`The role of nephrectomy following renal transplant failure`
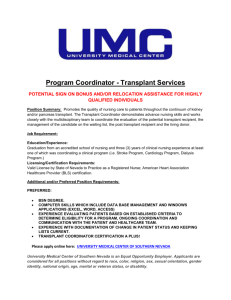
advertisement

P277 TRANSPLANT NEPHRECTOMY FOLLOWING GRAFT FAILURE: WHO GETS IT AND DOES IT MAKE A DIFFERENCE? Thomson, P, Clancy, M, Geddes, C Renal Unit, Western Infirmary, Glasgow INTRODUCTION: Transplant nephrectomy is not routinely conducted following graft failure although is often performed soon after a return to dialysis due to acute illness or later, in the context of a chronic inflammatory illness related to transplant rejection. The aim of this study was to identify the proportion of patients who undergo transplant nephrectomy following a return to dialysis and compare their clinical characteristics and outcomes to those in whom the transplant was left in-situ. METHODS: We identified all patients who attended our renal transplant unit between 01/01/1968 and 01/08/2009, were registered on the unitary electronic patient record (EPR) and were noted to have a failed renal transplant. Baseline clinical, laboratory and demographic data were recorded. These included age, sex, primary renal diagnosis, date of transplant, type of transplant, date of transplant failure, cause of transplant failure and whether transplant nephrectomy was undertaken. Duration of follow-up within the renal unit and subsequent mortality were recorded. Comparison of nephrectomy and non-nephrectomy groups was made by univariate parametric and non-parametric testing with significance level set at <0.05. RESULTS: A total of 774 patients experienced 994 episodes of renal transplant failure between 01/01/1968 and 01/08/2009. 468/774 (60.1%) of patients were male with a mean age at first transplant of 35.9yrs. A total of 919/994 (92.4%) failed transplants were from cadaveric donors whilst 75/994 (7.6%) were from live donors. 384/994 (38.6%) episodes of transplant failure were followed by transplant nephrectomy. 223/384 (58.1%) nephrectomies occurred within 4 weeks of transplant failure with 21/384 (5.5%) occurring >52 weeks after failure. Discounting those patients with transplant nephrectomy within 4 weeks of failure, those who subsequently underwent transplant nephrectomy were found to be similar in age at transplantation (33.4yrs v 33.3yrs, p=0.95), duration of renal transplant (5.1yrs v 4.6yrs, p=0.32), rates of transplant rejection causing failure (42.1% v 36.9%, p=0.26) and rates of mortality (13.4yrs v 14.5yrs, p=0.585) to those in whom the transplant was left in-situ. Transplant nephrectomy was found to occur more commonly in patients with chronic allograft nephropathy (7.1% v 3.3%, p=0.045) and was associated with a greater proportion of patients who had been treated for acute rejection prior to failure (63.6% v 39.5%, p<0.001). Mortality at 28 days post nephrectomy was 1.64%. CONCLUSION: Nearly 40% of patients with a failed renal transplant are likely to undergo transplant nephrectomy. Whilst up to 60% of nephrectomies occur in the first 4 weeks following transplant failure, 40% are undertaken later, at a time when many patients have returned to their parent haemodialysis unit. Those who underwent transplant nephrectomy after 4 weeks from transplant failure were found to share similar baseline clinical characteristics to those whose renal transplant was left in situ. When comparing these groups the presence of treated acute rejection prior to failure and a diagnosis of chronic allograft nephropathy were found to be significantly associated with proceeding to transplant nephrectomy. No difference in overall survival between groups was found.