Surgery Examination Checklists
advertisement

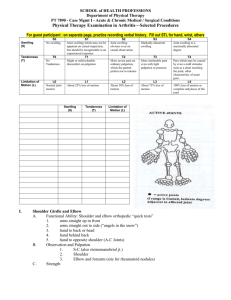
Surgery Examination Checklists Lump / Swelling Introduction, Consent, exposure, position I. Inspection 1. Site: measured from bony prominence 2. Size: measure length, width, depth 3. Shape: globular, pear-shaped, irregular, kidney-shaped, pedunculated 4. Overlying skin: texture, color, punctum, edematous, veins, previous scars 5. Discharge: color, composition 6. Movements: cough, breathing, swallowing, tongue protrusion II. Palpation 1. Temperature: back of fingers, compare to opposite & local area 2. Tenderness: check face of patient 3. Edge/ margin: index finger; distinct, indistinct, erosions, slip sign (lipoma) 4. Surface: smooth, nodular, lobular, matted, variable 5. Consistency: see table 6. Fluctuation: fix swelling then check in 2 perpendicular planes (pg.55-56) 7. Transillumination: + à clear fluid; use torch & rolled xray film at opposite end 8. Reducibility: disappears completely on appropriate pressure; hernia 9. Compressibility: becomes smaller but immediately comes back to original on release; vascular 10. Pulsatility: expansile - 2 fingers raise & separate; transmitted - raised but not separated 11. Fixity: TO SKIN – pinch skin; TO MUSCLE – contract skin (check size, mobility); TO VESSELS/NERVES – fixed in one plane (longitudinal); TO BONE – absolute fixation III. Percussion 1. Fluid thrill: only in large swellings (similar to abdominal) 2. Resonance: percussion IV. Auscultation – bruit V. Local tissues i. Lymph nodes (regional) ii. Arteries: pulses iii. Nerves: sensations, paresis, wasting iv. Bones & joints: active & passive movements IV. General examination: respiratory, cardiac, skeletal, abdomen Consistency Stony/ Bony hard Not indentable Malignant, Chondroma, osteoma Firm/ rubbery Like nose, rubber ball Fibroma, neurofibroma Soft/ spongy Like lips, very squashable, resilient Lipoma, cystic Very soft/ soft Like jelly, squashable, no resilience Brilliantly transillumination: 1. Ranula 2. Cystic hygroma 3. Lymph cyst 4. Hydrocele (male & female) 5. Epididymal cyst 6. Meningocele Thyroid Introduction, Consent, Position: sitting on stool Exposure: nipples and above is ideal I. Inspection: 1. Site, Size (measure), Shape 2. Skin, dilated veins, scar marks, discharging area 3. Movements: swallowing saliva, tongue protrusion 4. Pemberton’s sign: raise both arms above shoulder touching ears, 3 mins * Dilated veins, cyanosis, puffy face, respiratory distress à retrosternal extension +ve II. Palpation from front: 1. temperature 2. tenderness 3. tracheal position III. Palpation from back: “Layhee’s method” – stabilize w/ one hand, palpate with other 1. Movement with swallowing 2. Surface: smooth, diffuse, nodular 3. Consistency: a. If soft: do fluctuation & transillumination 4. Extent, margins 5. Mobility/ fixity: contract SCM, overlying skin pinch 6. Kocher’s Test: compress both lobes posteromedially * Stridor à tracheal compression due to weakened tracheal rings 7. Carotid pulse palpation: Berry’s sign +ve if no pulse 8. Lymph nodes: supraclavicular & cervical 9. Can check for exophthalmos while behind IV. Percussion: for retrosternal extension * Always from below à upwards (resonant à dull) V. Auscultation: 1. Carotid arteries: ask pt to stop breathing, check for bruit 2. Chest: crackles at base (pul. edema), pleural effusion 3. Heart: S3, murmurs, A.fib? VI. Eye signs: 1. Exophthalmos 2. Chemosis 3. Lid retraction 4. Lid lag 5. Ophthalmoplegia & Accommodation: check all movements VII. General Physical: 1. Hands: i. Hot, dry or moist ii. Pulse: iii. Fine tremor: use pen on outstretched hands, (not paper) 2. Pretibial myxedema: dusty pink, blotchy elevation due to mucopolysaccharide deposition 3. Proximal myopathy: both upper & lower 4. Reflexes: * Hypothyroid: relaxation component delayed * Hyperthyroid: brisk Venous System Introduction, Consent, Position: initially standing, later supine Exposure: umbilicus to feet & genitalia exposure (pampiniform plexus) I. Inspection (standing) – both limbs, front & back 1. Visible veins / varicosities: site & size – Long saphenous vein: medial, extends to thigh – Short saphenous vein: posterior & lateral, extends to popliteal – Communicating veins – Varicocele – Saphena varix 2. Swelling: localized, diffuse (edema or DVT) 3. Skin changes: gaiter’s zone – Color, Pigmentation – Lipodermatosclerosis – Ulcer: Extent, size, shape, floor, margin, edge, discharge, surrounding area 4. Deformity of limb: equinus (planter flexion due to short Achilles tendon) II. Palpation (standing) 1. Temperature, tenderness 2. Texture & skin changes; bone thickening (periostitis) – Ulcer: tenderness, induration, warmth, mobility, fixity 3. Fascial defects (crescenteric gaps) – Fegan’s test 4. Trunks of long and short saphenous veins 5. Schwartz test: tap lower vein à feel impulse above – Signifies: continuous column of blood, all valves incompetent III. Palpation (supine) 1. Morrissey’s Cough impulse: lie down, elevate leg, empty vein – Pt coughs à feel fluid thrill with finger below SFJ = saphena varix 2. Trendelenburg Test: * Elevate limb & milk veins à Tourniquet just below SFJ à Pt stands quickly (saphenofemoral junction: 2.5 cm below & lateral to pubic tubercle) * I: release tourniquet à filling from above = SF incompetence * II: DON’T release tourniquet, wait 1 min à filling from below = perforator incompetence 3. Short Saphenous Tourniquet test: – Same as above but just apply tourniquet at lower boundary of popliteal fossa 4. Multiple Tourniquet test: to find site of incompetent perforators – Elevate limb, milk veins, apply 3-4 tourniquets: i. Just below SFJ ii. Above Knee iii. Below knee iv. Above ankle – Stand, release tourniquets from BELOW -> UPWARDS – b/w i & ii à adductor canal perforator – b/w ii & iii à below knee perforator – b/w iii & iv à lower leg perforator (5, 10, 15 cm from medial malleolus) 5. Tests for DVT: do cautiously – Perthe’s test: tourniquet, pt walks; painful = DVT – Homan’s test: DORSIFLEXION of foot à pain in calf – Mose’s sign: squeeze calf muscles à pain – Neuhof’s sign: thickening & tenderness of calf on deep palpation IV. Auscultation: bruit over prominent veins à AVM V. Other: 1. Peripheral pulses 2. Regional lymph nodes 3. Ankle joint movements 4. Abdomen: compressive mass – gravid uterus, tumor, ascites, abdominal lymphadenopathy Arterial System Introduction, Consent, Position: supine Exposure: full limbs, not genitalia; ensure warm room I. Inspection: compare both limbs side-by-side 1. Limb deformity 2. Color change: pallor, cyanosis, gangrenous – Elevation pallor, dependency rubor 3. Skin: thin, shiny, loss of s/c fat & hair, brittle nails, pressure areas 4. Edema: inflammation, congestion 5. Superficial veins: pale, guttered (collapsed) 6. Muscle wasting: measure from bony prominence 7. Gangrene: Dry vs. wet, extent, discharge, color, odor – Line of demarcation: band of hyperaemia; well defined in dry but unclear in wet 8. Ulceration: site, size, extent, shape, discharge, floor, surrounding area; pressure ulcer, patchy ulcer II. Palpation: compare both sides 1. Temperature: extent of cold area 2. Tenderness: along vessel line - thrombosis 3. Crepitus: in gangrenous area 4. Capillary refill 5. Allen’s test: patency of radial & ulnar arteries 6. Buerger’s postural test: i. supine, raise leg 2 mins, watch for level pallor develops in foot sole · Buerger’s angle: < 30’ = severe ischemia · Ischemic height: ht cm = mmHg arterial pressure in foot ii. Put leg below bed, time taken to become pink * Capillary filling time: > 30 sec = severe ischemia * Reactive vasodilation: first turns blue then pink 7. Lower limb pulses: i. Dorsalis pedis: lateral to extensor hallucis longus tendon ii. Posterior tibial: against calcaneum, behind medial malleolus iii. Anterior tibial: above ankle joint, lateral to extensor hallucis longus tendon iv. Popliteal: knee flexed 130’, lower fossa v. Femoral: below midpoint of inguinal ligament, slight hip flexion 8. Upper limb pulses: i. Radial: lateral wrist; check radio-radio delay & radio-femoral delay ii. Ulnar: medial wrist iii. Brachial: medial to biceps brachii tendon, at elbow iv. Axillary: lateral axilla, against upper humerus shaft 9. Head/Neck pulses: i. Subclavian: supraclavicular fossa, shrugging shoulders ii. Common carotid: medial to SCM at thyroid cartilage level iii. Facial: distal to angle of mandible iv. Superficial temporal: in front of ear tragus III. Auscultation: 1. with bell for bruit over carotids, aorta, femoral 2. heart sounds IV. Blood pressure V. Neurological & lymph node examination Breast History: swelling, pain, nipple discharge, changes in nipple, asymmetry, trauma hx, lymph node swellings, metastasis – respiratory, abdominal pain, loss of appetite, bone pain, neurological symptoms, convulsions; past history of cancers or breast lumps; family history of cancers; risk factors in history like OCPs, early menarche, late menopause, menstrual cycles Introduction, Consent, privacy, chaperone Position: initially sitting, then 45’ lying down Exposure: until waist/ umbilicus, both breasts I. Inspection: compare both with arms at side and with arms above head 1. Chest symmetry of breasts and nipples 2. Nipple: number, displacement, retraction, discharge and color, cracks, inverted 3. Areola: cracks, fissure, paget’s disease 4. Skin: peau d’orange (block of dermal lymphatics), dimpling (cooper’s ligaments), dilated veins (phyllodes), Mondor’s disease (superficial thrombophlebities 5. Tell patient to LIFT breast and look underneath for scar marks 6. Obvious swelling: – quadrant site, size, extent, shape, margin, surface 7. Axilla & supraclavicular fossa: any obvious swelling II. Palpation: lying at 45’ with arm behind head ** always start with normal breast and area, palmar fingers, hand flat 1. Temperature 2. Tenderness 3. Palpate all four quadrants and axillary tail of normal breast first and then abnormal 4. Nipple & areola: tenderness, press for discharge & use tissue * Examination of specific swelling: 5. Extent, surface, margins 6. Consistency 7. Fluctuation & transillumination à cystic swelling 8. Fixity: 1. Skin fixation: pull up skin with thumb and fingers 2. Skin tethering (cooper’s ligaments involved) à stretch skin over and check dimpling 3. Within breast tissue: press breast and move lump, fibroadenoma is mouse and moves 4. With Pectoralis major: sitting up * Tell pt to put hands on waist lightly à check fixity parallel and perpendicular * Tell pt to press strongly down (flexion of shoulder) à check fixity parallel - if fixed parallel to fibers à T3 5. With Lattisimus dorsi: sitting up * Tell pt to extend shoulder and flex elbow at 90’ à check fixity of lump 6. With serratus anterior: sitting up * Tell pt to push against your shoulder à check fixity of lump - if fixed à fixity to chest wall à T4 7. With chest wall (intercostal and ribs): sitting up * Tell pt to lift arms à check fixity of lump 9. Axillary & cervical lymph nodes: * for patient’s left hand, use your left hand and rest patient’s arm on your own arm * make sure you do both sides 1. Anterior group: in anterior axillary fold (posterior to pec major) 2. Central group: 3. Posterior group: posterior axillary fold (anterior to subscapularis) 4. Apical group: press up in axilla 5. Lateral group: press against inside of humerus 6. Supraclavicular nodes 7. Deltopectoral nodes? 8. Cervical nodes 10. Lymphedema of arms / venous system? III. General physical: 1. Respiratory system (posterior chest) 2. While posterior is exposed, check for sacral edema and any spine lesions 3. Abdominal examination in supine position: a. Palpable liver, shifting dullness, fluid thrill b. DREs Inguinal Hernia Hernia: entire or part of viscus protruding through the wall that contains it Indirect: - Incomplete: bubonocele (in inguinal canal but not through the superficial ring) funicular (until upper part of testis) - Complete (to the bottom of the scrotum) Introduction Consent: privacy of patient with a chaperone Exposure: umbilicus to mid-thigh Position: initially standing straight, later lying down I. Inspection (standing) 1. Site 2. Size + extent: incomplete vs. complete 3. Shape: pyriform – indirect, globular – direct 4. Skin: veins, scars, redness, discoloration, strangulated skin 5. Expansile impulse with cough à diagnostic for hernia 6. Visible peristalsis à enterocele II. Palpation (standing first) 1. Temp 2. Tender 3. ** Get above the swelling or not à differentiates scrotal or inguinoscrotal swelling 4. Consistency: enteroceleà soft, elastic ; omentacele à doughy 5. Location of swelling: * Pubic tubercle found by contracting ADDUCTOR LONGUS and tracing tendon * Above and medial to the pubic tubercle à inguinal hernia * Below and lateral to the pubic tubercle à femoral hernia 6. Palpation of testes, epididymis, spermatic cord a. Both SIDES b. Find relation of swelling to testes! c. TRANSILLUMINATION if necessary, fluctuation etc 7. Reducibility: * Tell patient to lie down à reduces spontaneously or with patient’s own maneuvers * Taxis: flexion, adduction and rotation of hip joint -> relaxes the supf inguinal ring & oblique abdominal muscles 8. Coughing expansile: * Put fingers on superficial ring (1.25 cm above pubic tubercle) while he is lying down * Tell patient to stand up and cough à check if it comes through the superficial ring à INGUINAL HERNIA 9. Deep ring occlusion test: * Tell patient to lie down and again reduce swelling * Occlude the deep ring (1.25 cm above midpoint of inguinal ligament) while he is lying * Tell patient to stand up and cough o if the swelling appears à positive test à DIRECT o if the swelling does not appear à negative à INDIRECT III. Percussion: Omentocele à dull ; enterocele à resonant IV. Auscultation à enterocele bowel sounds V. Check for causes: 1. Bulbar urethra * Lift scrotum and palpate thickening or button-like depression à stricture of urethra 2. Abdominal examination * ** Abdominal muscle tone by telling patient to lift head à check for MALGAIGNE BULGING!! * Scars, acites, masses 3. Digital rectal examination à prostate, strictures 4. Respiratory examination à COPD, chronic disease etc.