Questions on Positioning Many graduate nurses are not comfortable
advertisement

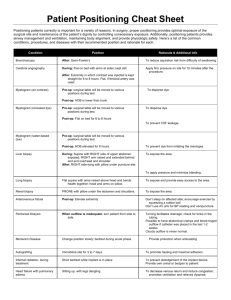
Questions on Positioning Many graduate nurses are not comfortable answering these questions because: • They don’t understand the “whys” of positioning • They don’t know the terminology • They have difficulty imaging the various positions Since many illnesses affect body alignment and mobility, you must be able to safely care for these clients in order to be an effective nurse. Correspondingly, these topics are also important on the NCLEX-RN® exam. The successful test taker must correctly answer questions about impaired mobility and positioning. Immobility occurs when a client is unable to move about freely and independently. To answer questions on positioning, you need to know the hazards of immobility, normal anatomy and physiology, and the terminology for positioning. If you have difficulty answering positioning questions, the following strategy will assist you in selecting the correct answer. Step 1. Decide if the position for the client is designed to prevent something or promote something. Step 2. Identify what it is that you are trying to prevent or promote. Step 3. Think about anatomy, physiology, and pathophysiology. Step 4. Which position best accomplishes what you are trying to prevent or promote? Does this sound a little confusing? Hang in there. Let’s walk through a question using this strategy. Immediately after a percutaneous liver biopsy, the nurse should place the client in which of the following positions? 1. Supine. 2. Right side-lying. 3. Left side-lying. 4. Semi-Fowler’s. Before you read the answers, let’s go through the four steps outlined above. Step 1. By positioning the client after a liver biopsy, are you trying to prevent something or promote something? Answer: You position a client after this procedure to prevent something. Step 2. What are you trying to prevent? Answer: The most serious and important complication after a percutaneous liver biopsy is hemorrhage. How did you know that you are trying to prevent hemorrhage? You accessed what you know about a liver biopsy. Step 3. Think about principles of anatomy, physiology, and pathophysiology. What do you do to prevent hemorrhage? Answer: You apply pressure. Where would you apply pressure? On the liver. Where is the liver? On the right side of the abdomen under the ribs. Step 4. How should the client be positioned to prevent hemorrhage from the liver, which is on the right side of the body? Now look at your answer choices. (1) Supine. If you lay the client flat on his back, no pressure will be applied to the right side. Eliminate. (2) Right side-lying. If you lay the client in a right side-lying position, will pressure be applied to the right side? Yes. Keep it in for consideration. (3) Left side-lying. No pressure is applied to the right side. Eliminate. (4) Semi-Fowler’s. If you lay the client on his back with head partially elevated, no pressure is applied to the right side. Eliminate. The correct answer is (2). Some students select (3) because they don’t know normal anatomy and physiology. Some students select (4) because semi-Fowler’s position is used for a lot of reasons. Things to Remember • Even if you didn’t memorize what position to use before, during, and after a procedure, think about the question for a moment. You can figure out what position is needed. • You cannot figure out the correct position if you do not know what the terms mean (supine, Trendelenburg, Fowler’s). • You cannot figure out a correct position if you do not know anatomy and physiology. If you think the liver is on the left side of the body, you are in trouble! • You cannot figure out a correct position if you do not know what you are trying to accomplish. If you couldn’t remember that a complication after a liver biopsy is hemorrhage, your best hope of selecting the correct answer would be to throw a dart. • To those students who think in images, you should form a mental image of each position. Picture yourself placing the client in each position, and then see if the position makes sense. Essential Positions to Know for the NCLEX-RN® Exam Position Therapeutic Function Flat (supine) Avoids hip flexion, which can compress arterial flow. Dorsal recumbent Supine with knees flexed; more comfort- able. Side lateral Allows drainage of oral secretions. Side with leg bent (Sims’s) Allows drainage of oral secretions; decreases abdominal tension. Head elevated (Fowler’s) Increases venous return; allows maximal lung expansion. High Fowler’s: 60 to 90 degrees Fowler’s: 45 to 60 degrees Semi-Fowler’s: 30 to 45 degrees Low Fowler’s: 15 to 30 degrees Feet and legs elevated Increases blood return to heart; relieves pressure on lumbrosacral area. Feet elevated and head Used to insert CVP line, or for treatment lowered (Trendelenburg’s) of umbilical cord compression. Feet elevated 20 degrees, Increases venous return; used for shock.knees straight, trunk flat,and head slightly elevated(modified Trendelenburg’s) Elevation of extremity Increases venous return. Increases blood volume to extremity. Flat on back, thighs flexed, Increases vaginal opening for legs abducted (lithotomy) examination. Prone Promotes extension of hip joint. Not well tolerated by persons with respiratory or cardiovascular difficulties. Knee-chest Provides maximal visualization of rectal area Positioning Facts: 1. Air/Pulmonary Embolism (S&S: chest pain, difficulty breathing, tachycardia, pale/cyanotic, sense of impending doom) --> turn pt to left side and lower the head of the bed. 2. Woman in Labor w/ Un-reassuring FHR (late decels, decreased variability, fetal bradycardia, etc) --> turn on left side (and give O2, stop Pitocin, increase IV fluids) 3. Tube Feeding w/ Decreased LOC --> position pt on right side (promotes emptying of the stomach) with the HOB elevated (to prevent aspiration) 4. During Epidural Puncture --> side-lying 5. After Lumbar Puncture (and also oil-based Myelogram)--> pt lies in flat supine (to prevent headache and leaking of CSF) 6. Pt w/ Heat Stroke --> lie flat w/ legs elevated 7. During Continuous Bladder Irrigation (CBI) --> catheter is taped to thigh so leg should be kept straight. No other positioning restrictions. 8. After Myringotomy --> position on side of affected ear after surgery (allows drainage of secretions) 9. After Cataract Surgery --> pt will sleep on unaffected side with a night shield for 1-4 weeks. 10. After Thyroidectomy --> low or semi-Fowler's, support head, neck and shoulders. 11. Infant w/ Spina Bifida --> position prone (on abdomen) so that sac does not rupture 12. Buck's Traction (skin traction) --> elevate foot of bed for counter-traction 13. After Total Hip Replacement --> don't sleep on operated side, don't flex hip more than 45-60 degrees, don't elevate HOB more than 45 degrees. Maintain hip abduction by separating thighs with pillows. 14. Prolapsed Cord --> knee-chest position or Trendelenburg 15. Infant w/ Cleft Lip --> position on back or in infant seat to prevent trauma to suture line. While feeding, hold in upright position. 16. To Prevent Dumping Syndrome (post-operative ulcer/stomach surgeries) --> eat in reclining position, lie down after meals for 20-30 minutes (also restrict fluids during meals, low CHO and fiber diet, small frequent meals) 17. Above Knee Amputation --> elevate for first 24 hours on pillow, position prone daily to provide for hip extension. 18. Below Knee Amputation --> foot of bed elevated for first 24 hours, position prone daily to provide for hip extension. 19. Detached Retina --> area of detachment should be in the dependent position 20. Administration of Enema --> position pt in left side-lying (Sim's) with knee flexed 21. After Supratentorial Surgery (incision behind hairline) --> elevate HOB 30-45 degrees 22. After Infratentorial Surgery (incision at nape of neck)--> position pt flat and lateral on either side. 23. During Internal Radiation --> on bedrest while implant in place 24. Autonomic Dysreflexia/Hyperreflexia (S&S: pounding headache, profuse sweating, nasal congestion, goose flesh, bradycardia, hypertension) --> place client in sitting position (elevate HOB) first before any other implementation. 25. Shock --> bedrest with extremities elevated 20 degrees, knees straight, head slightly elevated (modified Trendelenburg) 26. Head Injury --> elevate HOB 30 degrees to decrease intracranial pressure