notes on cyclophosphamide therapy
advertisement

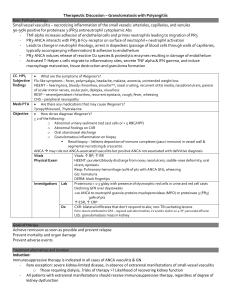
APPENDIX 5 NOTES ON CYCLOPHOSPHAMIDE THERAPY Cyclophosphamide therapy is probably the most toxic of the routinely prescribed immunosuppressive agents. The provision of cyclophosphamide should be in accordance with locally approved protocols and prescribing guidelines. Intravenous cyclophosphamide therapy should only be delivered by practitioners appropriately trained in managing extravasations of chemotherapeutic drugs. These short notes are designed to provide an overview of cyclophosphamide therapy in the context of inflammatory interstitial lung disease, most commonly in association with connective tissue disease or vasculitis and often in combination with corticosteroid treatment. Cyclophosphamide therapy is not recommended for the treatment of idiopathic pulmonary fibrosis. Dose and Mode of Delivery Oral cyclophosphamide is usually given at a dose of up to 2mg/kg/day, with a lower dose in those over 60 years and those with renal impairment. The length of treatment with oral cyclophosphamide is dependent upon the underlying disease and the response. In clinical trials of systemic sclerosis-associated ILD, oral therapy has been continued for up to 1 year1. Intravenous cyclophosphamide therapy is increasingly favoured over oral therapy due to a significantly better side-effect profile2. Pulsed intravenous treatment is usually given at a dose of 500-750mg/m2 with adjustments for age and renal function. The dose interval and duration of treatment is dependent upon the nature of the underlying inflammatory disease. Studies of intravenous cyclophosphamide in systemic sclerosis associated ILD have generally adopted a 3-4-weekly regimen over at least 6 months35. This regimen exposes the patient to the drug for a prolonged period but results in a lower cumulative dose than would be achieved with oral cyclophosphamide. Side effects and monitoring Nausea, vomiting and reversible hair loss are common side effects. Bone marrow suppression is the most common serious side-effect and regular full blood count monitoring is mandatory. The white blood cell nadir usually occurs 10-14 days after an intravenous pulse. Prophylactic cotrimoxazole therapy to prevent Pneumocystis jiroveci pneumonia has been shown to be cost effective in patients with Wegener’s granulamatosis 6, but there are no equivalent studies in patients with interstitial lung disease treated with cyclophosphamide. Haemorrhagic cystitis and bladder cancer are uncommon but serious sideeffects of cyclophosphamide therapy. The incidence of bladder cancer, after first exposure to cyclophosphamide and a cumulative dose of 100g, is estimated to be 5% at 10 years and 16% at 15 years7. The risk of bladder complications is reduced by: 1) co-administration of sodium 2-mercaptoethanesulfonate (Mesna), a regional detoxicant of active cyclophosphamide metabolites 2) good hydration 3) treatment in the early morning to avoid overnight bladder accumulation. Individuals receiving cumulative doses of cyclophosphamide exceeding 20g should have 3-6 monthly urinalyses, to detect microscopic haematuria, for up to 11 years after cessation of the drug8. Reduced and potentially irreversible infertility in male and females treated with cyclophosphamide is an important consideration. Counselling and support from local fertility services is mandatory in appropriate cases. REFERENCES 1) Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, Arriola E, Silver R, Strange C, Bolster M, et al., for the Scleroderma Lung Study Research Group Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med 2006;354:2655–2666. 2) Haubitz M, Schellong S, Göbel U, Schurek HJ, Schaumann D, Koch KM, Brunkhorst R. Intravenous pulse administration of cyclophosphamide versus daily oral treatment in patients with antineutrophil cytoplasmic antibody-associated vasculitis and renal involvement: a prospective, randomized study. Arthritis Rheum. 1998;41:1835-44. 3) Hoyles RK, Ellis RW, Wellsbury J, Lees B, Newlands P, Goh NS, Roberts C, Desai S, Herrick AL, McHugh NJ, et al. A multicenter, prospective, randomized, doubleblind, placebo-controlled trial of corticosteroids and intravenous cyclophosphamide followed by oral azathioprine for the treatment of pulmonary fibrosis in scleroderma. Arthritis Rheum. 2006;54:3962–3970. 4) Airò P, Danieli E, Rossi M, Frassi M, Cavazzana I, Scarsi M, Grottolo A, Franceschini F, Zambruni A. Intravenous cyclophosphamide for interstitial lung disease associated to systemic sclerosis: results with an 18-month long protocol including a maintenance phase. Clin Exp Rheumatol. 2007;25:293-6 5) Yiannopoulos G, Pastromas V, Antonopoulos I, Katsiberis G, Kalliolias G, Liossis SN, Andonopoulos AP. Combination of intravenous pulses of cyclophosphamide and methylprednizolone in patients with systemic sclerosis and interstitial lung disease. Rheumatol Int. 2007;27:357-61 6) Chung JB, Armstrong K, Schwartz JS, Albert D. Cost-effectiveness of prophylaxis against Pneumocystis carinii pneumonia in patients with Wegner's granulomatosis undergoing immunosuppressive therapy. Arthritis Rheum. 2000;43:1841-8 7) Vlaovic, P. and M. A. Jewett. Cyclophosphamide-induced bladder cancer. Can.J Urol. 1999;6:745-748. 8) Talar-Williams C, Hijazi YM, Walther MM, Linehan WM, Hallahan CW, Lubensky I, Kerr GS, Hoffman GS, Fauci AS, Sneller MC. Cyclophosphamide-induced cystitis and bladder cancer in patients with Wegener granulomatosis. Ann Intern Med. 1996;124:477-84