Bones can be described on the basis of their overall macroscopic
advertisement

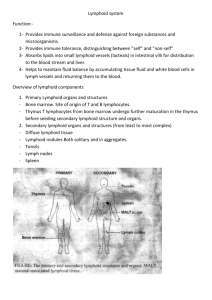
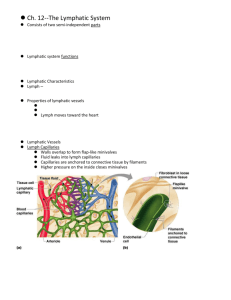
BIOL 2304 Lymphatic and Immune Systems The Lymphatic System Functions: Transport excess interstitial fluid back to bloodstream Transport dietary lipids Contain lymphocytes that filter and cleanse lymph Generate an immune response Components: Lymphocytes, Lymph nodes, Lymphatic vessels Lymphoid follicles in GI tract (Peyer's patches, tonsils) Other accessory organs: spleen, thymus, bone marrow Orders Of Lymphatic Vessels Lymph capillaries – smallest lymph vessels, first to receive lymph Lymphatic collecting vessels – collect from lymph capillaries Lymph nodes – scattered along collecting vessels Lymph trunks – collect lymph from collecting vessels Lymph ducts – empty into veins of the neck Lymphatic Capillaries Located near blood capillaries Receive tissue fluid from CT Minivalve flaps open and allow fluid to enter Highly permeability and low pressure allows entrance of ECF, bacteria, viruses, and cancer cells Lymphatic Capillaries Lacteals – specialized lymphatic capillaries Specialized lymphatic capillaries located in the villi of the small intestine Receive large digested fats Chyle – milky bodily fluid within lacteals made of a mixture of lymph and lipoproteins called chylomicrons Lymphatic Collecting Vessels Accompany blood vessels and nerves as neurovascular bundle Composed of the same three tunics as blood vessels: intima, media, externa Contain more valves than veins do Prevents backflow of lymph Lymphatics have zero blood pressure Lymph is propelled by: Contraction of skeletal muscles Pulse pressure of nearby arteries Tunica media (smooth muscle) of the lymph vessels Lymph Nodes Cleanse the lymph of pathogens ~500 lymph nodes in human body Lymph nodes are organized in clusters Microscopic Anatomy of a Lymph Node Fibrous capsule – surrounds lymph node Trabeculae – connective tissue strands formed from capsule Lymph vessels: Afferent lymphatic vessels Efferent lymphatic vessels Lymph sinuses – regions within node containing network of reticular fibers on which immobile phagocytes and lymphocytes await passing pathogens Subcapsular, cortical, and medullary sinuses Lymph Trunks Lymphatic collecting vessels converge into trunks Five major lymph trunk types: Lumbar trunks (paired) Receives lymph from lower limbs Intestinal trunk (unpaired) Receives chyle from digestive organs Bronchomediastinal trunks (paired) Collects lymph from thoracic viscera Subclavian trunks (paired) Receive lymph from upper limbs and thoracic wall Jugular trunks (paired) Drain lymph from the head and neck Lymph Ducts Cisterna chyli – a dilated sac located at the union of lumbar and intestinal trunks Thoracic duct – ascends along vertebral bodies Drains 3/4th of the body Empties into left brachiocephalic vein between the left subclavian and left internal jugular veins Right lymphatic duct – Drains 1/4th of the body Empties into right internal jugular vein and right subclavian veins The Immune System Reconnaissance, Recognition, and Response Components: Immune cells, lymphoid tissue, and lymphoid organs Functions of Immune Cells: Detect invader/foreign cells Communicate alarm & recruit immune cells Suppress or destroy invader Two major kinds of defense: Innate immunity – inborn, no exposure to antigen required Acquired immunity – develops after exposure to antigen Review of Blood Cells Erythrocytes (red blood cells) Thrombocytes (platelets) – anuclear cell fragments; essential for blood clotting Leukocytes (white blood cells) Granulocytes – Presence of granules in their cytoplasm Neutrophil: 50-70% of WBC; most common WBC; phagocytic; first response inflammation Eosinophil: <5% of WBC; fight parasites Basophil: <1% of WBC; release histamines (vasodilator) and heparin (anticoagulant) Agranulocytes – (aka lymphoid cells) Absence of granules in their cytoplasm Lymphocytes: 25-35% of WBC T-lymphocytes (T cells): fight virus-infected cells and cancer cells B-lymphocytes (B cells): produce & secrete antibodies Natural Killer Cells (NK cells): fight virus-infected cells and cancer cells Monocytes: 3-9% of WBC; largest of the leukocytes Leave the blood stream (diapedesis) to become macrophages Primary Lymphocytes T Lymphocytes: Helper T lymphocytes Alert other leukocytes of presence of pathogens Cytotoxic T lymphocytes Attack foreign cells directly B Lymphocytes: Become plasma cells and secrete antibodies Lymphocytes – B and T cells Different Types of T cells Cytotoxic T cells – attack foreign cells Helper T cells – activate other T cells and B cells Suppressor T cells – inhibit the activation of T and B cells Memory T cells – dormant T cells that are activated at second exposure to antigen T cell membranes contain CD markers: CD3 markers present on all T cells CD8 markers on cytotoxic and suppressor T cells CD4 markers on helper T cells Different Types of B cells Plasma cells – activated B cells that secrete antibodies Memory B cells – dormant B cells that are activated at second exposure to antigen Lymphocyte Formation B and T cells originate in bone marrow B cells remain in bone marrow for maturation T cells leave bone marrow, and migrate to thymus gland for maturation Lymphocyte Activation All lymphocytes originate in bone marrow B lymphocytes remain in bone marrow for maturation T lymphocytes leave bone marrow, and migrate to thymus gland for maturation Lymphocytes provide Acquired Immunity: Specificity – activated by and responds to a specific antigen Versatility – is ready to confront any antigen at any time Memory – “remembers” any antigen it has encountered Tolerance – responds to foreign substances but ignores normal tissues Immunocompetence – the body’s ability to produce a normal immune response following exposure to an antigen Lymphocyte Activation Activating T or B cells produce: Effector lymphocytes – short-lived, active, attack immediately Memory lymphocytes – dormant until body encounters same antigen again Basis of acquired immunity Guard against subsequent infections Lymphoid Tissue Lymphoid tissue – specialized connective tissue in which vast quantities of lymphocytes gather to fight invading microorganiss Two general types based on location: Mucosa-associated lymphoid tissue (MALT) - mucous membranes of digestive, urinary, respiratory, and reproductive tracts Found within all lymphoid organs except thymus Lymphoid follicles (nodules) – Spherical clusters of densely packed lymphocytes; not surrounded by a fibrous capsule; found scattered in lymphoid tissue Lymphoid Organs Primary lymphoid organs Bone marrow Thymus Secondary lymphoid organs Lymph nodes Spleen Tonsils Aggregated lymphoid follicles (nodules) in small intestine and appendix Thymus Immature lymphocytes develop into T lymphocytes Most active in childhood Functional tissue atrophies with age Composed of cortex and medulla Medulla contains Hassall’s corpuscles (thymic corpuscles) Differs from other lymphoid organs Functions strictly in T lymphocyte maturation Arises from epithelial tissue Lymph nodes Lymph nodes Lymph percolates through lymph sinuses Sinuses filled with network of reticular fibers containing phagocytes Most antigenic challenges occur in lymph nodes Spleen Largest lymphoid organ Two main blood-cleansing functions Removal of blood-borne antigens Removal and destruction of old or defective blood cells Storage of platelets White pulp Thick sleeves of lymphoid tissue Provides the immune function of the spleen Red pulp - surrounds white pulp, composed of: Venous sinuses – filled with whole blood Splenic cords – reticular CT rich in macrophages Also the site of hematopoiesis in the fetus Tonsils Simplest lymphoid organs Four groups of tonsils Palatine, lingual, pharyngeal and tubal tonsils Arranged in a ring to gather and remove pathogens Underlying lamina propria consists of MALT Aggregated Lymphoid Nodules And Appendix MALT – mucosa-associated lymphoid tissue Abundant in walls of intestines Fight invading bacteria Generate a wide variety of memory lymphocytes Aggregated lymphoid nodules (Peyer’s patches) Located in the distal part of the small intestine Appendix – tubular offshoot of the cecum