Sexual Health Services by Community Pharmacists
advertisement

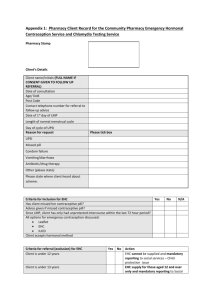
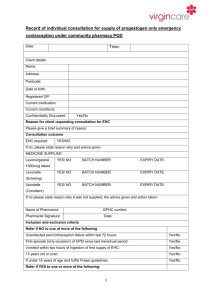
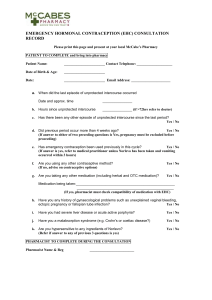
Providing a Sexual Health Service Goal To explore the roles that community pharmacy can play in providing a comprehensive sexual health service to women of child bearing age. Objectives After studying this module pharmacists should be able to: Describe how community pharmacists can provide contraception, advice and screening for Chlamydia Explain how pharmacy based sexual health services can contribute to reducing the incidence of unwanted pregnancy with specific reference to unwanted teenage pregnancy Understand the principles of providing for a sexual health service by community pharmacists. Prepare an action plan for premises, staff and systems needed to introduce (or revise) a sexual health service Self- Assess your learning needs: What additional skills, facilities and equipment would I need to initiate oral contraception in my community pharmacy? Is this a service that my PCT would want to commission? What is the current service provision for sexual health services in my PCT? What training would I need to provide to my staff to support this service? How comfortable would I feel discussing all types of contraception? CPD Competencies - this module supports the following pharmacy competencies: Competence Where the module supports competence development C1a Assessing the medication needs of patients C1c Reviewing medication with patients C1f Providing advice and counseling, C1i Generating and maintaining records of medication supplied to patients This module provides information on the assessments required to ensure that a patient would receive the most appropriate contraception In order to identify difficulties and potential risk e.g. concordance issues, adverse effects, changing medication needs The module focuses on the information that should be provided by the pharmacist to a patient to ensure that the patient knows how to take their medication. The module provides information of the records required for the service to be provided and information that would be required by a PCT for audit purposes. Background In the Western World the UK has the highest teenage pregnancy rate compared to the rest of Europe and the USA has the highest rates of teenage pregnancy. It is ten years since Our Healthier Nation made teenage pregnancy a priority and target for health authorities with high teenage conception rates (Department of Health 1998) The Social Exclusion Report 1999 set targets for local authorities to halve teenage pregnancy rates by the year 2010 and to establish a downward trend in the under 16 rate. This is coupled with the strategy to increase the proportion of teenage parents in education, training or employment to 60% by 2010 and hence reduce their risk of long-term social exclusion. All local areas have a 10 year strategy in place with local under 18s conception rate reduction targets of between 40-60%. These local targets underpin the national target of 50%. Reduction in teenage pregnancy is sometimes seen as a political issue however there are important adverse effects on both health and social as aspects (see Box 1). Box 1 – Health and social consequences of teenage pregnancy Children of teenage mothers have higher rates of infant mortality than children born to older mothers, They are more likely to be born premature – which has serious implications for the baby’s long-term health – and have higher rates of admissions to A&E. In the longer term, children of teenage mothers experience lower educational attainment and are at higher risk of economic inactivity as adults; The pressures of early parenthood result in teenage mothers experiencing high rates of poor emotional health and well-being – which impacts on their children’s behaviour and achievement; They often do not achieve the qualifications they need to progress into further education and, in some cases, have difficulties finding childcare and other support they need to participate in Education, Employment or Training (EET). Consequently, they struggle to compete in an increasingly high-skill labour market. Teenage mothers and young fathers disproportionately come from disadvantaged backgrounds and would, therefore, be more likely to need additional support to make a successful transition to adulthood, becoming a teenage parent adds significantly to the challenges they face. It is estimated that three quarters of under-18 conceptions are unplanned and around a half end in abortion. It is important, therefore, that there is a strong focus on preventing teenage pregnancies. Steady progress has been made on reducing the under-18 conception rate, which has fallen by 11.8% (based on 2005 data) since 1998, to its lowest level for over 20 years. Within this overall reduction in conceptions, the rate of births has fallen by almost 19%, whilst the rate of abortions has fallen by almost 3%. This means that we are reducing the proportions of young women who experience early parenthood and the poor outcomes associated with it. (Source DOH Teenage Parents Next Steps: Guidance for Local Authorities and Primary Care Trusts 2007.) Introduction Community pharmacists across the country have made a significant contribution to the access and provision of Emergency Hormonal Contraception (EHC) and contributed to the provision of screening for sexually transmitted diseases. Prior to these services being introduced there was some scepticism about whether the pharmacy was a suitable place to provide EHC. However not only are pharmacy based EHC services regarded as highly successful but there is now recognition of the significant contribution that can be made to the further development of contraceptive services by allowing pharmacists to provide regular hormonal contraception. In December 2007 in a statement to the House of Lords the Parliamentary UnderSecretary of State, Department of Health, Lord Darzi stated that ‘we recognise that pharmacies could play an increased role in the provision of contraception and other sexual-health services because of their accessibility and convenient opening hours. We will work with primary care trusts over the next year to pilot the supply of contraception, including the contraceptive pill, through NHS arrangements. We will also work with the pharmacy profession to ensure robust standard-setting and appropriate training so that pharmacists are competent to provide this service.’ The Pharmacy White Paper is a consultation document which is seeking the views of the public, patients and consumers, the NHS and healthcare professionals to feed into developing a primary and community care strategy due this summer. The White Paper acknowledges the input that community pharmacists have already provided in sexual healthcare. In particular pharmacists role in the provision of EHC and Chlamydia screening. An independent evaluation of a pilot Chlamydia screening service available across London since November 2005 has shown that 87% of young people reported that they would recommend the service. Based on this evaluation the Government intends to publish a national template to support Primary Care Trusts (PCTs) commissioning of Chlamydia screening from community pharmacies as part of the National Chlamydia Screening Programme. (Source: Department of Health ‘Pharmacy in England, Building on Strengths – delivering the future. April 2008) This module is able to draw on the experience of the pilot project developed by Manchester Primary Care Trust for the provision of a Sexual Health Service including a Patient Group Direction (PGD) by community pharmacists. The Manchester service is the first in the UK in which pharmacists are initiating oral contraception and thus provides a model for future services. We anticipate that other primary care organisations will want to commission this service in the future and this module aims to give readers an understanding of what is involved. The Manchester project involves accredited community pharmacists providing advice, supply and follow up to women who wish to access a family planning service. The pharmacists are able to supply either condoms or a hormonal method of contraception (combined oral contraceptive pill or progesterone only pill) or to offer advice and possible referral to other agencies where appropriate. In addition the project allows the pharmacist to access the Chlamydia Screening programme for women under 25 years of age or for any women who wish to access the service should the need arise. The project also allows the pharmacist to test and treat a woman (and her partner if appropriate) presenting with a positive result for Chlamydia under PGD. See the article on page x for further information on Chlamydia services in community pharmacy. The purpose of the new service is two-fold. To give women greater choice and flexibility in accessing services, and to reduce teenage conception rates. Commissioning of pharmacy based sexual health services Community pharmacists in Manchester have supplied Emergency Hormonal Contraception (EHC) under a Patient Group Direction since 1999. Many primary care organisations now commission this as an enhanced service under the pharmacy contract and Manchester does so. The local scheme has been very successful with over 150,000 women accessing the service over the 8 years. Any pharmacy based sexual health service will be commissioned based on the local needs identified. The Manchester Teenage Pregnancy Partnership (MTPP) published a report which identified 17 of wards across the city where the rate of teenage pregnancy and termination was higher than 60 per 1000 women. In addition due to the high student population of the city a further ward was included in the pharmacy service to address the needs of the student population resident during the academic year. These areas of greatest need were to be targeted through the new pharmacy service. Community pharmacists already experienced in providing the existing Emergency Hormonal Contraception (EHC) scheme under PGD were invited to become providers of the new service and received training to become accredited to do so. Practice Points: 1. Consider if your pharmacy would be identified in such a population area and whether to approach your PCT 2. Do you already provide EHC under PGD? This is an important consideration because you will have already undergone role play activities as part of your accreditation. Also the experience gained providing consultations for an EHC PGD service is invaluable. Service Delivery In order to provide this service there are a number of factors to be taken into consideration: premises, access, staff, equipment, the consultation, (including medical history) records/paperwork, training and service audit. Each of these will now be considered in turn. Premises Since the launch of the Pharmacy Contract in 2005, most community pharmacies now have a consultation room. This is an essential element for the sexual health service due to the length of a consultation. The average time for an EHC consultation using a PGD is approximately 10-15 minutes. The new service needs a longer period for the initial consultation. In addition the service will require storage of confidential paperwork and some equipment (see below). (Practice point- how would you manage your consultations for a contraception service in respect of other services that you may be providing such as MURs or observed supervised consumption?) Access to the Service Part of the consultation process for the Manchester EHC service requires the pharmacist to discuss future contraception. This is one access point for the new contraceptive service. There are other methods to encourage women to access the service which should be explored, for example: emergency supplies of oral contraceptives current contraceptive service provision, which may be poor in your area current contraceptive service provision which is not easily accessible the local GP practice may not have the capacity to provide this service. Your local surgery may wish to refer women directly to you. one advantage of the community pharmacy service is the longer opening hours including weekends. Staff As for any new prospective service your pharmacy staff should be consulted on this service being provided. You will need to consider how the staff will deal with the approach by women wanting to access the service and how this information is relayed to you in the dispensary. You should consider how the service would be available during sickness and holiday periods. In addition to the counter and dispensary staff the locum workforce must be consulted. The pharmacy may use a regular locum or agency staff and these staff should be able to access the required training. (Practice point - how would you approach your regular locum/s to engage them with this service?) Consideration should be given to the length of time for a consultation. If the pharmacy is busy at certain times then you may wish to direct staff to operate an appointments system and how that will be managed e.g. would you issue appointment cards? Equipment In order to safely decide on whether to supply oral contraception the pharmacist is expected to undertake a number of health checks which requires the following equipment to be available: BP monitor Weighing scales BMI chart Height chart Paperwork (Practice point – do you have agreements to have pharmacy equipment serviced regularly?) The PCT may provide this equipment for you or you may have to purchase this separately. The Consultation As stated above it may be difficult to determine the length of a consultation but you should allow yourself at least 30 minutes to complete all of the necessary checks and patient history. It is also dependant on how the client accessed the service e.g. via an EHC consultation or perhaps referral from another healthcare professional . Another important factor to consider is whether this is a first supply of hormonal contraception or a repeat supply. The Manchester scheme uses the same protocol for the supply of a POP or a COC contraceptive but has a different protocol for the initial and repeat supplies. The crucial difference between the protocols is to establish where the first supply of contraceptive was initiated and how long ago since the supply. If the supply has been within the 12months from the pharmacy then the repeat procedure would be followed. However if the supply was longer than 12 months then the pharmacist is advised to use the first issue protocol to ensure the client receives the most appropriate advice and care. If the client has accessed contraception from another agency in the past the pharmacist is responsible for ensuring that all the appropriate checks and advice has been undertaken during the pharmacy consultation. Medical History The most important aspect of this service is taking an accurate medical history from the client. This history together with the measurements that are undertaken will inform the decision about the type of contraception that should be considered. A guide to the consultation is provided below based on the Manchester service: 1. Client history Name Date of birth Address GP including practice details Ethnicity 2. Sexual History Ist day of the last period Inclusion and Exclusion Criteria Inclusion Criteria Have other methods of contraception been discussed including Long Acting Reversible Contraception (LARCS)? Does the client have regular periods? Was the last period normal? If less than 16 years of age - Does client meet Fraser Guidelines? Is the client competent to consent to treatment? 3. Exclusion Criteria Does the client have a known intolerance to oestrogen or progestogens? Is the client pregnant? Does the client have any unexplained vaginal bleeding? Does the client have active liver disease, cholestatic jaundice or a history of jaundice in pregnancy? Is there a history of migraine? Has the client had recent trophoblastic disease?* (this question could be asked as ‘are you undergoing any treatment for a complication of a previous pregnancy?) Does the client have heart disease or history of stroke? Does the client have malabsorption syndrome? (this question could be asked as ‘are you aware of that you have any condition such as coeliac disease or other condition that might affect you being able to absorb certain foods?) Does the client have cancer or history of breast cancer? Is the client receiving concomitant medication which interacts with oestrogen or progestogen? * Trophoblastic disease is an uncommon complication of pregnancy where there is an abnormal overgrowth of all or part of the placenta causing a condition called a ‘molar pregnancy’. It is detected by a rapid rise in the levels of Human Chorionic Gonadotrophin (hCG). It is recommended that a woman should not use either oral contraceptives or an IUD during treatment or for some time after to ensure that the levels of hCG do not rise and lead to confusion. Women are normally registered with regional centres for on-going treatment. . 4. Lifestyle Information BP If BP >140/90 = POP (Progestogen only pill) (i.e. COC would not be considered appropriate for this patient) Weight (Kg) Height (cms) BMI If BMI >35 = POP Smoking Status If >35 years & smokes=POP NB If client is an ex-smoker the date when given up should be recorded including the average number of cigarettes smoked per day. If it vies less than one year since the client has given up then the client should be treated as a smoker and counselled that that the most appropriate form of hormonal contraception is a POP. 5. Deciding which form of contraception is appropriate All of the above information should be collected prior to a discussion about the different forms of contraception available. The answers to the above questions would inform the clinical decision as to which form of hormonal contraception (if any) would be suitable for this client. You would then need to consider specific exclusion criteria for the combined oral contraceptive (COC) pill. (Practice point: what do you think would need to be considered?) a. Exclusion Criteria specific to a COC form of contraception Is the client less than six week's post partum or breast feeding? Does the client have complicated diabetes e.g. nephropathy, retinopathy or neuropathy? Is there a history of transient ischaemic attack? Is there a family history of venous thromboembolism (VTE), myocardial infarction (MI) or cerebrovascular accident (CVA) in first degree relative <45 years Is there a history of systemic lupus erythematosus (SLE) or lupus anticoagulant? Is there a history of acute porphyria? Does the client have current or past VTE or clotting tendency? Is there a known presence of gallstones? Is there a history of long term immobility? Is client suitable for COC? If YES proceed to Counselling section. (Practice point: if the answer was no – what would be your next course of action?) b. POP Exclusion criteria Does the client have a current VTE or acute porphyria? NB if YES is answered to this question the client should be referred to Family planning or GP Is client suitable for POP? If YES proceed to Counselling section. If the client is not suitable for either form of hormonal contraception this should be documented and the client referred to another healthcare professional. (Practice point- think about how you would deliver this information to a client) you should be aware of other forms of contraception because the client may be asking for further guidance. If the client is suitable for one of the hormonal methods of contraception you should provide the following counselling which must be documented every time. Counselling Efficacy Mode of action Effect on menstrual cycle/bleeding Risk and side effects, breast tenderness, headache, VTE risk Starting regime Vomiting and diarrhoea- and what action to take Enzyme inducing medication Missed pill advice Safer sex guidance Smoking/Alcohol advice Action if side effects or concerns Discussion of emergency contraception Contraception leaflet given Condoms given Follow-up appointment You should stock and be able to supply a range of literature that is available to help with counselling such as the DH leaflet on the different forms of contraception and literature on sexually transmitted diseases. (Practice point- do you already stock this information? If not do you know where to obtain supplies? The local PCT may be able to provide advice and support for this) Records and Paperwork The PCT would in all probability provide the necessary paperwork for audit purposes. However you may need to consider what information you should record in order to provide the appropriate advice and supply. In addition to the information recorded during history taking and counselling the following information should be recorded by the pharmacist to complete the consultation: Brand of contraception provided (you should be confident that you have supplied all of the relevant information for the client to make an informed choice) Batch number and expiry date Prescription length e.g. 3 or 6 months Date of review The PCT may require that information regarding the supply is supplied to the client’s regular GP. However patient consent must be obtained before this can occur. The client and pharmacist should sign and date the paperwork to complete the audit trail. (Practice point- how would you approach a refusal by a client for this information to be supplied to the GP?) An audit form should be completed for the PCT and all documentation stored following Caldicott Principles preferably in alphabetical order. (Practice point: think about the different brands of COC and POPs available. Are you confident to be able to explain about each one? Remember a client may have used a particular brand before so you must check what, if any, hormonal contraception has been used before. Also the PCT may specify which brands are to be supplied) Training In order to be commissioned to provide the Manchester service community pharmacists must fulfil the following criteria: Accredited to provide EHC Undergo further training and accreditation for the new service Undergo Enhanced Criminal Record Checks Working in wards identified in the Manchester Teenage Pregnancy Partnership as areas with high teenage pregnancy levels. Prepared to commit to providing the service at the pharmacy for a period of time. Be working in a pharmacy which has a consultation room of the standard required for accreditation under the advanced service of the pharmacy contract. The pharmacists will receive additional training delivered by a consultant in sexual health or similarly qualified clinician such as a GP with Special Interest in Sexual Health. The supply of hormonal contraception is made under a PGD. The training includes: 1) The PGDs for the different types of contraceptive pills i.e. Combined Oral Contraceptive (COC) , Progestogen Only Pill (POP) 2) Chlamydia testing and the PGDs for Chlamydia treatment which include azithromycin, doxycline and erythromycin 3) Inclusion and exclusion criteria 4) Referral pathways 5) Paperwork 6) Child protection 7) Education in Sexually Transmitted Infections (STIs) 8) How to complete the relevant health checks- i.e. height, weight, calculation of BMI and BP 9) Role play exercises 10) Multiple Choice Questions In order to reduce the paperwork Manchester PCT provided the pharmacists with a CD ROM of the relevant research papers and guidance and each pharmacy with a copy of the publication, ‘Family Planning: A Global Handbook for Providers 2007’ A WHO Family Planning Cornerstone publication. Service Audit The Manchester service will be evaluated by the PCT after 6 months and is collecting the following information for audit purposes: o o o o o o o o o o Number of women who have accessed the service Age Postcode Method of accessing the service Type of contraception supplied Length of consultation Number of women who have been referred to other services Number of women who fall outside the protocol Number of women who are receiving contraception for the first time Number of women who are receiving repeat contraception Post payment verification checks are to be carried out 6 months after the service has commenced together with a patient satisfaction survey of the service. Experience to date in Manchester The Manchester scheme is a pilot project and the 6 months evaluation will take into account the audit information together with advice and recommendations from the pharmacists providing the service. The intention is for the pharmacist to use the paperwork provided by the PCT for 6 months, then re-evaluate to ensure that all the necessary information has been recorded and to determine the length of time taken for each consultation. The service in Manchester used the expertise of some of the most experienced pharmacists already providing the EHC service. If the new service was to be provided by a primary care organisation which did not have such a wealth of experience then consideration should be given to the following: Providing training in conducting consultations for contraception Role play exercises Attendance at a family planning clinic to gain experience of the service. At present most women accessing the new service do so via a request for EHC. As community pharmacists become more familiar with the project it is expected that the uptake of women accessing the service will increase. Reflective activities What are the targets for your PCT in reducing the teenage pregnancy rate? Where would you find this information? What training would you provide to your staff in order to promote this service and ensure that women are dealt with sensitively? Multiple Choice Questions. 1. The combined oral contraceptive pill a. Increases the risk of breast cancer T/F b. Decreases the risk of breast cancer T/F c. Increases the risk of ovarian cancer T/F d. Increase the risk of endometrial cancer T/F 2. Chlamydia is an infection which a. has higher rates in women taking oral contraception T/F b. should be treated with azithromycin as a first line treatment T/F c. has symptoms at the onset of infection T/F d. is more common in women over 25 years of age T/F 3. The following contraceptive choices would be appropriate a. A woman who gave up smoking 6 months ago would be suitable for a COC? T/F b. A COC is the most appropriate choice for a woman over 36 years of age with a BMI of 27? T/F c. A POP is suitable for a woman over 29yrs of age who has not had a period for 38 days? T/F d. A COC is more suitable for a woman who works shifts? T/F 4. A woman taking a COC a. Should be warned to take extra precautions when taking amoxicillin for more than 4 weeks T/F b. Should be advised to stop if she is diagnosed with gallbladder disease? T/F c. Can continue with it during major surgery that will cause her to be immobile for more than 1 week T/F d. Is taking the most appropriate form of hormonal contraception with a BP of 145/93 T/F 5. The Progestogen Only Pill a. Is the recommended form of hormonal contraception for women who smoke T/F b. Is suitable for a woman taking rifampicin? T/F c. Can be taken if a woman has migraine headaches with aura T/F d. Can be supplied if a woman has had a VTE in the last 6 months T/F 6. With regard to contraception, pregnancy and breastfeeding a. It takes six months from stopping an oral contraceptive for a woman to become pregnant? T/F b. A woman who is partially breastfeeding does need to use contraception? T/F c. A POP can increase the risk of ectopic pregnancies? T/F d. A woman should stop take a ‘rest’ from COCs after taking them for a long time T/F 7. A woman should a. Does not need her BP to be checked at each supply of contraception T/F b. Be excluded from taking a POP if her mother had a CVA at 44 yrs T/F c. Always be offered a choice of which contraceptive? T/F d. Be advised seek further advice if she has vomiting or diarrhoea for more than 2 days? T/F 8. During the counselling session the following should occur a. A woman should be advised to have an STI screening after each episode of unprotected sex? T/F b. All woman should be offered Chlamydia screening? T/F c. Any type of contraceptive should be started on the fifth day after the period T/F d. Not be supplied with condoms T/F