary dermis, terminating on an anchoring plaque Traps collagen within a fibrillar network which enhances attachment DERMIS Composed of collagen, elastic fibers, ground substance (amorphous extracellular material) and fibroblasts o Collagen accounts for > 70% of skin’s dry weight o Type I collagen is the most abundant, followed by type III (in adults) o Provides support and strength to the skin Contains blood and lymphatic vessels, nerve endings, and cutaneous adnexal structures Contains striated muscle fibers in the face and neck Contains smooth muscle fibers in the external genitalia and areola NERVES Efferent nerve fibers: innervate blood vessels, adnexal structures, smooth muscle Free afferent nerve endings: nociceptors (pain receptors) in epidermis and dermis Encapsulated nerve endings: nerve end organs o Meissner corpuscle: mechanoreceptor (tactile) Located high in dermal papillae of palms, soles, digits, nipples, lips Cylindrical or pear-shaped Zigzag arrangement of unmyelinated terminal afferent nerve fibers with supporting (laminar) cells thought to be Schwann cells Can be seen by routine light microscopy but difficult to locate o Pacinian corpuscle: mechanoreceptor (pressure) Located in deep dermis or subcutis of weight-bearing and sensitive areas Ovoid; resembles a cut onion Contains a terminal afferent nerve fiber which loses its myelin after entering the corpuscle, and has supporting (laminar) cells thought to be Schwann cells BLOOD VESSELS Horizontal plexuses of superficial (in upper reticular dermis) and deep (in lower reticular dermis) arterioles and venules joined by vertical communicating vessels CUTANEOUS ADNEXAL STRUCTURES (SKIN ADNEXAE) There are different types of adnexal structures within the skin, mainly within the dermis: o Pilosebaceous unit = hair follicle + sebaceous gland Sebaceous glands may exist independently in limited locations o Eccrine gland o Apocrine gland HAIR FOLLICLE Present over entire body except: sides and volar surfaces of hands/feet, lips, around urogenital orifices Rate of hair growth: few tenths of 1 mm/day Hair functions: protection (of nasal passage from particulate matter, of scalp from sun, of eyes from sun and sweat), reduction of heat loss, decoration The infundibulum is a continuation of the epidermis o It contains the pilosebaceous canal, through which the hair shaft and sebum pass o The intraepidermal segment is called the acrotrichium The arrector pili muscle is a bundle of smooth muscle which attaches to the connective sheath surrounding the hair follicle o Arrector pili muscle contraction results in “goose pimples” (erect hair follicles) Hair size: o Terminal: long, coarse, heavily pigmented; produced by long follicles; spend a long time in anagen; e.g. scalp, axilla, pubis o Vellus: short, thin, lightly pigmented; produced by small follicles; spend a long time in telogen Conversion of terminal to vellus hairs is one of the causes of baldness Melanin production by melanocytes in the hair follicle contributes to hair shaft pigmentation Hair follicle keratinization: o Hair shaft layers (medulla, cortex, and cuticle) keratinize without granules; thus, hair keratin is hard keratin o Inner root sheath layers keratinize via trichohyaline granules, which stain eosinophilic (in contrast to basophilic keratohyaline granules in the epidermis); thus, inner root sheath keratin is soft keratin When fully keratinized cells of the inner root sheath reach the isthmus, they disintegrate; therefore, they do not contribute to the exiting hair o Outer root sheath keratinization is called tricholemmal keratinization (tricho- meaning hair), and it also occurs without granules, producing hard keratin This occurs at the isthmus, after the inner root sheath has disintegrated SEBACEOUS GLAND Present in all skin except palms and soles Most numerous and most productive on scalp and face Largest on nose, forehead, and upper back Hormonally responsive (therefore, well-formed in neonates and during the reproductive years, but small and inactive during other periods of life) Formed by cells of the outer root sheath, usually several lobulated glands (saccules) to one hair follicle ECCRINE GLAND (SWEAT GLAND) Located over the entire body except: lips, some external genital structures, external auditory canal Embryology: downgrowths from periderm into mesenchyme Highest concentration in the palms, soles, forehead, axilla [note: in these regions, the eccrine glands respond primarily to emotional stimuli, whereas those in other regions respond to thermal stimuli] Functions: thermoregulation (cooling results from sweat evaporation) and excretion Secretory portion: o Located in deep dermis or upper subcutis o 2 different types of secretory cells: staining differences may not be prominent by H&E Clear cells: contain glycogen; located between dark cells and myoepithelial cells Dark cells: contain mucopolysaccharide; located luminally o Merocrine secretion o Surrounded by a row of myoepithelial cells, which contract to move secretions out of gland Duct portion: o Stratified cuboidal epithelium without myoepithelial cells o Leaves the secretory portion as a coiled duct, then becomes straight o Spirals through the epidermis to the skin surface as the acrosyringium Sweat is a watery solution low in protein; it contains NaCl, urea, uric acid, and ammonia Innervated by the sympathetic nervous system and stimulated by cholinergic transmitters in response to heat and acute stress APOCRINE GLAND Located in axilla, areola, perineum, circumanal region, external genitalia, external ear canal (ceruminous glands), and eyelid (Moll’s glands) Small and nonfunctional until puberty Secretory portion: Duct portion: o Two layers of cuboidal cells and an inner cuticle but no myoepithelial cells o Travels from the secretory portion and empties into the infundibulum of the hair follicle, above the entrance of the sebaceous duct Considered a type of sweat gland but are not “the sweat glands” Secreted product becomes odiferous as the result of bacterial decomposition Innervated by sympathetic nervous system and stimulated by adrenergic transmitters in response to emotional and sensory stimuli SUBCUTIS (HYPODERMIS; PANNICULUS ADIPOSUS; SUBCUTANEOUS FAT) Deep to dermis and superficial to skeletal muscle Lobules of adipose tissue surrounded by fibrous tissue septae NAIL Overlies a richly vascular dermis that is contiguous with distal phalangeal periosteum Nail root: proximal part of nail buried under proximal nail fold Nail matrix: germinative epithelium of basaloid cells under the root that differentiates into the nail plate (keratinizes without granules hard keratin) and into some of the cells of the nail bed Lunula: crescent-shaped pale area near the root, just distal to the proximal nail fold o Especially prominent on the thumb o Thought to be due to thick layer of matrix (obscuring pink color imparted by blood vessels) and incomplete cornification of nail Eponychium (cuticle): cornified edge of proximal nail fold o Seals off potential space between fold and nail Hyponychium: epidermal thickening distal to nail bed that joins to undersurface of free edge of nail plate o Separated from volar (palm/sole) skin by the distal groove (not really a groove, but a slightly elevated margin) o Cornifies like volar skin INTEGUMENT (SKIN) LABORATORY SLIDES 10 and 39 – Thick Skin (HEEL or BIG TOE) Begin by holding the slide up to the light… 1. The basophilic rim around the outer portion of the tissue on one side is the epidermis. Note that the epidermis is no more than a couple of millimeters thick, even in this example of thick skin. 2. The pink layer underlying the epidermis is the dermis. 3. The subcutaneous tissue (the hypodermis or subcutis) contains adipose tissue, which produces a pale, lacy or lobulated appearance. The dermis itself may contain a small amount of fat, particularly in association with adnexal structures. Now, place your slide under the microscope… 1. Identify the layers of the epidermis (stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, stratum germinativum) and the epidermal-dermal junction. Next, move on to examination of the dermis. Low power: identify papillary and reticular dermis, rete ridges, dermal papillae, superficial and deep blood vessels, eccrine (sweat) glands, and eccrine ducts High power: identify nerve endings; examine the cellular composition of the dermis Meissner’s corpuscles in dermal papillae may be difficult to see in your slides. These are cylindrical or pear-shaped. View them on the demonstration slide. Questions: What are some functions of the rete ridges and dermal papillae? What is the major component of the dermis and how does it differ between the papillary and reticular dermis? How can you differentiate between eccrine glands and eccrine ducts based on their location and their cell layers? What skin appendages are not present on this (or any) slide of thick skin? 2. The hypodermis is predominantly composed of adipose tissue. Look for Pacinian corpuscles (although they may not be present on every slide). SLIDE 9 – SCALP (thin skin) 1. Identify once more the epidermal and dermal layers. Note the differences between thin skin (H-7) and thick skin (H-135 and H-111): the thinner overall epidermis, reduced thickness of the stratum corneum, absence of an identifiable stratum lucidum, reduced prominence of rete ridges, and presence of pilosebaceous units. 2. Low power: identify the following: Three segments of the hair follicle: infundibulum, isthmus, inferior segment; note how deeply the hair follicles extend in the scalp. Sebaceous gland 3. High power: identify the following: Layers of the hair follicle: inner and outer root sheath Look for red-staining trichohyaline granules in the middle layer of the inner root sheath Other features of the hair follicle Connective tissue sheath: surrounds the follicle Hair bulb: note the keratinocytes and melanocytes Dermal hair papilla: identify the dermal connective tissue extending into the bulb; some slides may show nerve endings and blood vessels in the hair papilla Hair: looks gold-brown and grainy on H&E-stained slides Arrector pili muscle Questions: Why do the cells of the outer root sheath appear “clear”? Where does the inner root sheath terminate? What type of secretion occurs in the sebaceous gland? SLIDE 51 – NIPPLE 1. Examine the epidermis. Note that the basal layer is deeply pigmented, which accounts for the darker skin color of the nipple and areola. 2. Examine the dermis. You may be able to identify a few apocrine glands in the deep reticular dermis. Questions: Does dark skin have more melanocytes and/or more melanosomes? What are the occasional deeply eosinophilic bundles with long, ovoid nuclei in the dermis? SLIDE 52 – NAIL Identify the following structures: nail plate, proximal nail fold, nail bed, root, matrix, eponychium, hyponychium. Questions: What type of keratin is produced by the matrix of the nail? How can you tell that by looking at this slide (hint – what’s NOT there?)? What epidermal layer does the nail plate resemble? What is the common name for the eponychium and what is its function?