Development and bioreactor culture of collagen
advertisement

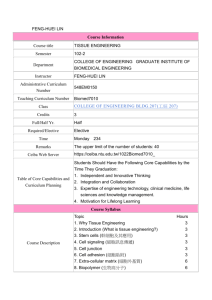
Development and bioreactor culture of collagen-hydroxyapatite scaffolds for bone tissue engineering Niamh A. Plunkett1,2, John P. Gleeson1,2, Michael J. Jaasma1,2, Fergal J. O’Brien1,2 1. Department of Anatomy, Royal College of Surgeons in Ireland, Dublin. 2. Trinity Centre for Bioengineering, Trinity College, Dublin. Abstract Tissue engineering provides an alternative solution for bone graft substitution to the standard, problematic treatments of autografts and allografts. Using a lyophilisation process, this study has developed a scaffold for bone tissue engineering from the two primary constituents of bone, collagen and hydroxyapatite (HA). Four scaffold variants were produced using increasing amounts of HA. The resulting scaffolds were highly porous (over 99%), permeable, supported cell growth and exhibited mineralisation after 28 days in culture. The scaffold with the highest percentage of HA present was chosen as the most promising for bone tissue engineering and was seeded with pre-osteoblastic cells and cultured in a flow perfusion bioreactor developed in our laboratory to enhance cell distribution and mechanically stimulate the cells. Bioreactor culture was found to enhance cell distribution in comparison to statically cultured constructs. The results demonstrate that using the bioreactor in combination with the novel scaffold may provide a promising strategy for bone tissue engineering. Introduction Limitations with autografts and allografts, the most commonly used grafts in bone replacement, include expense, limited size of obtainable graft, donor site morbidity, potential for rejection and complications arising from infection and chronic pain [1]. Due to these problems, interest in alternatives such as tissue engineering solutions has increased. Bone tissue engineering involves seeding bone cells onto a scaffold, culturing this construct so that mineralisation occurs (by using signalling mechanisms such as growth factors or bioreactors) and then implanting it into a defect site in the body [2]. The scaffold must provide a framework and yet have an open-pored structure that allows nutrients to penetrate into the scaffold in vitro and then vascularisation to occur in vivo. A pore volume fraction (porosity) of over 90% is desirable in order for cells to be viable in the construct [3; 4]. Another important parameter, permeability, depends on a number of factors, including porosity, pore size/distribution and pore interconnectivity [3] and governs how easy it is for nutrient delivery to and waste removal from the centre of the construct to occur. This then governs whether the scaffold is a suitable environment for cells to live in and grow. Here, composite scaffolds are presented that are fabricated from collagen and HA, the major constituents of bone. The aim in combining a polymeric material (collagen) and a ceramic one (HA) in a composite material is to combine the advantages of both materials, while overcoming any drawbacks they may have. Thus, the polymer imparts flexibility to the scaffold while the ceramic provides a reinforcing effect. The fabrication process (lyophilisation) used is highly effective in composite material fabrication, as well as being highly controllable and enabling highly porous, homogeneous scaffolds to be produced [5]. A major setback to bone tissue engineering has been the inability to develop homogeneous tissue engineered constructs in static culture. Bioreactors can be used to overcome this problem. Flow perfusion bioreactors force fluid through constructs, thus delivering nutrients to the centre of constructs, where necrotic regions occur, and exerting a shear stress on the cells which can mechanically stimulate them. A flow perfusion bioreactor has been designed and validated in our laboratory [6]. Use of this bioreactor has shown that rest periods of 7 hours between bouts of stimulation allow cells to restore their mechanosensitivity so that they can respond again to flow [7] and that short term rest periods of the order of seconds are also useful in restoring mechanosensitivity. The goals of this study were to develop and characterise collagen– hydroxyapaptite (CHA) scaffolds for use in bone tissue engineering and to use the optimal scaffold in the flow perfusion bioreactor in an effort to enhance cell distribution and mechanically stimulate the cells on the construct. Materials and Methods Scaffold fabrication and analysis: Type I bovine collagen (Collagen Matrix, USA) was blended with HA (Plasma Biotal, UK) in acetic acid to form slurries. CHA scaffolds were fabricated by freezedrying these slurries over 24 hours using a final freezing temperature of -40°C [5; 8]. Four different scaffolds were produced: (i) control collagen-only scaffolds (0% HA) (ii) 50wt%HA scaffolds (2:1 ratio of collagen to HA) (iii) 100wt%HA scaffolds (1:1 ratio) and (iv) 200wt%HA scaffolds (1:2 ratio). Scaffolds were crosslinked via dehydrothermal crosslinking in a vacuum oven at 120°C and 0.05 Bar for 24 hours. Scaffold discs (12.7 mm in diameter) were further crosslinked using EDC/NHS (14 mM N-(3-Dimethylaminopropyl)-N’ethylcarbodiimide hydrochloride and 5.5 mM N-Hydroxysuccinimide in distilled water; Sigma-Aldrich, Germany) [9]. Porosity was examined by measuring the density of the dry scaffold samples and comparing this to the density of the materials from which the scaffolds were fabricated. The permeability of scaffold samples was obtained by using a permeability rig designed and fabricated in-house. 12.7 mm diameter samples were placed into the rig under a column of water which was allowed to flow through the samples for 5 minutes. Darcy’s law was then used to obtain the permeability as follows: k Qh AP where k is the hydraulic permeability in m 4 / Ns , Q is the volume flow rate in m 3 / s , h is the height of the scaffold, A is the cross sectional area of the flow path and P is the pressure exerted by the column of water. A sample size of at least five per scaffold type was used. The Young’s modulus in compression of the scaffolds was obtained using a mechanical testing machine (Z050, Zwick/Roell, Germany) fitted with a 5-N load cell. Testing was carried out in a bath of PBS at a strain rate of 10% per minute to a maximum strain of 10%. The modulus was defined as the slope of a linear fit to the stress-strain curve over 2-5% strain [10]. A sample size of at least 10 per scaffold type was used. Scaffolds were seeded with 2 million MC3T3 E1 cells and cultured for 7, 14, 21 or 28 days. A sample size of 4 per scaffold type per time point was used. Cell number was quantified using Hoechst 33258 (SigmaAldrich, Germany). Cell distribution was examined by wax embedding scaffold samples, slicing at 10µm on a mictotome (Leica Microsystems, Germany), staining using haematoxylin and eosin and examining under a light microscope (Nikon, Japan). Mineralisation was examined by staining using alizarin red s and quantified using cetylpyridinium chloride (Sigma-Aldrich, Germany) [11]. Bioreactor culture: The 200wt%HA scaffold which proved to have the best osteogenic potential (see Results) was seeded with 2 million MC3T3 E1 cells, and cultured for 6 days. Subsequently, scaffolds were either cultured statically for a further 169 hours (Static group) or placed in the flow perfusion bioreactor. The flow perfusion bioreactor designed and validated in our laboratory consists of a programmable syringe pump (New Era Pump Systems Inc., USA), a scaffold chamber and a reservoir [6]. The constituent parts are connected via silicone tubing. This provides a closed circuit in which media can be circulated (Figure 1). 6 scaffold chambers were used in each experiment and each experiment was run at least twice to ensure repeatability. Of the groups placed into the bioreactor, two were controls and two experienced flow. The two controls were (i) a Timeless group which was placed into the bioreactor and then immediately removed, to assess the effect this process had and (ii) a Control-169 group which remained in the bioreactor for 169 hours but did not experience flow. Each flow group used 1 hour of stimulation followed by a resting period of no flow for 7 hours, with this pattern being looped for the entire culture period of 169 hours. The two flow groups were (i) a Steady group which experienced flow at 1mL/min for the stimulation period (ii) a Rest-Inserted group in which short-term periods of no flow of duration 5 seconds were incorporated after each 10 seconds of 1mL/min flow in the stimulation period, as this can restore mechanosensitivity to desensitised cells. Cell number and cell distribution were examined as above. Statistical analysis was done in Minitab 15 (Minitab Inc., USA) using general linear model ANOVA and the Tukey test as the post-hoc test. A Media Reservoir Scaffold Chamber Syringe Pump Figure 1. Diagram of flow perfusion bioreactor. ‘A’ shows one of the 6 systems that make up the bioreactor [6]. ‘B’ shows a closer view of a scaffold chamber. Results Scaffold fabrication and analysis: Porosity values ranged from 99.5% ±0.03% for the control collagenonly scaffolds to 99.0% ±0.06% for the 200wt%HA scaffolds. Permeability values increased with increasing HA content, to a maximum of 4.8 x10-9 m4/Ns ±1.5 x10-9 m4/Ns for 200wt%HA scaffolds. The Young’s modulus also increased significantly with HA content, with the 200wt%HA scaffold having a compressive modulus of 3 kPa ±1.6 kPa compared to the collagen-only scaffold’s modulus of 1.6kPa ±1 kPa (p<0.00005). Cells were viable on all scaffolds at 28 days, with all CHA groups showing an increase in cell number over the culture period of 10-48% while the control collagen-only group experienced a slight reduction in cell number of 13% (Figure 2). 50wt%HA scaffolds showed low initial cell attachment but good proliferation of cells. Mineralisation occurred at the surface of all scaffolds by day 28 (p=0.0137), with quantifiably more mineralisation occurring on the 200wt%HA scaffold group than any other group (p<0.0021). * Cell number (million) 4 * 3.5 3 c 7 day 14 day 21 day 28 day c 2.5 2 1.5 1 0.5 0 collagenonly 50wt%HA 100wt%HA 200wt%HA Figure 2. Cell number on the four scaffold types over a 28 day culture period. Average cell number increased on all CHA scaffolds over the culture period, while it decreased on the collagen-only group (these changes were not statistically significant). All groups had higher cell number than the 50wt%HA group (* represents p<0.0016), although this group experienced the greatest amount of proliferation over the culture period. Bioreactor culture: A trend for cell number reduction due to bioreactor culture was noted but was found to be non-significant and a substantial number of cells were retained on the constructs after the culture period (Figure 3, p=0.081). 1.3 – 1.4 million cells were attached to the flow group constructs after 169 hours of bioreactor culture, a large proportion (65-70%) of the amount initially seeded. Cell distribution was enhanced due to flow, as can be seen in the images in Figure 4. The static group exhibited a cellular distribution that was predominantly on the periphery of the construct, while in the flow groups the cells were dispersed in a homogeneous manner throughout the construct. Cell number (millions) 4.5 4 3.5 3 2.5 2 1.5 1 0.5 0 timeless static control-169 steady rest-inserted Figure 3. Cell number on groups used in the bioreactor study. No significant difference was found between groups, but there was a trend for bioreactor cultured groups to have a lower cell number compared to the static culture groups (p=0.081). Static Rest-Inserted Figure 4. Images of haematoxylin and eosin stained longitudinal sections of a static group construct (on left) and a rest-inserted group construct (on right). Cells reside predominantly on the periphery of the static group constructs while they are dispersed homogeneously throughout the flow group constructs. Scale bars are 200µm in length. Discussion This study has led to the development of patented, novel composite scaffolds with significant potential for bone repair and, furthermore, has shown that use of a flow perfusion bioreactor improves cellular penetration into the scaffolds. The CHA scaffold and the process for its production was submitted to the European Patent Office (EPO) in February 2008 and published internationally under the Patent Cooperation Treaty (PCT) in August 2008 [8]. Inclusion of HA in the scaffolds increases scaffold stiffness and permeability while retaining the very high porosity, and significant advantageous properties, of collagenonly scaffolds. The fabrication technique (lyophilisation) utilised offers a large degree of architectural control, providing scaffolds which should meet all of the criteria of an osteoconductive scaffold. High porosity is important to enable cell infiltration into the scaffold, and a high permeability allows for better nutrient exchange and waste removal from the scaffold. The permeability of trabecular bone is reported as being from 10-6 to 10-12 m4/Ns and the scaffold permeability lies midway within this wide range, which is a very promising result [12]. The scaffolds are highly biocompatible, showing an ability to support cell growth to 28 days in static culture, with modest cell number increases being noted on all CHA scaffolds. In addition, mineralisation of the scaffolds occurred by day 28, with significantly more mineral deposition on the 200wt%HA constructs than on any other group. This ability to enable mineralisation to occur demonstrates the osteogenic potential of the CHA scaffold, a potential which is vital for its use in bone tissue engineering. The 200wt%HA scaffold exhibited a high porosity of 99%, the highest permeability of the scaffold types tested and the highest compressive stiffness, thus pinpointing it as the most promising scaffold from a structural perspective. Furthermore, the biocompatibility of the 200wt%HA scaffold was similar to the highly biocompatible collagen scaffold and its mineralising ability surpassed all other scaffold types tested. Due to this promising combination of structural and osteogenic properties, the 200wt%HA scaffold was chosen for use in further experimentation in a flow perfusion bioreactor. Use of the bioreactor in conjunction with this novel scaffold has enabled better cell distribution throughout the scaffold to be obtained. While constructs cultured statically exhibited a cellular distribution where cells resided predominantly on the periphery of the construct, flow group constructs that had been cultured in the bioreactor for 169 hours displayed a much more homogeneous distribution of cells throughout the construct. Despite a trend for decreasing cell number due to bioreactor culture, use of a bioreactor is vitally important for improving the homogeneity of tissue engineered constructs and thus overcoming a major setback to tissue engineering and moving closer to the goal of developing a successful tissue-engineered construct for use as a bone graft substitute. Acknowledgements Irish Research Council for Science, Engineering and Technology SFI President of Ireland Young Researcher Award Enterprise Ireland References [1] Perry, C. R. Clin Orthop Relat Res: 71-86, 1999. [2] Plunkett, N. A. and F. J. O'Brien Technol Health Care: In Submission, 2008. [3] Harley, B. A. (2006). Cell-Matrix Interactions: Collagen-GAG Scaffold Fabrication, Characterization, and Measurement of Cell Migratory and Contractile Behavior via Confocal Microscopy. [4] Rezwan, K., Q. Z. Chen, J. J. Blaker, et al. Biomaterials 27: 3413-31, 2006. [5] O'Brien, F. J., B. A. Harley, I. V. Yannas, et al. Biomaterials 25: 1077-86, 2004. [6] Jaasma, M. J., N. A. Plunkett and F. J. O'Brien J Biotechnol 133: 490-6, 2008. [7] Jaasma, M. J. and F. J. O'Brien Tissue Eng Part A 14: 1213-23, 2008. [8] O'Brien, F. J., J. Gleeson and N. A. Plunkett (2008) WO 2008/096334 A2 [9] Lee, C. R., A. J. Grodzinsky and M. Spector Biomaterials 22: 3145-54, 2001. [10] Haugh, M. G., M. J. Jaasma and F. J. O'Brien J Biomed Mater Res A, 2008. [11] Venugopal, J., S. Low, A. T. Choon, et al. J Mater Sci Mater Med 19: 2039-46, 2008. [12] Sander, E. A. and E. A. Nauman Crit Rev Biomed Eng 31: 1-26, 2003.