Fetal development
advertisement

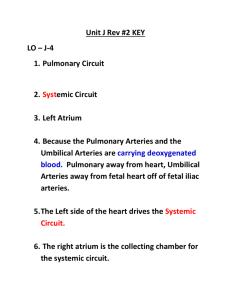
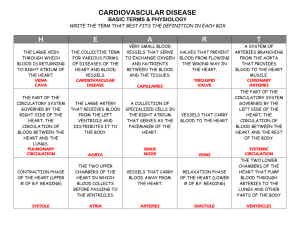
RSPT 2353 – Neonatal/Pediatric Cardiopulmonary Care Fetal Development & Monitoring Lecture Notes Reference & Reading: Czervinske Chapters 1, 2, & 3 I. The duration of human pregnancy can be described in several ways: a. 10 lunar months (4 weeks each) b. 9 calendar months (3 trimesters of 3 months each) c. 40 weeks d. Gestational age refers to time from conception. II. Definition of patient following delivery a. Neonate: delivery – 1st month of life b. Infant: 1 month to 1 year c. Child >1 year of age III. Growth & development is divided into 3 stages: a. Ovum: Development of organism From conception to completion of implantation. (12-14 days) b. Embryo: Major organs develop Extremely vulnerable to effects of radiation, infections, drugs End of ovum stage to approximately 3 cm from head to rump (54-56 days) c. Fetus: End of embryonic period to end of pregnancy Major organs are mostly developed IV. Development of the Pulmonary System – begins at conception and continues into pediatric years. Occurs in 5 stages: a. EMBRYONIC PERIOD: FIRST 2 MONTHS OF GESTATION; DAY 26 – DAY 52 P harynx begins development; earliest development of lungs; lung bud appear like a small pouch Day 26 – pouch has grown & branching into R & L lung buds Lobar bronchi forming; Mesoderm differentiates into muscle, tissue & vessels Diaphragm begins development and is complete by the end of 7 weeks. b. PSEUDOGLANDULAR PERIOD – DAY 52 - 16 WEEKS Week 7 – epiglottis is present; arytenoids tissues begin developing & become opening of airway; membrane that separates nasal cavity from oropharynx disintegrates @ choana Week 10 – cilica appear; present in peripheral airways by 13 weeks Week 12 – palates are formed Week 13-14 – goblet cells appear Fetal lungs development show significant dichotomy beginning with 4 generations and developing to 25 generations by week 16 c. CANALICULAR PERIOD – 17 – 28 weeks Terminal and respiratory bronchioles multiply Week 17-26 - Large amount of vascularization Formation of alveolar ducts Week 20 – 22 - Type I and II alveolar cells differentiate 1. Type I forms alveolar capillary membrane 2. Type II produce pulmonary surfactant Capillaries are present @ 20-21 weeks, doesn’t allow gasexchange until 24-25 weeks d. SACCULAR – WEEK 29-36 SACCULES - smooth walled & cylindrical Subdivide and become alveoli Alveoli detected at 32 weeks; present at 36 weeks e. ALVEOLAR PERIODS – WEEK 36 - TERM Alveoli are formed & continues to form until approx. age 8 Number varies from 20 to 150 million With increasing number of Type II alveolar cells, pulmonary surfactant is produced V. Surfactant a. Type II pneumocyte responsible for surfactant production b. Lower surface tension in the alveolar wall c. Prevent alveoli fro collapsing d. Composed of phospholipids, neutral lipids, & proteins e. In early stage (immature surfactant) production can be easily affected f. Mature surfactant present around week 35 VI. Fetal Lung fluid a. Functions Maintain patency of developing airways Plays a role in formation, size and shape of potential air spaces b. Fluid must be evacuated from lungs at birth 1/3 is removed by “the squeeze” Remaining is absorbed by pulmonary lymphatic system shortly before birth VII. DEVELOPMENT OF CARDIOVASCULAR SYSTEM – the heart is the first major organ to develop a. Early embryologic development Formation begins around day 21 or 3rd gestational week End or 3rd week – two tubes are formed and form a single, continuous chamber Week 5-6 – heart begins to beat Sinus venosus – horns that eventually become inferior and superior vena cava, and part of R atrium Truncus arteriosus grows from primitive ventricle; develops into pulmonary artery and aorta b. Cardiac Chambers Next the heart forms into an “S” shape Divides into R & L ventricles Blood beings to flow through sinus venosus and out truncus arteriosus R & L atrium are formed with the growth of tissue call the septum primum c. Major vessels & cardiac valves Pulmonary aretery & aorta are formed by the separation of the truncus arteriosus Valves form during this time Heart is formed at the end of 2 months (early in week 8) VIII. Fetal circulation – Because of the involvement of the placenta as well as a series of different shunts and pressures found in the fetal circulatory system, there is different way the blood circulates & pressures normally found in the adult are reversed. a. Why? 1. There is a high resistance from the pulmonary vasculature 2. Presence of the placenta offers little resistance to blood flow b. Fetal Circulation (fig 2-5) 1. Fetal Blood receives O2 & nutrients from PLACENTA 2. Collects in progressively larger vessels until it is in UMBILICAL VEIN 3. Umbilical vein carries blood to fetus through umbilical cord 4. Blood flow returns to placenta via umbilical arteries c. DUCTUS VENOSUS Continuation of the umbilical vein into the INFERIOR VENA CAVA Fist shunt encountered Blood mixes with venous blood and enters R ATRIUM d. FORAMEN OVALE 2nd shunt met Opening between R & L atrium Pressure in R ATRIUM is usually higher, shunts into L ATRIUM There is a flap that acts like a one-way valve on the L side of foramen ovale e. DUCTUS ARTERIOSUS 3rd shunt met Located where pulmonary arteries branch & connect to aorta Because of high pressures in lungs blood in PULMONARY ARTERIES is shunted to AORTA Leaves 10% of blood circulating through lungs, enough for developing lungs f. Blood flow after the heart After aorta blood travels to UPPER EXTREMITIES, KIDNEYS, GUT & ABD ORGANS In upper pelvic region, aorta splits into iliac arteries and further to internal & external iliac arteries Internal arteries is where the UMBILICAL ARTERIES branch returns to PLACENTA IX. Other important intrauterine structures a. Placenta Vital connection between fetus & mother Exchange of blood occurs b. Umbilical Cord Lifeline between mother & fetus 3 vessels – 2 arteries, 1 vein Surrounded by Wharton’s jelly c. Amnion Sac that surrounds fetus Enlarges as embryo grows