Developing and Sustaining a Competent and Confident Clinical
advertisement

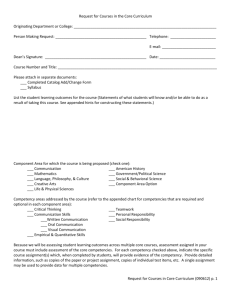
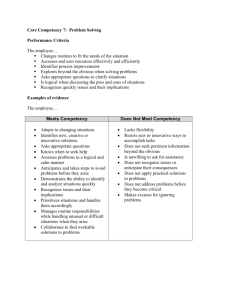
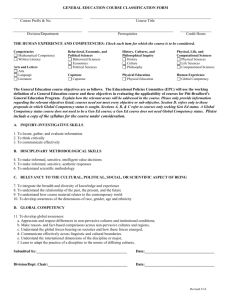
Developing and Sustaining a Competent and Confident Clinical Workforce through Essential Clinical Competencies for Registered Practitioners Competency Title: Documentation for Registered Nurses Competency Lead: Jacqueline Hazeldine Document Author Authorised Signature Written by: Jacqueline Hazeldine Authorised by: Richard Young Signed: Signed: Date: 10/05/2014 Date: 22 May 2014 Job Title: Modern Matron/Practice Educator Job Title: Head of Clinical Education and Resuscitation Effective Date: 1st June 2014 Review Date: 1St June 2017 Approval at: Clinical Competency Group Date Approved: 22 May 2014 1 CF /v10/DB/KB/GS2013 How to use this Competency Framework This Competency Framework has been developed to enable the assessment of clinical competence. In light of the Francis Report (and the move towards Foundation Trust status), the Isle of Wight NHS Trust is required to demonstrate that clinical staff are competent to provide quality care for everyone, every time and are all practising to an agreed level. Definition of Competence A definition of competence was agreed by clinical leaders in May 2013 and is detailed below: “A set of specific and detailed outcomes that need to be achieved in order to a) prove immediate competence in essential skills or b) aid personal and professional development in desirable skills. The competencies must incorporate knowledge, skill, behaviour and demonstration of how these all equate to personal professional accountability for competent care of the patient” (Barnett 2013). This definition focuses attention on the importance of recognising individual personal responsibility and accountability to deliver high quality care. This means taking appropriate actions following the results of any clinical assessments to ensure the individual needs of the patient are met and this care is delivered with care and compassion. Competency is not about performing the task in hand in a mechanistic way without patient involvement. Responsibilities It is the responsibility of the competency lead to develop the competency statements using the agreed framework, present the competency pack to the competency group for approval, develop and co-ordinate the delivery of the master classes, undertake competency assessments and ensure the outcome is forwarded to Development and Training for recording on Pro4. It is the responsibility of the clinical lead to ensure that they are competent themselves and that their registered staff are competent within their scope of practice. The clinical lead may undertake competence assessments themselves or delegate to Band 6s/Clinical Educators who have been competency assessed and who have also attended a recognised course on assessment. The clinical lead should also monitor compliance by ensuring that the essential competencies are reviewed annually at appraisal. The clinical leads are professionally accountable to the Executive Director of Nursing and Workforce and their relevant professional body. It is the responsibility of the individual professional to ensure that they are competent within their scope of practice and that the essential competencies are reviewed annually at appraisal. They are professionally accountable to the Executive Director of Nursing and Workforce and their relevant professional body. 2 CF /v10/DB/KB/GS2013 The Process of Competency Assessment Clinical Leaders A master class will be timetabled within the monthly clinical lead development day in addition to being accessible electronically via the Intranet. This will provide all the relevant underpinning knowledge needed to inform practice and prepare for the competency assessment. The clinical lead feels prepared for the competency assessment. Add wh Yes No http://intranet/index.asp?record=4457 Contact the relevant competency lead to organise a date for assessment. It is recommended that the assessment takes place within 4-6 weeks of accessing the master class. The outcome of the competency assessment is Green. Contact the relevant competency lead to arrange further input. No The assessor provides feedback to the assessee and assists them to develop an individual self directed learning plan at the time in preparation for the second re-assessment. NB for the 3rd re-assessment refer to box below. Yes The assessor provides feedback to the assessee and completes the assessment documentation. The outcome of the competency assessment will be forwarded to Development & Training within 3 days of the assessment. The clinical lead is now competent to assess their clinical staff. NB If this The assessor provides feedback to the assessee and arranges an individual tutorial led by the Competency Lead, focusing on specific learning needs in preparation for the third re-assessment. NB for a referral refer to the box below. Referral at the third attempt may lead to capability. This will be discussed in confidence with the clinical lead and their line manager. 3 CF /v10/DB/KB/GS2013 The Process of Competency Assessment Registered Practitioners Bands 5 and 6 A master class will be accessible either face to face or electronically. This will provide all the relevant underpinning knowledge needed to inform practice and prepare for the competency assessment. http://intranet/index.asp?record=4457 The registered practitioner feels prepared for the competency assessment. Yes No Contact the relevant competency lead to arrange further input. Contact their clinical lead to organise a date for assessment. It is recommended that the assessment takes place within 4-6 weeks of accessing the master class. The outcome of the competency assessment is Green. No The assessor provides feedback to the assessee and assists them to develop an individual self directed learning plan at the time in preparation for the second re-assessment. NB for the 3rd re-assessment refer to box below. Yes NB If this The assessor provides feedback to the assessee and completes the assessment documentation. The outcome of the competency assessment will be forwarded to Development & Training by the competency assessor within 48 hours of the assessment being undertaken for input onto Pro 4 The assessor provides feedback to the assessee and arranges an individual tutorial focusing on specific learning needs in preparation for the third reassessment. NB for a referral refer to the box below. Referral at the third attempt may lead to capability. This will be discussed in confidence with the registered practitioner and their line manager. 4 CF /v10/DB/KB/GS2013 Name: Role: Band: Assessor Role: Assessor Band: Work Base: Assessor Name: Competency Statement (Core Competencies to be included in all Competency Assessments) Expected Level of Competency Registered practitioners deliver person centred care with sensitivity and compassion respecting the dignity and diversity of patients, relatives, carers, visitors and colleagues During this assessment the practitioner is observed acting with respect, kindness, compassion and sensitivity. Demonstrates consistent person centred care with very good professional conduct/behaviour in line with trust expectations. The practitioner explains how they would enable people to understand the rationale for documentation and therefore give informed consent. The practitioner consistently recognises the significance of confidential information and explains the safe storage of patient information through scenarios. During this assessment the practitioner is able to consistently communicate safely, sensitively and effectively using appropriate methods according to the situation. During the assessment the practitioner is observed practising or is able to explain the standards for documentation applicable to the Trust and their professional body, e.g. legibility, confidentiality, accuracy and contemporaneous with dates, times and signatures. During the assessment the practitioner consistently recognises and works within the limitations of their knowledge, skills and professional boundaries, understanding their responsibility and accountability for their own actions and omissions. During the assessment the practitioner is observed or is able to recognise and respond correctly when people are in vulnerable situations, at risk or in need of support and protection. Registered practitioners gain consent for all interventions per Trust policy and professional body requirements Registered practitioners consistently maintain confidentiality as per Trust policy and professional body requirements Registered practitioners provide accurate and meaningful verbal information in a polite and respectful manner to patients, relatives, visitors and colleagues Registered practitioners complete documentation in accordance with organisational and professional body standards Registered practitioners demonstrate professional accountability and act with a ‘duty of candour’ Registered practitioners demonstrate how to safeguard vulnerable adults and children, and when to raise identified concerns through the appropriate channels Level of Competency Evidenced Signature of Assessor 5 CF /v10/DB/KB/GS2013 Competency Statement Subject Specific Competencies Expected Level of Competency The practitioner uses only approved documentation and is able to list the process for approval All pages contain patient’s name and IW number or addressograph labels and the practitioner is able to explain the rationale for this All entries are dated, timed, signed with designation listed and the name is printed on the first entry and a sound rationale for this is given The practitioner is able to review documentation written by colleagues and provide constructive feedback to them The practitioner is able to discuss the appropriate use of abbreviations A full understanding of the professional responsibility and accountability RNs hold for delegating care to HCAs should be evident The practitioner can demonstrate a full understanding of the professional responsibility and accountability for accurately identifying a patient need/problem, with the patient (where possible) The practitioner demonstrates full completion of a risk assessment and accurately identifies subsequent actions required The practitioner consistently demonstrates detailed completion of a nursing needs assessment The practitioner is able to clearly discuss the goal or outcome of care with the patient (where possible) and clearly document this The practitioner is able to clearly discuss steps in the care plan in order to achieve the patient’s stated goal/outcome of care Real life documentation will be checked to ensure current versions are only in use Level of Competency Evidenced Signature of Assessor Real life documentation will be reviewed to see if this criteria is met Real life documentation will be reviewed to see if this criteria is met Practitioner will be asked to undertake a review of one patient’s documentation and explain the feedback they would provide Real life documentation will be reviewed to see if this criteria is met The practitioner is able to describe the role of the HCA in completing nursing documentation Real life documentation will be reviewed to see if this criteria is met Real life nursing documentation will be reviewed to determine whether there is sufficient detail to look after the patient from the written risk assessment Real life nursing documentation will be reviewed to determine whether there is sufficient detail to look after the patient from the nursing needs assessment A full understanding of the professional responsibility to clearly document patient’s goals. Real life documentation will be reviewed to see if this criteria is met A clear explanation is provided by the RN regarding the care to be provided will be recorded in the patient’s notes 6 CF /v10/DB/KB/GS2013 All information and advice given to the patient/relative/carer is clearly documented, in line with the NMC guidelines A full understanding of the professional responsibility and accountability to evaluate the care provided The practitioner consistently demonstrates sound evaluation and progress reports A clear statement of the patient’s condition is documented at the point of discharge or transfer of care to another clinical area Real life documentation will be reviewed to see if this criteria is met Real life documentation will be reviewed to establish that an evaluation of care had been undertaken Real life nursing documentation will be reviewed to determine whether there is sufficient detail reported to give a full picture of the patient’s current condition. Real life documentation will be reviewed to see if this criteria is met Competency Statement Completing a Care Plan Competencies Expected Level of Competency The practitioner consistently demonstrates detailed completion of care plans associated with the nursing needs identified following assessment using clinical judgement and sound rationales Real life nursing documentation will be reviewed to determine whether there is sufficient detail to look after the patient from the care plans and to determine whether the decision making process is apparent Level of Competency Evidenced Signature of Assessor 7 CF /v10/DB/KB/GS2013 Assessment Outcome – Please sign in relevant box Rating Level Actions Green All essential competencies evidenced Red One or more competencies not evidenced No action required, review annually at appraisal. Revisit any development learning points listed below as recommended by assessor. Clinical practice in relation to the specific competency not evidenced is to be supervised and reassessed within 2 weeks. Assessor Signature and date Initial Assessment Assessor Signature and date 2nd Assessment Assessor Signature and date 3rd Assessment Learning points to revisit following successful competency assessment: Assessor Signature: Registered Practitioner Signature: Date: 8 CF /v10/DB/KB/GS2013 Action Plan for Red Rating to be completed following this assessment if required in preparation for second assessment Agreed plan for practice to be supervised until reassessment undertaken if required Date for Reassessment: Name of Assessor: Registered Practitioner Signature: 9 CF /v10/DB/KB/GS2013 Action Plan for Red Rating to be completed following this assessment if required in preparation for third and final assessment Agreed plan for practice to be supervised until reassessment undertaken if required Date for Reassessment: Name of Assessor: Registered Practitioners Signature: 10 CF /v10/DB/KB/GS2013